Even as recently as the mid-1980s, many experts in otology and auditory science thought that restoration of useful hearing with crude and pervasive electrical stimulation of the cochlea was a fool’s dream. The esteemed Prof. Rainer Klinke from Frankfurt (Figure 1, right: Rainer Klinke in the late 1970s.) was among the chorus of critics, asserting in 1978 that “from a physiological point of view, cochlear implants will not work.” Many others made similar categorical statements.
What Professor Klinke and most everyone else missed at the time is the brain’s awesome power to process a highly impoverished and otherwise unnatural input and make sense of it. In retrospect, the main task in developing a useful hearing prosthesis for deaf or nearly deaf people was to provide enough information in the right form for the brain to take over and do the rest of the job. That is not to say that any input would do, as different strategies for stimulation at the periphery produce different results and the initial results were no better than what the experts had predicted. However, once a threshold of quantity and quality of information presented at the periphery was exceeded, the brain could indeed take over and do the rest. And by the rest, I mean most of the job. Designers needed somehow to exceed the threshold, and that is the story of the modern cochlear implant (CI).
The Path to the Modern CI
Today, the CI is widely acknowledged as one of the great advances in medicine and something that even the most ardent proponents of CIs could not have foreseen at the beginning. The decades-long path to today included four steps:
- the pioneering step to implant the first patients and develop devices that were safe and could be used for many years in patients’ daily lives
- the development of devices that provide multiple sites of stimulation in the cochlea to take advantage of the tonotopic (frequency) organization of the cochlea and the auditory pathways in the brain
- the development of processing strategies that utilized these multiple sites far better than before and thereby enabled high levels of speech recognition for the great majority of CI users
- stimulation in addition to that provided by a CI on one side, either with a second CI on the opposite side or with acoustic stimulation for people who have useful residual hearing in one or both ears, usually hearing at low frequencies only.
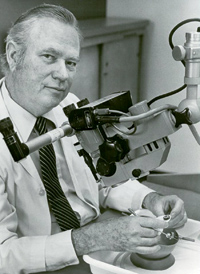
William F. House (Figure 2, right) contributed the most in achieving the first of these steps and got us started on this great journey. He persisted in the face of the criticisms, and, without that determination, the development of the CI certainly would have been delayed, if initiated at all.
House was a physician (as well as the universally acclaimed “father of neuro-otology”) and was assisted by Jack Urban, an electrical engineer, in designing and implementing the earliest devices starting in the mid-1960s. House was working at the House Ear Institute in Los Angeles (founded in 1946 by House’s older half-brother Howard), and Urban was president of an aerospace research company in Burbank.
This partnership between a physician and an engineer presaged larger teams that included one or more physicians (usually more) and sometimes a goodly number of engineers, plus auditory and speech scientists, audiologists and oftentimes additional professionals. Many teams worldwide participated in those subsequent efforts. The modern CI most certainly could not have been developed without the engineers or the physicians. Such partnerships are, of course, what biomedical engineering is all about.
The approximate times for completion of the steps mentioned previously are shown in Figure 3, along with the cumulative number of implant recipients between 1957 and December 2012. The dots in the graph show published data points, and an exponential fit to the data has a correlation higher than 0.99. If that exponential growth continues as expected, a million people will have received a CI or bilateral CIs by early 2020; according to unpublished industry records, the number of recipients had already reached a half million in early 2016.
![Figure 3: Major events in the development of the CI and the cumulative number of implant recipients over the years. (The graphic is adapted and updated from [1] and used here with permission.)](https://www.embs.org/wp-content/uploads/2017/03/wilson03-2649039.jpg)
Two National Institutes of Health Consensus Development Conferences have been convened to evaluate the status of CIs and offer recommendations to physicians in the United States and worldwide on best practices. The first conference, held in 1988, followed introductions of multisite devices into clinical practice (step 2); the second conference, in 1995, met soon after the introduction of the new processing strategies (step 3). The published statement from the 1988 conference suggested that multisite implants were more likely to be effective than single-site implants and indicated that about one in 20 patients could carry out a normal conversation without lip-reading. Such results were encouraging but nonetheless far below the speech-reception scores that would be achieved later. And, in fact, a principal conclusion in the 1995 statement was that “a majority of those individuals with the latest speech processors for their implants will score above 80% correct on high-context sentences, even without visual cues.” That latter performance is a long trip from total or nearly total deafness!
Further improvements in performance were made with adjunctive stimulation (step 4) for people who had enough residual hearing to benefit from combined electric and acoustic stimulation (EAS) and those who were not precluded from receiving a second implant due to national health policies or restrictions in insurance coverage. Both combined EAS and bilateral CIs produced statistically significant increases in speech-reception scores, especially for difficult test items or speech presented in competition with noise or other talkers. In addition, bilateral CIs could reinstate at least some sound-localization abilities, and combined EAS produced large gains in music reception and appreciation. The sound-localization abilities are no doubt due to representations of the interaural level differences the brain uses to infer the positions of sounds in the horizontal plane, and the better music reception may be due to representations with the acoustic stimulus of the first several harmonics of periodic sounds, as those harmonics are vital for robust perception of fundamental frequencies and thus melodic contours.
Details about the design, history, and performance of the modern CI and related hearing prostheses are presented in [2]–[4]. These papers also suggest possibilities for even better performance and wider use in the future.
Acceptance and Honors

I am happy to say that Professor Klinke was quick to acknowledge the wonderful results that had been obtained by the early 1990s and that he was delighted to be proven wrong. He and I became close friends (Figure 4), and I recall with the greatest fondness a special symposium he, Rainer Hartmann, and I organized in 2003 in Frankfurt, with the title “Future Directions for the Further Development of Cochlear Implants.”
Over the past several years, the development of the modern CI has been recognized by many prestigious awards and honors, including the 2013 Lasker–DeBakey Clinical Medical Research Award and the 2015 Fritz J. and Dolores H. Russ Prize. As many readers of IEEE Pulse know, the Russ Prize is the world’s top award in bioengineering and one of three prizes conferred by the U.S.’s National Academy of Engineering (the other two being the Charles Stark Draper Prize and the Bernard M. Gordon Prize), popularly known as the “Nobel Prizes for Engineering.” Similarly, the Lasker awards are second only to the Nobel Prize in Physiology or Medicine for recognizing advances in medicine and medical science; in fact, more than a third of Lasker laureates go on to win a Nobel Prize at a later time. The engineering and medical prizes for the CI reflect the partnerships that made the CI possible and indicate the importance of the CI to both fields.
The CI is by far the most effective and most utilized neural prosthesis to date. And thus, not surprisingly, it has become the principal model for the development (or further development) of other types of neural prostheses and a foremost exemplar of the power of engineering to improve human health. With respect to the latter point, the design of the CI is included in most every biomedical engineering program worldwide (see, e.g., Figure 5). In addition, it is a core component of the curricula for budding audiologists, auditory scientists, speech scientists, and otologists.
Lessons for Biomedical Engineering
But the path to success hasn’t been easy. Joshua Boger (Figure 6), one of the developers of ivacaftor (a drug for the treatment of cystic fibrosis), offers the following cogent and insightful observation about medical breakthroughs, which certainly captures the experience with CIs as well: “The development of ivacaftor was a high-wire act from beginning to end.… If you are looking for dramatic changes in medicine, you are not looking to be comfortable in research; every breakthrough project I know about has passionate detractors” [5].

Some lessons biomedical engineers can learn from the development of the CI are that the experts are not always correct and that perseverance and teamwork are important. Thanks to the second point, most of today’s CI users can communicate fluently via the telephone, even with previously unfamiliar people at the other end and even with unpredictable and changing topics. That wonderful outcome could not have been reasonably imagined at the outset or, indeed, up to the early 1990s when new processing strategies were introduced into clinical practice and the number of implant recipients began to skyrocket (Figure 3).
Although room remains for improvement, the present-day devices “allow children to be mainstreamed into regular schools, adults to have a wide range of job opportunities, and for all recipients to connect in new and important ways with their families, friends, and society at large” [6]. The resulting human and economic benefits have been immense—benefits that were made possible by grit, brilliance, key discoveries, exquisite engineering, and multidisciplinary teams.
Acknowledgment
This article is largely based on a guest of honor address by the author at the 149th Annual Meeting of the American Otological Society, held in Chicago, Illinois, 18–22 May 2016.
References
- B. S. Wilson and M. F. Dorman, “Interfacing sensors with the nervous system: Lessons from the development and success of cochlear implants,” IEEE Sensors J., vol. 8, no. 1, pp. 131–147, 2008.
- B. S. Wilson and M. F. Dorman, “Cochlear implants: A remarkable past and a brilliant future,” Hear. Res., vol. 242, no. 1–2, pp. 3–21, 2008.
- F. G. Zeng, S. Rebscher, W. Harrison, X. Sun, and H. Feng, “Cochlear implants: System design, integration, and evaluation,” IEEE Rev. Biomed. Eng., vol. 1, pp. 115–142, 2008.
- B. S. Wilson, “Getting a decent (but sparse) signal to the brain for users of cochlear implants,” Hear. Res., vol. 322, pp. 24–38, 2015.
- J. Boger, “Cystic fibrosis and the need for partnerships,” in Accelerating the Development of New Drugs and Diagnostics. Washington, D.C.: National Academies Press, Institute of Medicine, 2012.
- B. S. Wilson. Acceptance remarks, 2013 Lasker Awards Ceremony. [Online].