Innovative researchers are employing flexible, rather than rigid materials in combination with new design approaches as part of the emerging field of biomedical soft robotics. The idea is to generate tools that conform to and interact with the human body in a much more natural and lightweight way, providing better treatment options for clinicians and translating into better outcomes for patients.
The applications for soft robotics are wide ranging. For instance, recent publications portray such innovations as soft-material, origami-inspired, artificial muscles with actuators that can lift a thousand times their weight [1], [2]; and personalized-for-the-patient cardiovascular occluders that use inflatable silicone/polyurethane balloons [3]. Other devices are already well into development.
Still, although much progress has been made over the past couple of years in particular, the field of soft robotics is just beginning, according to Conor Walsh, Ph.D., John L. Loeb Associate Professor of Engineering and Applied Sciences at Harvard University and a core faculty member at the Wyss Institute for Biologically Inspired Engineering at Harvard. “This field involves an interesting mix of disciplines, from more traditional robotics people to people who are in the apparel industry (for wearable, external robots) to materials scientists as well as many other disciplines, and we’re just at the start of seeing how the fields converge,” explains Walsh. “One thing that is certain, however, is there are lots of applications.”
From Rigid to Soft
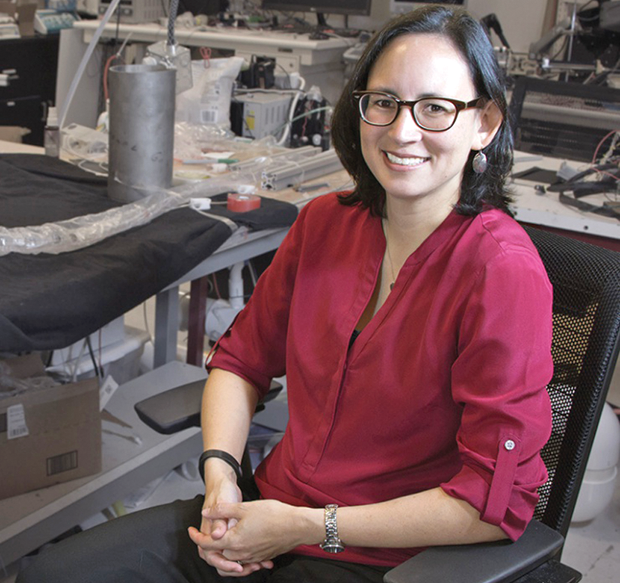
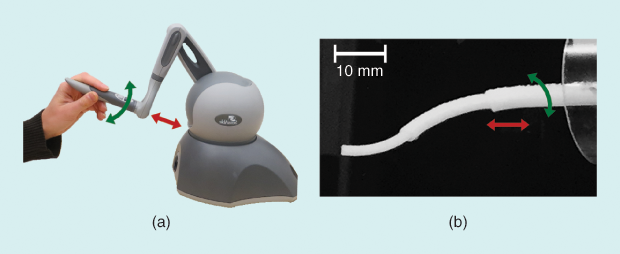
Bringing soft robotics to minimally invasive procedures is a special interest of Allison Okamura, professor of mechanical engineering and director of the Collaborative Haptics and Robotics in Medicine (CHARM) Lab at Stanford University (Figure 1). She began her transition from traditional robotics to soft robotics when she initiated work on a project at Johns Hopkins University more than a decade ago. “We developed this concept of steerable needles, which were not as soft as the current generation of soft robots, but they were very highly flexible, extremely thin needles made of Nitinol, which is a superelastic alloy that can take a lot of strain without breaking,” Okamura says.
She continued that project when she moved to Stanford University in 2011. A few years later, postdoctoral researcher Giada Gerboni led the effort to control the long, thin, flexible needle (Figure 2). “The main objective of our steerable needle was to access tumors that are inside dense organs, such as the liver,” Gerboni states, noting that the tip of the needle can generate heat to ablate a tumor. Current minimally invasive methods utilize straight, nonbending needles that often cannot reach tumors in these organs or, if they can, must be inserted multiple times to ablate the entire tumor. “Since multiple insertions increase risk, the solution was to puncture once and then be able to steer the needle in different directions and to different locations inside the tissue,” she continues.
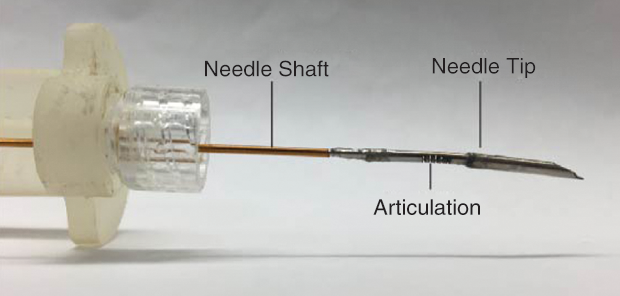
To navigate the flexible needle, Gerboni adds cuts to one side of the needle near the tip that enable the tip to change angle. With that design, the asymmetric forces on the articulated tip cause the needle to curve as it is inserted (Figure 3). Then, using motors located outside the body to spin the needle and assisted by ultrasound imaging to view its position, the needle can be directed in convoluted paths within the tissue (Figure 4) [4], [5].
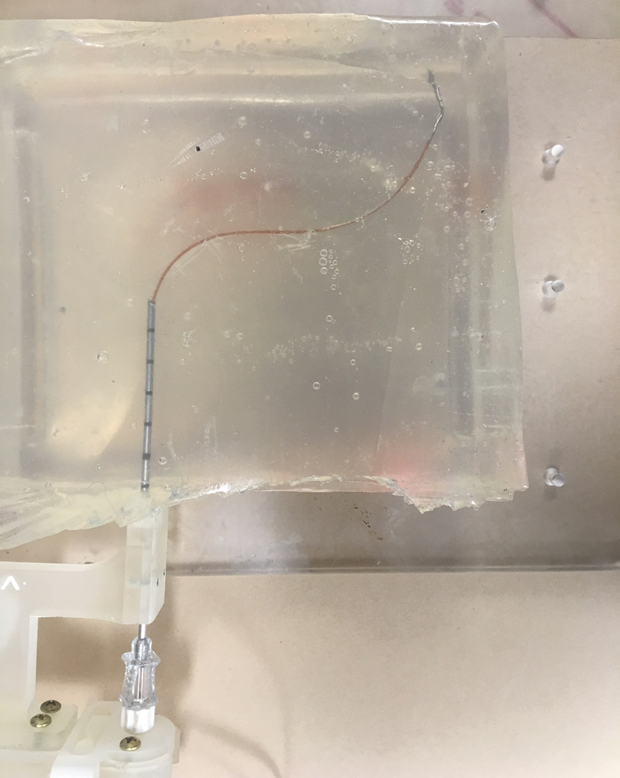
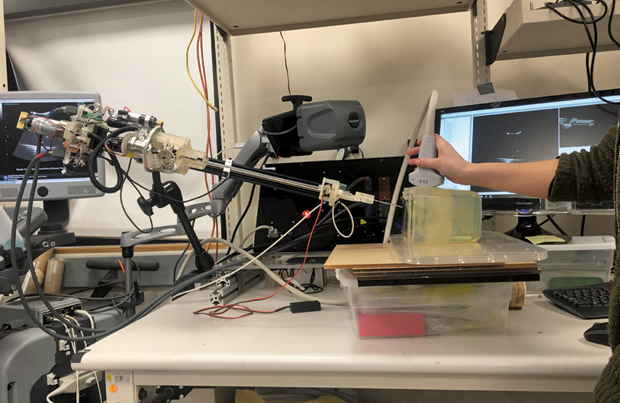
“As of now, the whole system works very well in both the lab and in preliminary pig–cadaver tests, and with a control platform that is made by Ph.D. students. But we hope to turn it into a medical product,” Gerboni remarks. The group plans to conduct live-animal testing in mid-2018 and, if all goes well, hopes to eventually seek a company to take the steerable needle from the bench to the bedside.
Tube Robots
In other work, Okamura’s research group is developing a couple of tube-style robots. One, called a concentric tube robot (Figure 5), comprises a series of flexible tubes, each with a different curvature and diameter so that they can be nested one inside another [6]. The second, called a growing robot, works rather like a latex glove that has had the fingers pushed in; when air or liquids are pumped in, the pressure slowly extends the tubes (or fingers) back out [7], [8].
Both robots utilize external actuators to control the tubes’ extension. The soft material used for the concentric tube robots is polycaprolactone, a biodegradable polyester commonly available for use with 3-D printers. Preoperative imaging can help the clinician determine the best path to a target, and software can automatically compute what the shape of the tubes should be. “We can print a specific set of tubes on the spot, so they can then be attached to the robot and do what is needed for that patient and that procedure,” Okamura says.
She sees concentric tube robots being especially useful in certain areas of the body. While the tissue in solid organs is necessary to support and direct the steerable needle, she says, “the concentric tube robot itself is its own kind of backbone, so it would not only work in extremely soft tissues, such as the brain, but it could also even operate in free spaces and open cavities in the body.”
A concentric tube robot has other advantages as well. One is the diameter of the tubes, which is considerably smaller than that of the rigid tools used in surgical systems today. “We collaborated with a pediatric urologist who was interested in treating kidney stones in very young patients—children who are 7, 8, and 9 years old—and large conventional surgical tools weren’t an option for that patient population,” Okamura explains. The smaller size of the tubes is possible because, like the steerable needle, all of the space-taking motors and actuation are outside the body.
At this point, Okamura’s research group—and especially then-Ph.D. student Tania Morimoto (now at the University of California, San Diego)—developed a complete end-to-end concentric tube system. It includes a virtual environment into which a surgeon can upload medical images, perform a practice run of the operation with the help of a virtual-reality headset, and make any design changes before the tubes are printed. “We have also shown that a surgeon can operate the robot to reach targets in an artificial patient, which is a fake patient made of fake tissues,” Okamura reports. The next step is to test it in animals.
In contrast, the growing robots use a thermoplastic material that has the consistency of a plastic storage bag (Figure 6). Okamura envisions them being used to provide a channel through which medicine as well as other surgical instruments can be delivered [9]. “Unlike traditional catheters that have to be pushed through blood vessels and can cause significant friction, especially when making tight turns, the growing robots don’t have that problem,” Okamura contends. “Instead, material elongates the robot at the tube tip, which means less tissue damage.” Once a tube’s job is done, it is a simple matter to deflate the tubes and pull them out.
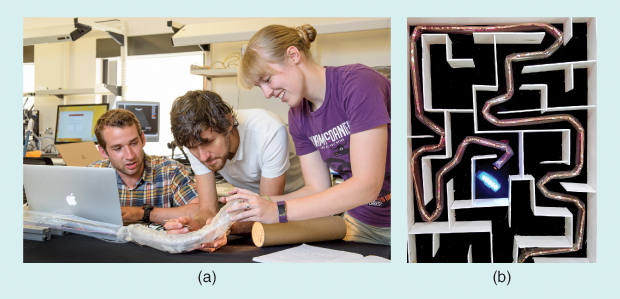
At present, Okamura’s group is pursuing the growing robots for search-and-rescue operations, such as delivering air and water to buried survivors until they can be extracted, while one of her former postdoctoral researchers, Elliot Hawkes (now at the University of California, Santa Barbara), is working on the medical applications. “He has already gotten the diameter of the tubes down to about a millimeter, which is the level where you could start to go through vasculature and into the brain,” according to Okamura. If used for drug delivery, such a system could circumvent the blood–brain barrier, because “you could go in through the arm or leg and grow this tube, making all the necessary turns and going in the right direction through the different branches of the vasculature, until you get to the target, where a strategically placed hole in the tube would precisely deliver the medication,” she says. “There are many different ways to use these robots, and that’s just one example.”
This project is still in its early stages, but the group has published a paper showing proof of the basic concept, and Hawkes is currently continuing this research in at-scale human models before conducting animal studies.
Assistive Heart Sleeve
In a completely different approach to soft robotics, another project is creating a robot designed for patients with end-stage heart failure. Made of a silicon matrix embedded with actuators, it is a soft sleeve that fits over the ailing heart and contracts on command to help the organ pump effectively [10], [11]. The project originated in Walsh’s lab at Harvard and is now continuing in the lab of his former doctoral student Ellen Roche (Figure 7), an assistant professor of mechanical engineering at the Institute for Medical Engineering and Science at the Massachusetts Institute of Technology. She is collaborating with a wide range of mechanical and computer engineers as well as surgeons and surgical residents on this project.

The sleeve’s design includes actuators oriented to mimic the complex motions of the heart, Roche says. “In addition, we can selectively actuate or deactuate certain elements so that we can really tune the heart sleeve to what the patient needs.” To provide that kind of control and precisely assist the heart, the researchers have developed software that monitors the native electrocardiogram (ECG) waves, as well as blood pressure, to trigger the sleeve to pump as much as necessary and exactly where it is required, she describes.
The sleeve’s construction was multilayered. “We made the actuators ourselves from internal balloons that we generally formed and then put inside a braid of mesh and connected. Then we embedded the whole thing in silicon, which was available commercially, to make it into the sleeve,” recounts Roche. The sleeve also incorporates a data-acquisition system that monitors the ECG and hemodynamics waves as well as the performance of the sleeve, a laptop from which the researcher can change actuator timing or other parameters, and a control box that uses information from the data acquisition system and laptop to control the sleeve’s activity. “After multiple iterations of the design, we ended up with a device that works well and can also be surgically implanted and fitted onto very anatomically different hearts,” she adds.
To date, the research group has had success with the sleeve in short-term preclinical models and is now working on miniaturizing the hardware, while also planning longer-term studies to see how the device may function in patients with chronic heart conditions. “Once we get some good long-term data, we’ll hopefully license the technology, partner with someone to move to regulatory approval, and test in humans,” Roche maintains. “That will probably take a couple of years.”
At the same time, Roche is working on another soft-robotics device for drug delivery. “What we have are implantable reservoirs that can be put where you want them to take effect and deliver the drug on demand or slowly release it. We’ll be publishing that soon,” she asserts. “We also have a right ventricular assist device that has been published, and we’re starting up a few more projects that are specific to different diseases, including some congenital heart defects, so we are busy.”
Soft, Wearable Robots
When most people hear “wearable robots,” they think about rigid exoskeletons designed to provide mobility for individuals who are paralyzed, but in Conor Walsh’s lab, the focus is on “all of the people out there who just need a little bit of a boost,” he says. “That might be people who have had a stroke, or who have Parkinson’s or multiple sclerosis, or even just people who are elderly.” The basic premise behind Walsh’s approach is to design and construct innovative and lightweight functional textiles that are worn on the legs, shoulders, or hands to make movement easier and more efficient.
Several projects are under way. In particular, an exosuit is being developed to address weakness in the lower extremities. “Given that these people can already walk, the basic premise is to refrain from overburdening them with any device you put on,” he says. “So in our project, the part that goes on the legs is the textile apparel components that anchor tightly to the calf, thigh, or other site, and power is transmitted via flexible cables so the part on the legs is very lightweight and nonrestrictive,” (Figure 8).
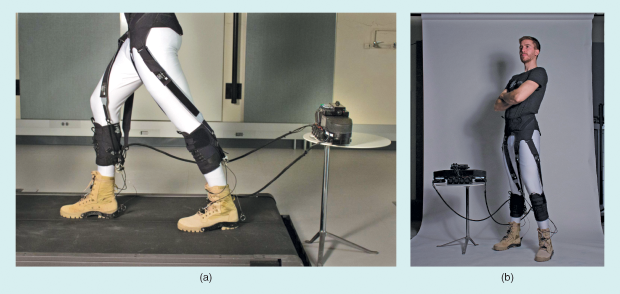
An exosuit for a poorly functioning ankle, for instance, could be anchored on the calf and in a shoe’s insole and include wearable sensors to monitor various parameters of the individual’s gait for analysis by a control algorithm. A cable would run across the ankle joint and up to a waist belt, where an algorithm would activate a motor and associated electronics in an actuation pack. That, in turn, would pull on the cable and cause the proper force to be applied at the ankle joint to assist the patient in walking.
Walsh and his research group have already published a study in Science Translational Medicine [12] showing that the exosuit improved the gait in nine stroke patients. They have also established a collaboration with the medical device company ReWalk Robotics, which has headquarters in Israel, Germany, and the United States. He says that ReWalk will begin a clinical trial this year to investigate the soft exosuit as an assistive device for stroke patients.
To improve a person’s ability to grasp, Walsh’s group is developing soft, wearable robots that are powered by air. “Here, we have a compressor pump or small storage tank of air that will go on a wheelchair or on a tabletop, and we have a soft glove that includes air chambers so that when you inflate those air chambers, it closes the hand or presses the hand, or it lifts the shoulder joint” (Figure 9).
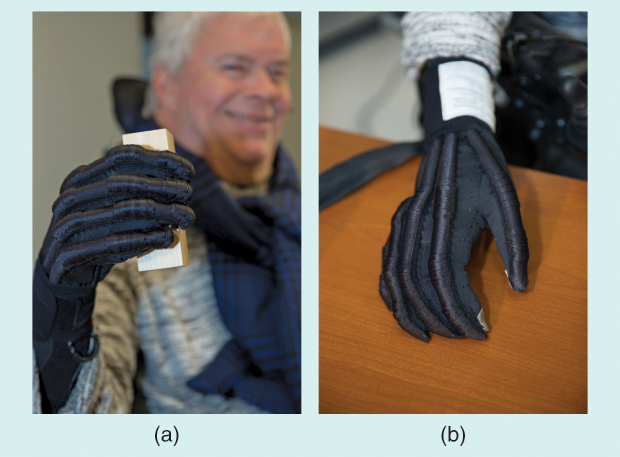
The glove project is at an earlier stage than the exosuit, Walsh says. “We just finished a study in eight spinal cord injury patients with promising results showing improved grasp function, and the glove still needs a little more iteration before it will be ready for commercialization.” In particular, the researchers will continue to optimize the textiles, sensors, and control algorithms to make it very easy for a person to use, and also consider the manufacturing methods that will be required to move the lab-made prototype to a commercialized product.
Wide-Open Possibilities
The overall field of soft robotics may still be in its infancy, but Okamura already sees a bright future. “The medical applications of soft robotics are especially important because we’re often dealing with physical interaction with the human body.” That’s why soft robotics is a good pairing with minimally invasive surgical devices, she says. “Human bodies are flexible, animals are flexible, plant life is flexible, so we need soft devices that are biologically inspired, go in curvy paths, and conform to the natural mechanics of the human body.”
Walsh agrees that opportunities abound. “There’s huge potential in wearables, and while my lab is only looking at two areas, you can think of many areas in rehabilitation, orthopedics, and recovery after injury, where there’s great promise,” he says. “And for implantable devices, you can probably imagine a range of different applications where soft robotics would not only be delicate enough for interacting with tissue, but also could include the ability to release drugs or other therapy, or perhaps be used as surgical tools that could grasp tissue without damaging it.”
He summarizes, “These are all exciting areas, and what we need to do is to think about ‘How do we advance the fundamental science to make it easy for people to think of ways they can adapt soft robotics for different applications in the future?’”
References
- S. Li, D. M. Vogt, D. Rus, and R. J. Wood, “Fluid-driven origami-inspired artificial muscles,” PNAS, vol. 114, no. 50, pp. 13,132–13,137, 2017.
- Brownell, L. (2017, Nov. 27). Origami-inspired muscles are both soft and strong, and can be made for less than $1 press release. Wyss Institute. [Online].
- S. S. Robinson, S. Alaie, H. Sidoti, J. Auge, L. Baskaran, K. Avilés-Fernández, S. D. Hollenberg, R. F. Shepherd, J. K. Min, S. N. Dunham, and B. Mosadegh, “Patient-specific design of a soft occluder for the left atrial appendage,” Nature Biomed. Eng., vol. 2, pp. 8–16, 2018.
- Stanford CHARM Lab. (2018, Feb. 1). Steerable needle goes around obstacles. [Online].
- G. Gerboni, J. D. Greer, P. F. Laeseke, G. L. Hwang, and A. M. Okamura, “Highly articulated robotic needle achieves distributed ablation of liver tissue,” IEEE Robot. Autom. Lett., vol. 2, no. 3, pp. 1367–1374, 2017.
- Stanford CHARM Lab. (2018, Feb. 1). Design of a compact actuation and control system for flexible medical robots. [Online].
- Stanford CHARM Lab. (2018, Feb. 1). Vine robot 2017. [Online].
- Stanford CHARM Lab. (2018, Feb. 1). Science robotics growing robot video. [Online].
- E. W. Hawkes, L. H. Blumenschein, J. D. Greer, and A. M. Okamura. (2017, July 19). A soft robot that navigates its environment through growth. Sci. Robot. [Online]. 2(8).
- E. Roche, M. Hovarth, I. Wamala, A. Alazmani, S. Song, W. Whyte, Z. Machaidze, C. Payne, J. Weaver, G. Fishbein, J. Kuebler, N. Vasilyev, D. Mooney, F. Pigula, and C. Walsh, “Soft robotic sleeve supports heart function,” Sci. Transl. Med., vol. 9, no. 373, 2017.
- SciNews. (2018, Feb. 1). Soft robot helps the heart. [Online].
- L. Awad, J. Bae, K. O’Donnell, S. De Rossi, K. Hendron, L. Sloot, P. Kudzia, K. Holt, T. Ellis, and C. Walsh, “A soft robotic exosuit improves walking in patients after stroke,” Sci. Transl. Med., vol. 9, no. 400, pp. eaai9084, 2017.



