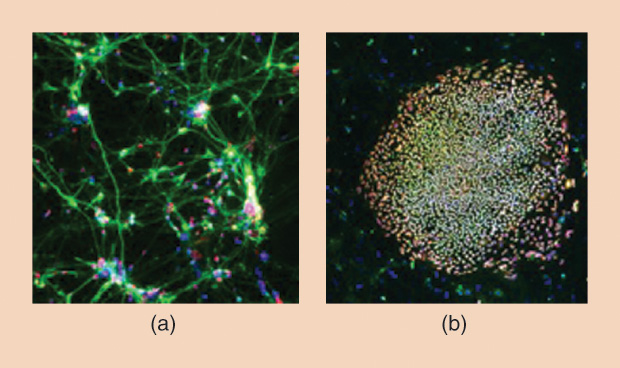
Researcher Jeanne Loring thinks she has a good method for reversing the symptoms of Parkinson’s disease, and she believes this method—a stem-cell therapy—will find its way to clinics in as little as twoand- a-half years. Although the work has progressed very smoothly, one thing has continued to nag at her: is it actually safe to transplant induced pluripotent stem cells (iPSCs), or are these cells potentially dangerous to patients?
Surprisingly, even though stem-cell research is currently underway in many labs around the world, this basic question has remained unanswered. So Loring, a professor of developmental neurology at the Scripps Research Institute in La Jolla, California, discussed it with Nicholas Schork, a professor and the director of human biology at the J. Craig Venter Institute, also in La Jolla, and together they embarked on a comprehensive analysis to find out whether stem cells are safe or not. The results of that study, published in Nature Communications in February 2016 [1], provided some of the first real evidence about whether iPSCs were prone to mutations that could harm patients.
IEEE Pulse spoke with these two researchers about the study, their findings, and how they hope the results will impact stem-cell research and associated therapies.
IEEE Pulse: What concern were you addressing with this study?
Loring: Reprogramming skin cells into pluripotent stem cells is a pretty dramatic event, and there had been several papers published suggesting that reprogramming could cause harmful mutations. We were pretty sure that wasn’t really true, so we set out to prove it.
Schork: The belief is that the use of stem cells in cell-replacement therapies will be a reality, so it’s important to know whether the cells that are going to be put into a patient’s body are full of deleterious mutations. That’s also true for a researcher who may not be using stem cells for clinical applications but is using them in assays studying phenomena in a petri dish or in an animal model. Essentially, they’d want to know if certain mutations were present because those mutations could impact their results.
IEEE Pulse: How did you approach the study?
Schork: There are actually several different ways of reprogramming cells, and they all exploit different mechanisms. So we looked at three of these strategies to see if any of them induced deleterious mutations, and, if they did, we wanted to know whether those mutations actually had some kind of functional effects that would compromise resulting stem cells as cell-replacement therapies. For instance, if the act of creating pluripotent cells seemed to induce a particular mutation known to cause cancer, the last thing you would want to do is put those cells back into somebody’s body.
IEEE Pulse: What were the three reprogramming strategies you targeted?
Loring: One was the original method, which uses retroviruses that integrate into the genome. Another was the non-integrating Sendai virus, which uses as viral delivery but the Sendai virus isn’t capable of integrating into the genome, so it’s a transient expression of the transcription factors (involved in reprogramming). And the third method was synthetic messenger ribonucleic acid, which is also a transient expression of the transcription factors. These three methods are the most popular in the field now, and we wanted to find out whether one method was better than another. Frankly, there had been a fair number of papers published in which people would claim the method they were using was safer than the methods others were using, but they had no evidence to actually show that. For somebody like me who is actually planning on putting these cells into people and is focusing on quality control, this is not a subtle difference. Choosing the method you use for reprogramming should be based on science, and not on somebody’s opinion.
IEEE Pulse: How did you set up the study to compare the strategies?
Schork: We came up with a new protocol for evaluating the mutation profiles of the cells, and we spelled out each step so that if somebody wanted to do a similar study, they could follow our recipe. We took a fibroblast, a kind of skin cell, from a donor, and used clones of that fibroblast as the starting material for each of the reprogramming techniques. We did this to make sure that the cells made were on an equal playing field for all three techniques and any of the mutations we identified after we reprogrammed the cells would be attributable to the methodology and not necessarily to differences in the starting material.
As these cells were growing and moving toward the pluripotent state, we checked to see if, how many, and what type of mutations were building up. Instead of just subjecting the cells to exome sequencing or looking only at candidate genes, copy number, or gene expression, we did whole genome sequencing to identify mutations.

IEEE Pulse: Why was it important to use whole genome sequencing rather than one of the other techniques, such as exome sequencing?
Schork: The exome only gets at the coding regions of the genome; so while you can identify variations that impact protein structure, you can’t interrogate regulatory regions.
Loring: I’ve never really liked exome sequencing for that reason. As a genome biologist, I know that regulation of expression of genes makes all the difference in whether a cell becomes one thing or in whether a cell dies. It’s not the genes themselves, but the regulation of the genes that’s important.
IEEE Pulse: Was there anything else that made your study unique?
Schork: We used a suite of bioinformatics tools to identify the mutations—the belief being that if we settled on any one, it might have its own biases. So we used a couple of different ways of identifying the mutations from the sequence data to assess their consistency. Researchers may have used any one of those tools in an isolated context, but we put many of them together, and that’s one key element of what really differentiates our studies from others.
Loring: I’m really acutely interested in new technology, especially new genomics technology, and for this study we collaborated with a company called BioNano Genomics that has come up with a method for looking at really long strands of deoxyribonucleic acid (DNA), which are essentially the contigs (DNA segments) we used to use, to see how all the strands overlap in the entire genome. That method allows them to find really big deletions, duplications, and even inversions that, interestingly, you can’t see by bioinformatic analysis of whole genome sequencing.
IEEE Pulse: What were your results? Did you find any indication that these stem cells had dangerous mutations?
Schork: We ultimately found that there was no kind of systematic induction of overtly deleterious mutations in the three different reprogramming techniques that we used. In other words, there was no big smoking gun where, for example, any of the three methods always seemed to create the same clearly deleterious mutation. Of course, since mutations naturally occur during the cell replication in our bodies, an individual stem cell now and again would be likely to develop one or another mutation, but there was nothing obvious that we found in the stem cells created by any of the three strategies that would make us think twice about using them.
Loring: This lets us start with the assumption that these stem cells are safe rather than the opposite, which is starting with the assumption that they are dangerous. There’s been a certain fear factor surrounding stem cells, and I hope this will help people get over it.
IEEE Pulse: So based on this study, what conclusions can you draw about pluripotent stem cells and their use in clinical applications?
Loring: There’s nothing we found that precludes their use, so we can stop worrying about the programming method we’re employing and can move forward.
Schork: When the press picked up on our study, they said that we reported stem cells were safe, but what we actually reported was that we found no systematic mutations. That’s not the same thing. It’s possible that within a pool of stem cells that have no systematic mutations, there might be a cell here or there that actually has a randomly occurring deleterious mutation just as random mutations occur naturally as cells replicate in our bodies.
With iPSCs, you’d never be able to know if a certain cell you were implanting had an individual mutation because, to test it, you’d have to sequence it. And that means you’d have to destroy it. So what we do instead is test a sample of a pool of potential replacement cells to find any problems that are common across the cells. We found absolutely nothing obvious that would make us say there’s no way that these cells have potential in cell-replacement therapies.
Loring: In other words, our paper said that the sky isn’t falling.
IEEE Pulse: What other research is needed on pluripotent stem cells, and what would such research tell us about their safety for clinical use?
Schork: Our study went through the generation of the pluripotent state, but there’s the next step where you differentiate those pluripotent cells into neurons, cardiac cells, or any other unique cell type that you need. That next step also needs to be studied to see if there are any systematic issues.
So overall, I believe we need better and more sophisticated strategies to give a pool of iPSCs a clean bill of health, and that will be difficult because, as I said, mutations occur randomly. That’s true of any cell-replacement therapy, whether it’s based on a traditional gene therapy or one that uses iPSCs. As we move even closer to clinical application, however, I think we’ll need industrial-scale ways of vetting the quality and health of the cells we’re going to think seriously about putting back in someone’s body.
IEEE Pulse: Dr. Loring, now that this study has found no systematic problems with iPSCs, what’s next for your own research on Parkinson’s disease?
Loring: We’ve done our first meeting with the Food and Drug Administration, and we’re hoping to start our phase one trial in 12–18 months. If everything goes according to plan—and it has so far—a reasonable guess is that it’s about two-and-a-half years away from being available clinically. In the meantime, we’re continuing to run quality-control checks of other steps in our research process to make sure we’re not introducing anything we don’t want to introduce.
In fact, this is a very important time because ours is only one of many stem cell projects that are starting to enter early clinical trials. Although there have been no problems reported with them as of yet, if something did [happen], it would have a huge negative impact on the field and could really slow progress, maybe even delaying the field for a decade. So to me, quality control is cool.
Reference
- K. Bhutani, K. L. Nazor, R. Williams, H. Tran, H. Dai, Ž. Džakula, E. H. Cho, A. W. C. Pang, M. Rao, H. Cao, N. J. Schork, and J. F. Loring. (2016, Feb.). Whole-genome mutational burden analysis of three pluripotency induction methods. Nat. Commun. [Online]. 7, 10,536.