Clinicians have long used ultrasound to image inside the body, but it may prove even more useful as a therapeutic tool
Focused ultrasound is an early stage, noninvasive therapy with the potential to treat a range of medical conditions. Like diagnostic ultrasound, it uses sound waves above the range of human hearing. But its purpose is to interact with tissues in the body, rather than just produce images of them. In focused ultrasound, multiple, intersecting beams of high frequency sound are aimed to converge on specific targets deep within the body. There, the ultrasound energy can act in multiple ways to either modify or destroy tissue.
The U.S. Food and Drug Administration (FDA) has approved focused ultrasound to treat eight conditions, including uterine fibroids, cancer that has spread into the bones, and breast, prostate, and liver tumors. It is under investigation for dozens of other applications [1]. However, it is the potential of focused ultrasound to treat diseases of the brain that is generating the most excitement. Already approved for the treatment of Parkinson’s disease and essential tremor, researchers are exploring focused ultrasound for a variety of other neurological and psychiatric conditions.
“The brain has taken over focused ultrasound,” says Elisa Konofagou, professor and principal investigator at the Ultrasound and Elasticity Imaging Laboratory at Columbia University (Figure 1). “Neurosurgeons are embracing it, as well as neurologists, oncologists, and psychiatrists. There are many devastating brain diseases that could potentially benefit from ultrasound.”

Figure 1. Elisa Konofagou is a professor in BME and a principal investigator at the Ultrasound and Elasticity Imaging Laboratory, Columbia University. (Photo courtesy of Konofagou.)
Heat as a tool
Focused ultrasound can be made to produce different therapeutic effects by varying the parameters of the ultrasound beams. In high intensity focused ultrasound (HIFU), high power sound waves converge at one point to raise the temperature and destroy tissue. Typically, magnetic resonance imaging is used to identify and target the specific tissue to be treated and guide the treatment in real time. This technique is FDA-approved and in clinical use for several applications.
The ability of HIFU to precisely ablate tissue without requiring surgery makes it a promising alternative to deep brain stimulation (DBS) for movement disorders associated with Parkinson’s disease and essential tremor. Although DBS of targets in the thalamus can be effective for these conditions, it is a costly and invasive treatment.
“We know that the cells in that part of the brain fire abnormally and are entrained to fire with the tremor,” says Nir Lipsman, a neurosurgeon at Sunnybrook Research Institute in Canada (Figure 2). “Getting rid of that neuronal activity, whether with electricity or heat, is a way to impact that tremor. High intensity focused ultrasound is a new tool that we use in an established way—to generate a lesion in the brain.”

Figure 2. Nir Lipsman is a neurosurgeon at the Sunnybrook Research Institute, Canada. (Photo courtesy of Sunnybrook Health Sciences Centre.)
Over the last ten years, Lipsman has helped develop several clinical trials of focused ultrasound. He was part of the team that established HIFU as an effective and safe treatment for patients with essential tremor, leading to FDA-approval in 2016 [2]. A recent follow-up study demonstrated that patients who underwent HIFU for essential tremor sustained improvements for up to five years [3].
Currently, HIFU is FDA-approved and commercially available for the treatment of essential tremor and tremor-dominant Parkinson’s disease. It is also under investigation for other conditions where overactivity in a specific brain region causes problems, such as chronic pain and obsessive-compulsive disorder [4], [5].
Dialing down the intensity
In contrast to HIFU that destroys cells, focused ultrasound at low intensities, known as low intensity focused ultrasound (LIFU), is under investigation for its ability to modulate neuronal activity without incurring cell damage. There is mounting interest in the use of LIFU to treat neurological and psychiatric disorders, but this technique is still experimental [4], [5].
There are clear targets for some conditions, says Noah Philip, a professor at Brown University and the founding section chief of psychiatric neuromodulation at VA Providence (Figure 3). For instance, he is conducting trials of LIFU to inhibit brain areas known to be involved in post-traumatic stress disorder, anxiety, and depression. “If we can noninvasively reach deep into the brain and turn off these areas that drive psychiatric illnesses, the hope is that it will yield a treatment that is more effective than what we have right now,” says Philip.

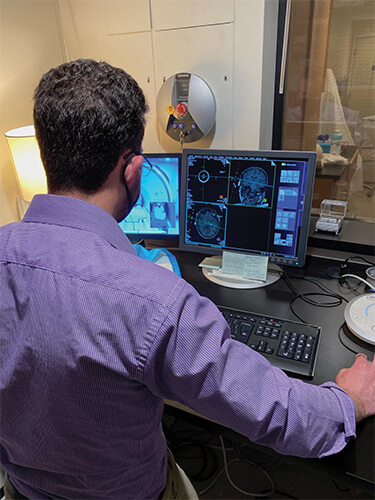
Figure 3. Noah Philip, professor at Brown University and the founding section chief of psychiatric neuromodulation at VA Providence. (Photos courtesy of Brown University.)
That is also the hope of Wynn Legon, an assistant professor and a principal investigator at the Fralin Biomedical Research Institute at the Virginia Tech Carilion School of Medicine (Figure 4). Legon has been at the forefront of LIFU research for a decade and his lab is currently focusing on investigating applications for addiction and chronic pain. “We’ve done a lot of studies in healthy control participants demonstrating its safety and tolerability and showing that it can reduce their perceived pain,” he says. “Now we want to see how durable the effect is and if it will impact quality of life or reduce pain for patients with chronic pain. We are just on the cusp of getting into some clinical indications.”

Figure 4. Wynn Legon is an assistant professor and a principal investigator at the Fralin Biomedical Research Institute at the Virginia Tech Carilion School of Medicine. (Photo courtesy of Clayton Metz for Virginia Tech.)
Shaking open barriers
In addition to manipulating cells deep in the brain, LIFU shows promise in another application: opening the blood–brain barrier. This protective membrane surrounds a specialized system of blood vessels in the brain, preventing pathogens and other dangerous substances in the blood from gaining entrance. However, it can also prevent drugs and other therapies from reaching the brain, complicating the treatment of brain tumors and Alzheimer’s disease, among other conditions.
Researchers are now leveraging the fact that LIFU mechanically stimulates anything under its focus to disrupt the blood–brain barrier. This is achieved by injecting microbubbles into the bloodstream and then applying LIFU to them as they pass through blood vessels in the brain. The ultrasound activates the bubbles, temporarily loosening up the blood–brain barrier, providing an opportunity for drugs or other therapeutic molecules to pass through.
Konofagou’s group recently demonstrated the use of LIFU to open the blood–brain barrier and enable genome editing [6]. Gene therapy is a sought-after goal for neurologic diseases, such as Alzheimer’s and Parkinson’s, but getting gene editing vectors across the blood–brain barrier has proven challenging. Konofagou used LIFU and microbubbles to open the blood–brain barrier and deliver CRISPR-encoded viral vectors into the brains of mice. The technique increased gene editing efficiency in mouse neurons, suggesting that it could one day be used to edit the genome of neuronal cells to correct genes involved in brain diseases.
Konofagou’s research has also shown that opening the blood–brain barrier with ultrasound may have therapeutic effects on its own. “Opening the blood–brain barrier stimulates immune cells in the brain called microglia that are mechanically sensitive,” says Konofagou. “They respond to the ultrasound by clearing away more debris in the brain, such as the proteins beta-amyloid and tau that accumulate in Alzheimer’s disease.” In a recent experiment, mice treated with LIFU alone had decreased levels of beta-amyloid and tau and improved working memory. When the researchers applied the technique to individuals with Alzheimer’s in a clinical trial, they found a modest reduction in beta-amyloid in the region where the blood–brain barrier was opened compared to an untreated area [7].
Challenges and unknowns
The potential of focused ultrasound to provide noninvasive access to the brain and treat previously intractable diseases has produced a lot of buzz, but there are limitations to the technology. Currently, HIFU’s usefulness is limited to making lesions in areas near the center of the brain. In addition, not everyone’s skull is amenable to HIFU; denser skulls can absorb much of the ultrasound energy and make it difficult to create lesions in some patients, says Lipsman. “These are some of the technical limitations to the technology that you learn about once you start using a tool widely,” he says. “But we and others are working on overcoming these limitations to make HIFU as widely accessible as possible.”
When it comes to LIFU, basic questions remain about how the treatment produces its modulatory effects on cells. Legon suspects mechanical forces are important. “There is evidence showing that some channels in brain cells that have been traditionally regarded as being voltage-gated electrical channels also respond to mechanical energy,” he says. “The idea is that if you send in a pressure wave across a cell membrane or to one of these specific channels, it will perturb the channel mechanically and that can bias it to either open or close.”
While the exact mechanisms underlying how LIFU works are under active investigation, our shifting understanding of how psychiatric illnesses work presents another challenge, says Philip. Today, psychiatric illnesses are thought of as disruptions of large-scale, functional neural networks, marked by unhealthy patterns of communication between different brain areas. “We have a highly precise and specific intervention device and yet, we are becoming more mindful that these illnesses are a product of large-scale neural networks,” says Philip. “We hope that modulating core elements of these networks is going to be helpful, but it is entirely possible that LIFU may not be sufficient because it is, in fact, too precise a tool.”
Bright future
Despite the current unknowns, Philip and others are optimistic about the future of focused ultrasound. “As a psychiatrist as well as a researcher, I’m acutely mindful that the treatments we have today simply do not meet our patients’ needs,” he says. “This technology, unlike some other neuromodulatory interventions such as transcranial magnetic stimulation or deep brain stimulation, has the potential to be extremely portable and scalable.”
According to the Focused Ultrasound Foundation, there are nearly 40 neurological and psychiatric applications currently under investigation; most are in early stages. In addition to the brain disorders already mentioned, this includes depression, epilepsy, schizophrenia, bipolar disorder, and amyotrophic lateral sclerosis [1]. Much work remains to establish where and how the technology will provide the most therapeutic value. “The great advantage of focused ultrasound is the ability to reach these previously inaccessible areas of the brain noninvasively,” says Legon. “I think it has promise for any clinical indication where there is an established location deep in the brain.”
In addition, Lipsman looks forward to future studies to investigate how best to take advantage of the transient blood–brain barrier opening that LIFU induces. “We are working closely with our partners in the drug development world to determine which drugs we should deliver to the brain for different neurological diseases,” he says. “Whether it’s gene therapy, or anti-amyloid or anti-tau antibodies for Alzheimer’s, or enzymes for Parkinson’s—this pairing of pharmaceutical or therapeutic development with the technology is an exciting area.”
“Although we are very much in the early days of using focused ultrasound to treat brain diseases, I think there is a bright future for this technology,” Lipsman adds. “We are learning a lot about the hardware and software, as well as the optimal indications for focused ultrasound.” Given the challenges associated with accessing the brain and the limitations of some current treatments—as well as the mounting efforts to optimize the technology—the excitement surrounding focused ultrasound’s potential is warranted.
References
- Focused Ultrasound Foundation: Diseases and Conditions. Accessed: Oct. 15, 2023. [Online]. Available: https://www.fusfoundation.org/diseases-and-conditions/
- W. J. Elias et al., “A randomized trial of focused ultrasound thalamotomy for essential tremor,” New England J. Med., vol. 375, no. 8, pp. 730–739, Aug. 2016, doi: 10.1056/NEJMoa1600159.
- G. R. Cosgrove et al., “Magnetic resonance imaging-guided focused ultrasound thalamotomy for essential tremor: 5-year follow-up results,” J. Neurosurgery, vol. 138, no. 4, pp. 1028–1033, Aug. 2022, doi: 10.3171/2022.6.JNS212483.
- Y. Meng, K. Hynynen, and N. Lipsman, “Applications of focused ultrasound in the brain: From thermoablation to drug delivery,” Nature Rev. Neurol., vol. 17, no. 1, pp. 7–22, Jan. 2021, 10.1038/s41582-020-00418-z.
- H. Baek et al., “Clinical intervention using focused ultrasound (FUS) stimulation of the brain in diverse neurological disorders,” Frontiers Neurol., vol. 13, May 2022, Art. no. 880814. doi: 10.3389/fneur.2022.880814.
- Y.-H. Lao et al., “Focused ultrasound-mediated brain genome editing,” Proc. Nat. Acad. Sci. USA, vol. 120, no. 34, Aug. 2023, Art. no. e2302910120, doi: 10.1073/pnas.2302910120.
- M. E. Karakatsani et al., “Focused ultrasound mitigates pathology and improves spatial memory in Alzheimer’s mice and patients,” Theranostics, vol. 13, no. 12, pp. 4102–4120, Jul. 2023, doi: 10.7150/thno.79898.



