With the advent of wearable biometrictechnology like smart watches, “hacking” our bodies’ functions and cycles has become a tool in the never-ending quest for better health. And sleep is no exception. For example, a staggering one-third of Americans don’t get enough sleep, according to the Centers for Disease Control and Prevention (CDC).
Aside from affecting one’s mood, less sleep is correlated to a number of very real health risks. The American Academy of Sleep Medicine and the Sleep Research Society states that adults who get less than seven hours a sleep a night are at risk for higher levels of obesity, diabetes, heart disease, stroke, and depression, as well as impaired immune function, accelerated signs of aging, and increased tendency for errors and accidents [1]. (To learn more about our understanding on how and why we sleep, see “Sleep on It”.)
Because sleep is so directly tied to health, it is as important to study as nutrition or exercise, according to W. Christopher Winter, M.D., president of the Charlottesville Neurology and Sleep Medicine (Figure 1) and author of The Sleep Solution. The two biggest issues he sees are excessive sleepiness from inadequate or dysfunctional sleep, and people who have insomnia. Other common problems include sleep apnea—a state of paused breathing during sleep—and restless leg syndrome—an uncontrollable urge to move the legs at night.
Whether a good night’s sleep means the difference between a good day or a bad day, or sickness or health, consumer sleep tracking technologies suggest a way to improve sleep without needing to spend the money, time, and effort to go into a sleep lab for a clinical-level analysis. “[Sleep tracking] devices are simultaneously becoming both more accurate and smaller and less invasive,” says Winter. “I employ these devices frequently to get insight about my patient’s sleep.”
While many of the currently available devices fall short of true sleep analysis, experts point to the field’s growing potential to unlock a new era of understanding sleep, diagnosing disease, and even unlocking our dreams.

Parsing sleep trackers
In addition to hundreds of tracking apps through smart phones and watches, there’s no shortage of wearable or in-home devices to help measure, understand, and, presumably, improve your sleep.
Wearables, such as wristbands, are available from Samsung, Fitbit, Whoop, Garmin, and others that record movement and other metrics to make informed guesses about users’ sleep, creating a “sleep score” to help track sleep quality over time and even suggesting ideal bedtime and awake times. For those who don’t like to wear devices, Beddit, Emfit, Beautyrest, Withings, and others offer underthe- mattress recordings, while technologies like Eight Sleep’s pod, Bryte’s smartbed, Serta Simmons’ Tomorrow mattress, the Sleep Number 360 C2 Smart Bed and its kid-geared SleepIQ bed have a host of embedded sensors built into the bed itself that track activity to, for example, adjust temperature zones on the bed or provide custom sleep reports. S+ by ResMed offers a “no-contact” bedside tracker, which records a user’s breathing and movement from a distance, as well as temperature and light, to provide a sleep report and recommendations. In addition to trackers, other devices to heighten sleep include smart lamps (like Casper’s Glow), white noise machines, weighted blankets, and even a huggable sleeping device called the Somnox Sleep Robot.
Despite the abundance of options, consumer-based sleep analysis technologies typically do not have much independent validation as to their efficiency, and worse, can even backfire, as evidenced by a recently coined sleep disorder called orthosomnia, where people experience insomnia due to feeling anxious over their sleep metrics.
“It’s a bit of a wild west out there,” Emmanuel Mignot, the Craig Reynolds Professor of Sleep Medicine at Stanford University, says in terms of sleep trackers. Mignot, who discovered the cause of narcolepsy and directed Stanford’s Center of Sleep Sciences and Medicine for ten years, points out that an inherent problem with most sleep trackers is that they can’t reliably distinguish quiet wakefulness from sleep: measuring physical movement wouldn’t capture someone who is laying still but not asleep, for example.
While many tracking technologies use accelerometers to track movement and guess sleep stage (with less movement equated to deeper sleep), newer trackers seek to integrate additional physiological measurements. For example, since our temperature, blood pressure, and heart rate tend to drop during non-rapid eye movement (REM) sleep, devices that measure the heart’s beats per minute (BPM) may have a better chance at pinpointing sleep stages. Additionally, during REM (dreaming) sleep, the sleeper is typically paralyzed but has an unstable pulse, so an algorithm could look for low movement and varying pulse rate to differentiate REM sleep. But, these metrics are still only inferring sleep.
“Often these technologies have limitations if they don’t measure brain waves; it’s only then you can really tell if someone’s asleep,” Mignot says, adding that measuring sleep would be a boon to research. “If we can directly record a person’s sleep, we can relatively easily get a good picture of their general physiology, including brain and heart health, which is much harder to record during daily waking activities.”
Winter agrees that wearable devices that can reproduce sleep study grade electroencephalogram (EEG) signals would be especially useful. “I would like to be able to monitor brain activity while a consumer is at home, particularly in this era of COVID,” he says.
Headbands offer one way to measure brain waves. The Philips SmartSleep headband has one such wearable EEG system, which uses sensors on the scalp to detect subtle electrical activity generated by brain waves. Designed for people without sleep issues, the device aims to improve the quality of sleep by playing acoustic tones to help boost the brain’s deep sleep waves, thought to be the most restorative for overall health, based on research from the University of Wisconsin–Madison [2]. Another EEG headband on the market, this one registered as an FDA Class II Medical Device, is called Dreem and offers consumers custom sleep coaching programs.
Sleep headbands have had a notoriously difficult time finding a market place (see “How’s My Sleep?”). One big obstacle to headbands is that many consumers may find them uncomfortable or distracting to sleep in; another is that many sensors need to be integrated for a complete assessment of sleep and sleep disorders. Mignot, who is on the scientific advisory board for Dreem, says these types of consumerbased EEG technologies are advancing rapidly, as advances in manufacturing and materials are heightening accuracy and improving wearability.
As they continue to improve, these devices could be a game changer for health monitoring. In July, Mignot and others published work in JAMA Neurology showing that decreased REM sleep correlated to greater risk of death in several thousand people and raises the question of whether sleep monitoring could be an early predictor of disease [3]. To better understand novel biomarkers for sleep and disease, Mignot’s lab has created machine-learning systems to mimic the abilities of sleep technicians to parse data in brain wave recordings to determine phases of sleep and potential anomalies.
“Sleep is a general window into your physiology,” he says. “Detecting disruptions in the brain could potentially predict things like depression, Alzheimer’s, or schizophrenia. We don’t really know yet, but it’s an exciting area with enormous potential.”
Treating sleep issues
Devices that fall short of clinical-level sleep detection can still be helpful to customers. For sleep deprivation, the use of consumer devices can call attention to loss of sleep and might prompt users to prioritize getting more sleep, according to Jennifer Kanady, Ph.D., the lead clinical innovator for sleep at London and San Francisco-based Big Health.
“However, it’s important to note that these devices could also have the opposite effect; some may hyper-focus on the output, leading to sleep-related anxieties and subsequent sleep problems,” Kanady says, adding that tracking sleep may increase anxiety for insomnias and exacerbate sleep problems.
Instead, she says, insomniacs may find use from digital applications of a recommended treatment for the condition: cognitive behavioral therapy for insomnia (CBT-I), which helps patients identify and change negative thoughts or beliefs that affect sleep and replace them with good bedtime habits. Numerous apps offer virtual CBT-I coaches, such as the U.S. Department of Veteran Affairs. Big Health’s Sleepio program presents a digital professor avatar that can walk users through CBT-I to handle insomnia (Figure 2), in use by CVS Health and other companies.
“Many randomized controlled trials have demonstrated time and time again that CBT-I is effective across different and diverse populations…there are zero to few side effects, and the benefits are long lasting,” says Kanady. However, she adds, traditional in-person CBT-I is not always accessible or affordable, while digital options can bridge the gap.

In addition to insomnia, sleep apnea may soon be easier to treat with new technologies. More companies like Fitbit and Garmin, are incorporating SpO2 sensors in their trackers which measure blood oxygen levels. Levels are known to decrease in cases of sleep apnea as breathing becomes obstructed, so seeing dips in the measurements could be a cue for the user that they have the condition. NightBalance’s Sleep Position Trainer (recently acquired by Philips), developed a chest strap that uses a gentle vibration to encourage sleepers to turn from their back, reducing the occurrence of sleep apnea.
Detecting COVID-19
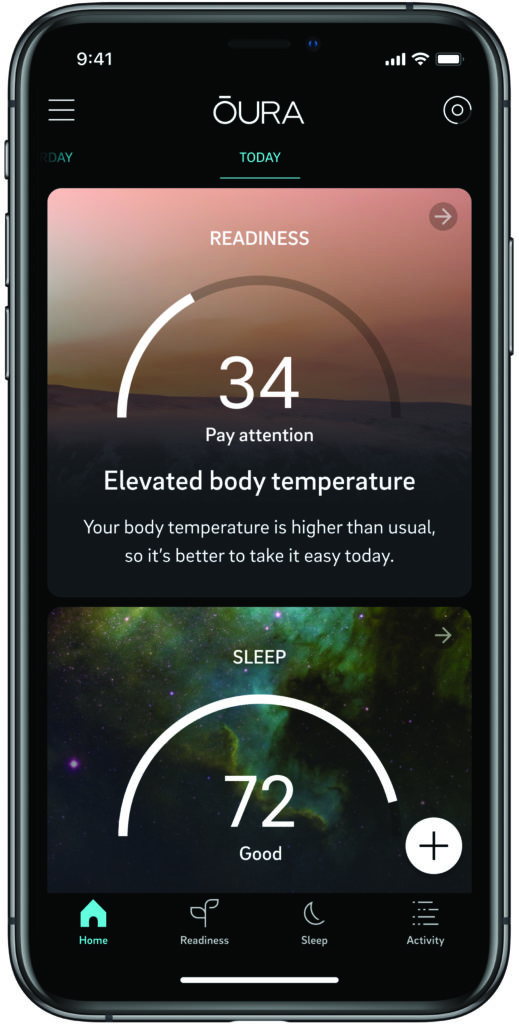
In March 2020, Finland resident Petri Hollmen noticed his Oura, a sleep tracker in the form of a ring (Figure 3), showing a slightly higher temperature. Even though he felt fine, he decided to get a COVID-19 test, which confirmed he was positive for the novel coronavirus and prompted him to self-quarantine.

In April, Oura (headquartered in Oulu, Finland), together with the Rockefeller Neuroscience Institute and WVU Medicine, launched a study with 600 health care workers to see if data from the Oura ring—which tracks changes in body temperature, respiratory rate, and heart rate day and night—could help with early detection of COVID-19 people with no early symptoms, like Hollman (Figure 4). The team announced that the ring coupled with RNI’s COVID-19 monitoring smartphone app (Figure 5) was able to detect symptoms with over 90% accuracy three days before a user noticed them.
“We designed the Oura Ring and app to help people better understand their health through daily personalized insights. Through research studies with UCSF and The Rockefeller Neuroscience Institute, we now have compelling evidence for how Oura can support discoveries in illness detection, symptom profiles, and recovery,” said Harpreet Rai, CEO of Oura.
The ring uses infrared light photoplethysmography (PPG), which reaches deeper than the green light LEDs found in most other wearables for higher accuracy in body metrics (the company reports the device detects a resting heart rate and heart rate variability in the upper nineties percentiles compared to medical- grade tests, as well as temperature changes as small as 0.05 °C). Currently, thousands of health care workers across the country are using the smart ring to detect COVID-19 and, in July 2020, NBA and Oura Health announced a partnership to provide the smart rings and early illness detection monitoring services to league staff in an effort to help restart the season.

More generally, any method to improve sleep will also help fight COVID-19 indirectly, as better sleep correlates with a stronger immune response. “Sleep loss is associated with reduced natural killer cell activity, which helps to explain why we are more likely to get sick following poor sleep. Therefore, getting a good night of sleep is a great way to protect yourself during the COVID-19 pandemic,” confirms Kanady. “Early data suggests that many individuals are struggling with worry and anxiety as a result of the pandemic. When we don’t sleep well, we tend to feel more anxious, and when we are anxious, we don’t sleep well; it can feel like a very vicious and frustrating cycle. The good news is that this cycle can be broken and treating sleep disturbance and promoting healthy sleep often reduces anxiety symptoms as well.”
Looking toward the future
In the research realm, scientists are pushing the boundaries of wearable sleep technologies. MIT Media Lab’s Fluid Interfaces Group led by Prof. Pattie Maes aims to take advantage of hypnagogia— the state between waking and deep sleep when one experiences vivid, creative imaginings right before falling asleep.
A sensor-equipped glove called Dormio tracks a user’s muscle tone, heart rate, and skin conductance and plays a recorded cue when it detects the dreamer entering hypnagogia to help them record their thoughts. The group has also created a smart sleep mask called Fascia that records EEG and facial expression to read the emotional content of dreams and a device called BioEssence that releases different scents in an attempt to promote learning and consolidate memories during sleep.
To get to a deeper understanding of sleep and dreams, some researchers aim to go beyond EEG. Yukiyasu Kamitani, Ph.D., an informatic researcher at Kyoto University, uses deep neural networks to reconstruct images from functional magnetic resonance imaging (fMRI) of sleeping subjects. These rudimentary images of people’s dreams are a step closer, he hopes, to understanding how conscious experience can emerge from spontaneous brain activity.
“Measuring brain activity during sleep is difficult, especially using a brain scanner like MRI. EEG does not provide signals that allow for reading detailed mental states,” he says. Implanted electrodes— like the type Elon Musk’s Neuralink company is developing—could offer more precision and help unravel mysteries like how and why the brain daydreams, he adds.
As technology continues to grow more sensitive and accurate for users and researchers alike, the potential to squash sleep issues and maximize well-being through dreams and sleep, seem within reach. Whether for a sleep condition or just to better one’s creativity, new technologies are charging ahead with the promise of unlocking our sleep.
References
[1] N. F. Watson et al., “Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society,” J. Clin. Sleep Med., vol. 11, no. 6, pp. 591 592, Jun. 15, 2015. [Online]. Available: https:// aasm.org/resources/pdf/pressroom/adult-sleepduration- consensus.pdf [2] G. Tononi, B. Riedner, B. Hulse, F. Ferrarelli, and S. Sarasso, “Enhancing sleep slow waves with natural stimuli,” Medicamundi, vol. 54, no. 2, pp. 82–88, Jan. 2010. [Online]. Available: https://www. researchgate.net/publication/279545240_Enhancing_ sleep_slow_waves_with_natural_stimuli
[3] E. B. Leary et al., “Association of rapid eye movement sleep with mortality in middle-aged and older adults,” JAMA Neurol., Jul. 6, 2020, doi: 10.1001/ jamaneurol.2020.2108. [Online]. Available: https:// jamanetwork.com/journals/jamaneurology/articleabstract/ 2767713
Kristina Grifantini, M.S., is an award-winning science writer hailing from San Diego, CA. She has written hundreds of technology and medical articles for a variety of publications, including MIT Technology Review, Sky and Telescope, LiveScience, and others.



