After suffering a stroke—perhaps a blood clot gets lodged in the brain or a blood vessel near the brain bursts—a person may suddenly not be able to hear, talk, or see. He or she might have trouble walking or exhibit a speech impediment. In fact, one of the greatest challenges of treating patients affected by stroke is that it’s a heterogeneous condition, says Joel Stein, a physiatrist specializing in physical medicine and rehabilitation at Columbia University and Weill Cornell Medical College in New York City (right). “It can affect any area of the brain,” he explains. “There are large and small strokes. There are strokes that bleed into the brain, or block blood vessels, so it’s reasonable to believe that the recovery and treatment may not be the same for all these types of strokes.”
In the United States, on average per year, more than 800,000 people have a stroke; in Europe, the number is roughly 1 million. The costs associated with therapy and loss of productivity for patients who suffer a stroke total nearly US$34 billion per year, which makes it imperative to find effective treatments to help patients recover.
Because strokes can occur in so many different ways, there’s no one-size-fits-all solution. Researchers and engineers are therefore working on several fronts to develop technologies that could be of assistance: from wearable robotic devices to utilizing virtual reality (VR) modules that help patients relearn movement. At the same time, doctors are also interested in incorporating brain stimulation techniques to enhance other technologies that might help patients recover more quickly from impairments following a stroke.
The Bot Can Help You Now
Poststroke, approximately 80% of patients lose normal functioning in one limb and often rely on canes and braces to help with walking. Although some can recover their mobility during physical therapy, stroke patients may have residual abnormalities in gait precluding their participation in activities that might cause them to trip or fall, ultimately affecting quality of life.
Over the years, robotic groups and engineers have developed wearable devices that help patients restore limb mobility after a stroke. Recently, interest has grown in exoskeletons designed to provide the external strength and movement that patients lose after suffering a stroke. The newer skeletons are being developed as soft exosuits with no rigid elements that constrain movement. The ultimate goal is to design soft suits that are unobstructive, i.e., can essentially be worn as clothing.

One of the latest developments of this technology comes from the Wyss Institute for Biologically Inspired Engineering of Harvard University in Boston, Massachusetts. Researchers there have developed a soft exosuit to help stroke patients walk (above). This suit was originally created to help military personnel carry heavy loads and hike long distances while exerting less effort. The team, led by Conor Walsh (below) and Kathleen O’Donnell, wants to leverage the success from the military application and apply it toward a medical condition: stroke. “Stroke seemed like a good opportunity for this technology because the exosuit works by providing small amounts of assistance, but at critical time points in the gait cycle to help improve your walking,” explains O’Donnell, the lead for the medical exosuits program.

The exosuit developed by the Wyss researchers uses cables to coordinate the movement of walking. One end of the suit is worn at the waist, where motion in a patient’s hips generates a force to initiate walking. The other end is wrapped around the affected leg at the calf muscle and the insole of the patient’s shoe. Forces generated in the motor at the hips pull on the cables that terminate at the insole. When this cable retreats, it shortens the distance between the calf wrap and the insole, causing the ankle joint to move and the person using the exosuit to walk.
Thus far, the Harvard team has looked at the immediate effect these exosuits have on the act of walking for poststroke patients and observed a relatively small learning curve for people to correct their gait, once the suit is on. Researchers have seen dramatic changes as early as the very first day someone uses the system. The suit is designed to adapt to an individual’s unique gait, says O’Donnell. “It doesn’t require you to walk with any particular step length or cadence. It measures the way you’re walking and adapts the timing of the assistance it delivers based on how you already walk.”
Moving forward, O’Donnell and her colleagues are eager to see whether there are any lasting impacts on gait rehabilitation once the suit is taken away. “Those studies would take longer to run, but that’s an exciting area to start exploring; [in other words], what are the benefits of wearing something like this over the long term?” The team is now collaborating with ReWalk, a robotics company headquartered in Marlborough, Massachusetts, toward commercializing the technology. At a projected cost of US$19,500 per suit, this technology is intended for purchase by rehabilitation clinics and use by patients during physical therapy sessions, according to Larry Jasinski, chief executive officer of ReWalk. The suits will be worn during the first few days following a stroke. In the best-case scenario, they would fully retrain patients. ReWalk is looking to develop a future exosuit that individuals can take home.
Another robotic device to train stroke patients in walking has already received clearance from the U.S. Food and Drug Administration (FDA). Ekso Bionics, a robotics exoskeleton company headquartered in Richmond, California, has developed the Ekso GT. Made of aluminum and titanium, the exoskeleton retrains users to walk using information from the skeleton’s gyroscope, trajectory sensors, and torque sensors to assess how much help someone needs. The Ekso GT’s sensors continuously monitor the motion of the legs and the patient’s posture to help initiate a step when the user’s weight is properly shifted to his or her feet. A “trainer” or “spotter” can also walk behind the user to help initiate steps. Of the roughly 50 patients who participated in a clinical trial in the United States, those who walked with the exoskeleton in a rehabilitation facility reported more independence compared to those who used traditional physiotherapy techniques. The suit is currently employed in approximately 170 rehabilitation centers worldwide, according to Adam Zoss, a staff scientist at Ekso Bionics. Patients are using it soon after a stroke to regain the ability to walk as quickly and safely as possible. Patients continue to use the suit if their recovery period is lengthy.
Researchers are also developing robotics to help stroke patients who suffer from upper limb mobility issues. Rehab Robotics, a company headquartered in Hong Kong, China, has developed the Hand of Hope for patients recovering from a stroke. The device captures electrical signals from motor neurons that lead muscles to contract and sends them to the hand brace, which ultimately allows the hand to move. This device is not meant for use during daily activities, says Haris Begovic, a clinical advisor at Rehab Robotics. Rather, it’s a therapeutic device often paired with customized games to help retrain the hand in the clinic.
Similar to the soft exosuits under development by engineers at the Wyss Institute, research scientists at the University of Texas at Arlington Research Institute in Fort Worth are developing soft robotic gloves to use in rehabilitation clinics and at home. These soft devices are focused specifically on helping patients regain movement of the fingers and thumbs; they rely on soft actuator sections attached to the joints of the hand. Ultimately, the device controls how the hand bends, flexes, and extends to retrain patients in grasping, manipulating objects, or gesturing. Researchers have tested the robotic glove on healthy patients to assess fit and safety. Although they have yet to conduct efficacy studies in any stroke patients who have lost hand functionality, the team is in the early stages of commercializing the product to create a package that incorporates this device with VR programs that assist in retraining the hand. The hope is that the hand can rewire the brain to compensate for or adapt to the injury. For patients who can’t fully recover after prolonged use with the hand, the device can be used at home.
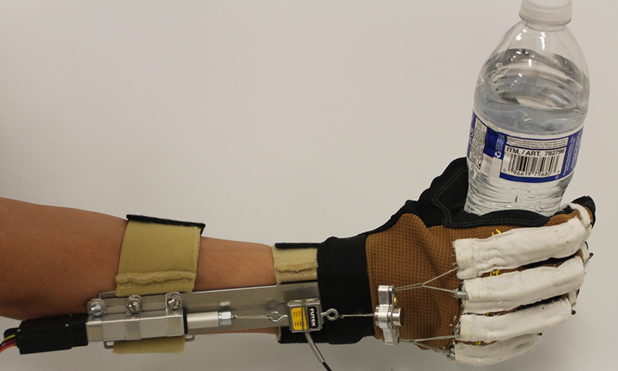
Stein and Matei Ciocarlie, a colleague and mechanical engineer at Columbia, have created MyHand, a glove-like device that helps stroke survivors regain hand motion. MyHand, which uses artificial tendons to help stroke patients regain their ability to grasp objects, is still in development (below).
A New Reality
Ordinarily, VR technology immerses its users in an artificial, computer-generated environment where they can interact with elements through devices like helmets or gloves fitted with sensors. Now, therapists are looking to use elements of VR to help patients recover from strokes.

It wasn’t until the mid-2000s that some VR technologies started making their way into clinics, according to Mindy Levin, a motor rehabilitation researcher at McGill University in in Montréal, Canada (right). “After a stroke, patients move less; they’re not as active as they used to be,” Levin says. “And we know that activity is very important for enhancing brain function.” This means that any way to get a patient moving would be helpful in rehabilitation. Over the years, as VR technology has progressed, some VR games have helped address cognitive problems patients experience poststroke. Additionally, these technologies can help people regain mobility in their arms, legs, and hands.
Motekforce Link, a company headquartered in Amsterdam, The Netherlands, that specializes in rehabilitation technologies has developed modules incorporating VR into a treadmill so patients can walk or train in an immersive environment. Jintronix, a Montréal-based biomedical device company, is incorporating upper limb training, balance, and gait as part of its modules. And Eodyne, a rehabilitation group located in Barcelona, Spain, has developed a rehabilitation gaming system to help patients regain limb function, including in the hands.
These VR systems work by adding a game and reward-based element into the recovery process. They are designed specifically for stroke recovery and incorporate feedback to help patients regain motion. Some of these systems have been used in rehabilitation clinics in Europe and North America. For instance, in a module to help with gait, VR can bring stroke patients into an environment where they need to walk across a busy intersection. A timer indicates to users how long they have to walk across the street before the light changes. In a different module, patients then follow footsteps as dictated on the screen to achieve better gait symmetry or cadence. The VR module could also have users step on a rock, for example, to test balance. After a segment of the game is over, users receive feedback in terms of how well they’ve done.
Researchers studying the effects of VR on stroke rehabilitation are watching to see how patients can benefit from these applications; the field is evolving as motion-tracking systems improve. Currently, high-end motion tracking can be expensive, costing up to hundreds of thousands of dollars. (Less-expensive systems lack the same accuracy of tracking.) According to Levin, researchers are now looking for motion trackers based on accelerometry, known as visual tracking, to better sense patients’ movement.
Brain Stimulation Techniques
While robotics and VR can lead to some modest gains in poststroke rehabilitation, researchers are looking at ways to stimulate the brain using electrical or magnetic means to augment gains made through physical therapy. These techniques are still experimental, and clinicians continue to validate their use in stroke patients.
Transcranial direct stimulation (tDCS) is a noninvasive approach in which physicians apply direct electrical current to stimulate specific areas of the brain. This current passes through two electrodes placed over the head, which can then modulate neuronal activity. A stroke patient, for instance, could wear a cap hooked onto the tDCS electrodes and receive the stimulation before he or she begins a physical therapy session. It’s believed that this prior brain stimulation could potentiate the effects of exercise. “This method is appealing since it’s easy, very safe, and readily combined with other treatments,” Smith says. However, despite its potential, tDCS is not yet an FDA-approved treatment.
In a second potential method, transcranial magnetic stimulation (TMS), neurologists could use a small electromagnetic coil to deliver bursts of magnetic energy to certain parts of the patient’s brain after a stroke. This magnetic field would then induce an electrical current that modulates the currents in the patient’s brain. Compared to tDCS, it would be impractical to deliver TMS during other treatments, but it could be used prior to therapy and may increase gains experienced beyond those achieved by exercise therapy alone. Evidence suggests that TMS, especially if performed repetitively, could affect motor behavior in stroke patients.
In spite of these new technological advances in robotics and VR consoles and the added research in brain stimulation techniques, stroke patients have yet to make substantial gains in recovery, according to Smith. “One hypothesis why it could be so difficult to get those gains is because we haven’t found the right treatments or combination of treatments. The other [hypothesis] may be that the brain’s ability to recover has a biological limit,” he continues. Researchers are also starting to investigate the pairing of stem cells and growth factors to help the brain repair itself more effectively poststroke, but many of these techniques are still in their infancy and have yet to be brought to clinical trials.
The full rehabilitation of patients who are left with physical disabilities after a stroke is likely to remain a challenge in the short term. But recent advances in technology and research suggest that, in the long term, stroke survivors will one day have a range of methods available to help them recover and rehabilitate faster and more fully.
References
- L. N. Awad, J. Bae, K. O’Donnell, S. M. M. De Rossi, K. Hendron, L. H. Sloot, P. Kudzia, S. Allen, K. G. Holt, T. D. Ellis, and C. J. Walsj. (2017, July). A soft robotic exosuit improves walking in patients after stroke. Sci. Translational Medicine. [Online]. 9(400), pp. eaai9084.
- W. H. Chang and Y. H. Kim, “Robot-assisted therapy in stroke rehabilitation,” J. Stroke, vol. 15, no. 3, pp. 174–181, Sept. 2013.
- G. Schlaug, V. Renga, and D. Nair, “Transcranial direct current stimulation in stroke recovery,” Archives Neurology, vol. 65, no. 12, pp. 1571–1576, Dec. 2008.
- E. H. Hoyer and P. A. Celnik, “Understanding and enhancing motor recovery after stroke using transcranial magnetic stimulation,” Restorative Neurology Neuroscience, vol. 29, no. 6, pp. 395–409, 2011.