Technology that allows the human brain to communicate with an external device can help patients with some of the most severe neurological issues
Operating a drone, playing video games, or controlling a robot simply by thinking are exciting applications of brain–computer interfaces (BCIs) that pave the way for more mind-bending breakthroughs. Crucially, BCIs, which enable the brain to exchange signals with an outside device, also represent a powerful tool to restore movement, speech, touch, and other functions to patients with brain damage. Despite recent progress in the field, technological innovation is needed and plenty of scientific and ethical questions remain unanswered. Still, researchers say BCIs hold great promise for patients with the most severe impairments—and that major breakthroughs are within reach.
Innovation and tradeoffs
Broadly, a BCI (sometimes called a brain–machine interface, or BMI) measures brain activity (either electrical, magnetic, or metabolic), transmits those signals to an external device, and then initiates an action [1]. BCIs are already being developed and used to restore communication and motor functions to people with amyotrophic lateral sclerosis (ALS), spinal cord injury, stroke, and locked-in syndrome; to help amputees control robotic arms; and more. Most BCIs rely on electrodes to collect data on electrical currents and potentials in the brain, although magnetic, acoustic, and infrared technologies also exist. Compared to electrodes placed on the scalp, implanted BCIs are much closer to the neurons they aim to record and thus provide a cleaner signal that is easier for a computer to decode and respond to. But they carry additional challenges and risks, including specialized surgeons and the possibility of infection.
“With every solution, there’s some sort of tradeoff,” said Shadi Dayeh, Ph.D., a professor of electrical and computer engineering at the Jacobs School of Engineering at the University of California, San Diego (UCSD). “More invasive devices, such as those that penetrate the brain tissue, offer higher resolution.”
The Utah array, which contains 100 electrodes and penetrates about 1 millimeter into the cortex has been at the heart of many breakthroughs in the field so far. “We’re getting great information by using several of these arrays spread across the cortex,” said Sydney Cash, M.D., Ph.D., an associate professor of neurology at Harvard Medical School who is part of the BrainGate consortium. “But the quantum leap we’re looking for is moving to thousands of channels—perhaps a 50-fold increase in the number of neurons we’re recording from.”
That quantum leap looks increasingly possible, now that the semiconductor and telecommunications industries have created high-density electrode arrays that can be produced at a relatively low cost. Dayeh recently led the development of a new BCI that borrows fabrication techniques from display screens. The device contains more than 4,000 channels and has flexible backing that can conform to the brain’s 3D surface [2].
Covering a larger area of the brain with a thin, flexible BCI could ultimately allow scientists to decode brain activity using waves, rather than local electrical potentials. Dayeh and his team first observed these signature patterns among patients in the operating room at UCSD. Using a BCI with a few thousand channels, they had patients open and close their hands, then detected waves of brain activity that bounced back and forth between the motor and sensory cortices to coordinate the motion. “This offers an advantage over existing technology, because if one or more contacts on the interface go bad with time, we would still be able to capture neurological function,” he said.
Restoring movement and speech
Alongside the technological innovation that aims to advance BCIs, researchers still have many scientific questions about how to decode signals from the brain, including about how communication works between various regions. “We still have a lot to learn about how the nervous system works—how do neurons talk to each other and what are they saying?” Cash said.
Researchers across the field are making progress on that front. Using Utah arrays, Jennifer L. Collinger, Ph.D., an associate professor of physical medicine and rehabilitation and research operations director of the Rehab Neural Engineering Labs (RNEL) at the University of Pittsburgh is working with her team to restore upper limb function to patients with paralysis resulting from a chronic spinal cord injury. They have demonstrated that participants can use a BCI to orient a robotic arm and pick up and move objects (Figure 1).
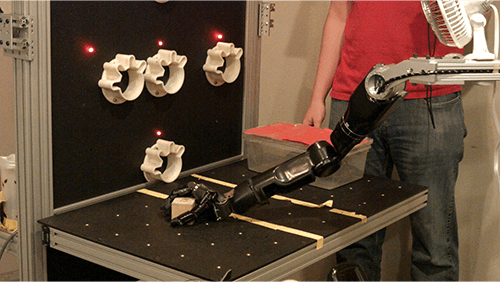
Figure 1. Stimulating the somatosensory cortex with a BCI improves accuracy when controlling a robotic limb. (Image courtesy of UPMC/Pitt Health Sciences.)
“We’ve also shown that adding sensory feedback can improve the ability to grasp and interact with objects quite dramatically,” she said. By implanting electrodes in the somatosensory area of the brain, the BCI can generate sensations that feel as if they’re coming from a participant’s hand, a key source of feedback we use when manipulating objects [3]. The sensory feedback enabled a person with tetraplegia to double the speed of movements with a robotic limb, largely due to less time spent trying to grasp objects. Collinger and her colleagues are now exploring how stimulating the somatosensory cortex can convey subtle details about pressure and contact location to further support dexterous hand movements (Figure 2).

Figure 2. Jennifer L. Collinger, Ph.D., tests a BCI with a participant in the Rehab Neural Engineering Labs. (Image courtesy of UPMC/Pitt Health Sciences.)
Also at RNEL, Lee Fisher, Ph.D., is using a BCI to stimulate the spinal cord of upper or lower limb amputees who are using a prosthesis. By stimulating lateral parts of the spinal cord, he and his team have helped restore sensation from missing limbs and can even control the intensity and location of those sensations. That has helped improve balance and gait in lower limb amputees relying on prosthetics and, though the mechanism is not fully understood, has even led to a clinically meaningful reduction in phantom limb pain among participants [4].
BCI researchers are also continuing to pioneer ways for paralyzed people to communicate with the outside world. Edward Chang, M.D., a neurosurgeon at the University of California, San Francisco, developed the first speech “neuroprosthesis” that can decode full words from the brain activity of a person who cannot speak due to an injury or neurological disease [5].
“By recording brain activity during speech and correlating it with the kinematics of mouth movement, Dr. Chang and his team developed a way to decode and reproduce speech without a patient even opening their mouth,” Dayeh said.
For people with even more significant impairments, such as ALS, Collinger is helping test another method of restoring communication. That project, led by Douglas Weber, Ph.D., of Carnegie Mellon University, and David Lacomis, M.D., of the University of Pittsburgh, is a clinical trial of a new and different BCI: the Stentrode by Synchron, one of several companies that develops BCIs. The device is essentially a stent covered with electrodes, which can be implanted in one of the brain’s blood vessels with a catheter, rather than a more invasive brain surgery.
“You’re a little further away from the neurons than if you implant an electrode in cortex,” Collinger said, which limits the recording potential. But for people with severe communication impairments, even the ability to give two discrete commands could be incredibly valuable.
Centering patient needs
In addition to the scientific and technological advances underway to make BCIs safer and more effective, significant ethical, regulatory, and logistical challenges also exist. On the ethical side, one of the biggest concerns is regarding free will. For example, deep brain stimulation—which has been used to treat obsessive-compulsive disorder, depression, and anorexia—can impact both mood and personality [6]. But can a patient reflect on how a BCI has changed their mind? And if not, can they ethically consent to continue receiving treatment?
For these and other reasons, including privacy concerns about arguably the most sensitive protected health information, regulators are stepping in with force to ensure that devices are safe, effective, and used appropriately. While crucial, such regulations add a layer of complexity for groups studying BCIs, Cash said.
Looking forward, researchers agree that patient needs should be a major driver of development. For one, thought should be given to rolling out devices in a way that’s both commercially viable and able to reach eligible patients in an equitable way. As BCIs are increasingly used at home for daily living, the field will also need to ensure that patients can rely on their devices in less controlled environments, according to Collinger. At home, for example, patients may be more likely to face fatigue, pain, or waning attention—and new BCIs should be designed with those conditions in mind. “As we’re getting closer to having operational systems, we need to be getting more and more input from the patients and their caregivers,” Cash said.
In the meantime, engineers, researchers, and clinicians continue to tackle the challenge from all angles with a healthy dose of enthusiasm. “We’re only tapping on the surface of what could be done with BMI with existing technologies,” Dayeh said. “We should celebrate the successes that we have so far, because they are life-changing for patients. But this is only the tip of the iceberg.”
References
- L. Nicolar-Alonso and J. Gomez-Gil, “Brain computer interfaces, a review,” Sensors, vol. 12, no. 2, pp. 1211–1279, Jan. 2012, doi: 10.3390/s120201211.
- Y. Tchoe et al., “Human brain mapping with multithousand-channel PtNRGrids resolves spatiotemporal dynamics,” Sci. Transl. Med., vol. 14, no. 628, Jan. 2022, Art. no. eabj1441, doi: 10.1126/scitranslmed.abj1441.
- S. Flesher et al., “A brain-computer interface that evokes tactile sensations improves robotic arm control,” Science, vol. 372, no. 6544, pp. 831–836, May 2021, doi: 10.1126/science.abd0380.
- A. Nanivadekar et al., “Spinal cord stimulation restores sensation, improves function, and reduces phantom pain after transtibial amputation,” medRxiv, Sep. 2022, doi: 10.1101/2022.09.15.22279956.
- D. Moses et al., “Neuroprosthesis for decoding speech in a paralyzed person with anarthria,” New England J. Med., vol. 385, pp. 217–227, Jul. 2021, doi: 10.1056/NEJMoa2027540.
- L. Drew, “The ethics of brain-computer interfaces,” Nature, vol. 571, pp. S19–S21, Jul. 2019, doi: 10.1038/d41586-019-02214-2.