Every year, Doris’s primary care physician sends her to see a neurologist to check on her hand tremor, which has increasingly worsened over the past 20 years. Year in and year out, the neurologist asks her to draw a circle on a piece of paper. “The doctor looks at it, says ‘Hmm,’ and sends me home,” Doris explains, adding that she gets no treatment, no recommendations, nothing except a request to schedule next year’s appointment.
Doris’s experience is all too typical. “Still today, it remains very common for primary care practitioners to say to patients, ‘Oh, you have essential tremor, but it’s not going to kill you, so you just have to learn to live with it,’” notes Kelly Lyons, Ph.D., president of the International Essential Tremor Foundation and director of research and education at the Parkinson’s Disease and Movement Disorder Center at the University of Kansas Medical Center (Figure 1). “We’re trying really hard to break through the barriers to make physicians aware that there are treatment options, and there are things we can do to help people with essential tremor.”

Such advances take on special significance when the prevalence of essential tremor is factored in. A recent estimate placed the number of Americans who have essential tremor at about 7 million, or more than 2% of the U.S. population [1].
High-tech care today includes deep-brain stimulation (see “Beyond Deep-Brain Stimulation”), which received approval from the U.S. Food and Drug Administration in 1997 to treat essential tremor, as well as many more recent technologies that reduce the tremor itself or help negate the symptoms of tremor.
[accordion title=”Beyond Deep-Brain Stimulation”]
One of the ways to help patients is to get to the crux of essential tremor: the ventral intermediate nucleus (VIM) of the thalamus. Located deep in the brain, the thalamus controls muscle movement and coordination. Although the exact cause of essential tremor is still unknown, inactivation of the VIM nucleus does dampen tremor. Deep-brain stimulation (DBS) accomplishes this by continuously zapping the VIM nucleus with electrical impulses. A pacemaker-type device implanted in the chest sends impulses via wire to electrodes implanted in the VIM nucleus, interrupting its normal electrical activity and reducing the tremor.
“I would say that DBS has probably had the biggest impact on the treatment of essential tremor, and many patients get up to a 90% reduction in tremor, which can change people’s lives,” notes Kelly Lyons, Ph.D., president of the International Essential Tremor Foundation and director of research and education at the Parkinson’s Disease and Movement Disorder Center at the University of Kansas Medical Center.

Medtronic, a public limited company headquartered in Dublin, Ireland, first introduced DBS for essential tremor almost two decades ago and is currently building on that technology. It has developed the investigational Activa PC+S system (Figures S1 and S2), now being used for research purposes, which adds a research component employing sensors, a new brain–machine interface (BMI) chip, and an interactive algorithm toolkit to allow study of the relationships between the stimulation and a patient’s symptoms, according to Tim Denison, senior director of core technology at Medtronic. Developing the system required algorithms that could discern microvolt signals from the neural networks, a particular challenge given that the DBS is simultaneously delivering impulses that are between 1 and 2 V (six orders of magnitude larger). “It’s actually a lot like building a duplex [two-way] radio, where you’ve got to worry about your transmitter jamming your receiver,” Denison says. “A lot of the design problems of a bidirectional radio system were applied to this neural interface and went into the sensor design.”
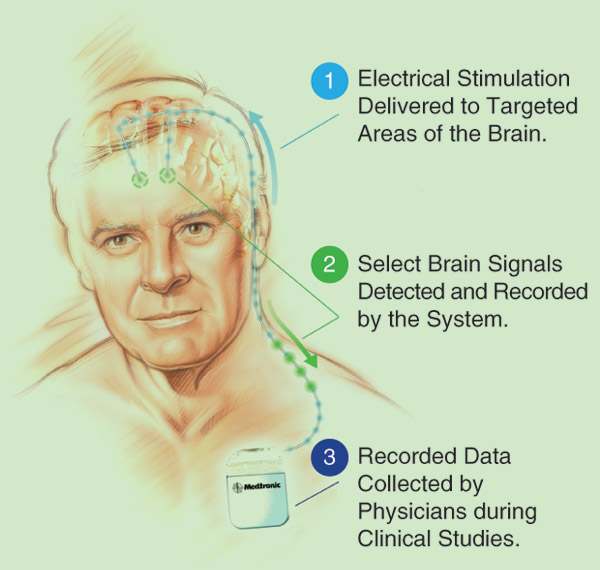
“One of the most important design constraints for Activa PC+S,” Denison explains, “was that we have to maintain baseline expectations with therapy, so there’s no compromise expected by the patient, and then we layer this research toolkit on top of it. The toolkit gets ‘woken up’ by the investigators, so they can do their scientific exploration. Then they power down the toolkit, and the device goes back to looking, for all intents and purposes, like a classical DBS stimulator.”
A team of researchers at the University of Washington is investigating whether they can use the BMI functionality to optimize patient therapy [1], Denison adds. Today, most patients receive a fixed pattern of DBS, and any adjustments to that pattern require either a clinician or the patient to make these manually using a telemetry module. “With the BMI advances, the UW team is exploring how the Activa PC+S might provide more of an adaptive system with a pattern that uses network activity to determine the real-time needs of the patients,” he explains.
The intent of an adaptive system is to improve treatment—and prolong the device’s battery life—by delivering electrical impulses only when the patient needs them, explains Denison. While investigator studies are moving forward in the United States to develop the most compelling algorithms, he says Medtronic hopes to bring Activa PC+S to the clinic in the coming years.
Another company is approaching the thalamus differently. InSightec, which has corporate headquarters in Israel, is developing a system called ExAblate that uses focused ultrasound to destroy the VIM nucleus. Before DBS was approved, surgeons would lesion or ablate the VIM nucleus by cutting an opening in the skull, then inserting and energizing a probe to burn away the tissue. “When targeted properly, it works extremely well,” according to Richard Schallhorn, vice president of neurosurgery for InSightec. There were challenges, however, and the biggest was targeting only the VIM nucleus. “If you destroyed adjacent structures, you could have side effects that affect sensory perceptions, typically in the hands and face, or perhaps balance, gait, or even speech.”
By using focused ultrasound, ExAblate eliminates the need for the skull-opening surgery required for DBS or for traditional ablation techniques. However, it retains the ability for pretesting the lesion noninvasively, so it allows precise destruction of the VIM nucleus while leaving adjacent tissue unharmed, he says. “What we’re doing preserves several key advantages of invasive surgery but allows it noninvasively so that it is accessible to a much broader group of patients.”

ExAblate is a helmet that is equipped with 1,024 individually controllable ultrasound transducers and that is attached to the bed of a magnetic resonance imaging (MRI) scanner (Figure S3). “What we’re doing is taking the ultrasound beams from those 1,024 transducers and aiming them at a common central point. At that focal point, the combined energy of the thousand-plus beams can bring the temperature of the brain up over 60 °C, which is enough to permanently destroy tissue,” Schallhorn explains.
The big hurdle was the skull. “When each ultrasound beam penetrates the skull, it is reflected and refracted by the bone, so the key was how to refocus all of the beams on a central point once they’ve passed through the skull, and that is really the big engineering challenge that we’ve accomplished,” Schallhorn says. InSightec did so by developing a focusing algorithm that accesses a high-resolution computed tomography scan of the skull, compensates for the local bone thickness, and adjusts the phase of each beam so the beams intersect. According to Schallhorn, “With this technology, we can create lesions that can be as small as 2 mm in size and can be accurate to within 0.5 mm.”
As of February 2016, the worldwide clinical trial of ExAblate has ended, and the U.S. Food and Drug Administration is reviewing results, Schallhorn says. He expects it to be commercially available in 2017.
He views this technology as a good option for patients who want to treat their tremor, but with an alternative to DBS. “There is no really satisfying medication that treats this condition well, so we believe focused ultrasound will be potentially attractive to the many thousands of patients who do not currently want to seek the surgery associated with DBS.”
References
- M. Guiden. (2015, Apr. 14). UW among select universities to use investigational Medtronic device, advance research into brain activity. UW Today [Online].
- Insightec, Ltd. (2015, Oct. 22). Insightec submits pre-market application for FDA approval of ExAblate Neuro for treating ET [Online].
[/accordion]
Technologies for hand tremor are particularly needed because, although essential tremor sometimes includes shaking of the head and the voice (symptoms that many people recall as afflicting actress Katharine Hepburn), the most common complaint by far is hand tremor, Lyons explains. In fact, about 90% of patients with essential tremor have uncontrolled shaking that affects the upper extremities, usually both hands, and the tremor often becomes pronounced as soon as the person tries to do something, whether it is moving a computer mouse, raising a spoonful of food, or buttoning a shirt. “In more severe cases, it can keep people from being able to perform their own activities of daily living or to care for themselves, because it is so disabling,” adds Lyons.
Even patients with less-severe tremor find it very disruptive. According to Lyons, “There’s an embarrassment factor, whether it’s going to a movie and shaking while you’re trying to eat your popcorn so you end up throwing it, or eating your soup at a restaurant and it’s flying off the spoon.” This loss of dignity causes many people to stop going out in public, which leads to social isolation and often depression, she notes.
Fortunately, however, more and more researchers are turning their attention to essential tremor. This extends beyond deep-brain stimulation, which—although very successful— is not for everyone. “It is brain surgery, so there is always the inherent risk of hemorrhage or stroke or even death, and even though that’s a very small percentage, it can be a risk not all patients are willing to take,” Lyons says. “The International Essential Tremor Foundation has done surveys and gotten patient opinion on deep-brain stimulation, and we’ve found that while it may be very successful for them, there’s a proportion of people who are just not willing to do it.”
With new technologies now available or coming to market, this group of patients now has a growing number of choices.
Tremor-Fighting Flatware

One product that has been getting a good deal of notice since its release in 2014 is a computerized eating utensil that compensates for hand tremor and steadies the utensil sufficiently so that many patients can regain the ability to feed themselves (Figure 2). Called Liftware [2], the utensils look much like regular spoons or forks. “We designed it that way on purpose. We wanted to hide all the technology away from the user so it was just as simple as can be to use, even though there’s a pretty complicated system inside,” notes company founder Anupam Pathak.
Any of the utensil attachments—a spoon, a soup spoon, and a fork—can snap into the handle, which is where the technology lies. Sensors detect the user’s hand movements, whether they are intended movements (lifting the utensil to the mouth, for instance) or unintended movements associated with tremor. The company, based in Mountain View, California, developed a variety of different algorithms that distinguish between the two different types of motion by taking into account certain features, such as the frequency of unintended versus intended movements, Pathak explains. A feedback controller sends commands to two actuators in the handle that move the utensil up and down or left and right.
For this device, both function and form were critical (Figure 3). “It wasn’t enough just to cancel the unintended motion. We also wanted to make it feel to the user like they were still using a spoon, and that required additional design and algorithms,” he says, adding that patient insight was indispensable. “We met with patients over a couple of years, coming back to the lab, changing things, going back to get their input again, and finally shaping something that has turned out to be very useful.”

Although Pathak can’t go into detail for proprietary reasons, he mentions that Liftware is working on additional attachments, including “some for personal hygiene and grooming,” and is also developing devices for other disorders that cause uncoordinated movements. “Once we started in this area, a lot of patients and other people have approached us looking for help, and we are very much focused on being able to do what we can in that broader sense.”
Steadying Gloves
Across the Atlantic, a team of students also tackling essential tremor is well on its way to a generating a new product. The project started when Faii Ong, a medical student at Imperial College London, met a 103-year-old patient with essential tremor. “She looked at me and said, ‘Will you take care of me?’ I simply didn’t know how to respond, as her memory was limited to several minutes, and I didn’t know if I could truly do anything for her. It was a poignant moment that got me thinking about tremor.” He jotted down the thought in a notebook that already had a long list of other things he noticed in the hospital that could use some innovation: “When I had a little bit of time, I ranked all of them, and the tremor issue came out on top.”
That’s when he called on a few friends who were studying engineering to help with his idea of developing a tremor-canceling glove, ultimately named the GyroGlove [3]. They looked at everything from “rubber bands and weights to exotic robotic systems and magnetic fluid dampeners,” but decided that a gyroscope was the most elegant solution, Ong says (Figure 4). “Gyroscopes counteract tremor proportionally and exceedingly smoothly, and that’s the reason why we went with spinning gyroscopes.”

Preliminary testing with patients has had promising results, he notes. “We have a video of a 71-year-old lady with severe essential tremor, and on a good day she can barely use both hands to hold a bottle of water. We strapped on our weakest prototype—that was from July 2015—and even with that, she was able to simulate drinking from a bottle with one hand. The glove reduced the displacement of her palm quite significantly.”
Since then, the glove has taken on a more stylish look, and the gyroscope is much smaller—but twice as powerful (Figure 5). In miniaturizing the gyroscope, which spins at 20,000 rpm, the team had to ensure that it was perfectly balanced. “With the assembly, the motors, and everything else, an unbalanced disk is very noisy, so we will require costly precision equipment to balance the system,” Ong says.
Today, they are hard at work refining the system, with a focus on better controlling the orientation of the gyroscope in response to the patient’s movements. At the same time, the team is planning formal clinical trials so the GyroGlove can make it to market by the end of the year.

tactile-Film Exoskeleton
Researchers in Taiwan and Japan are also collaborating on technology for essential tremor. A group at Taiwan’s Industrial Technology Research Institute (ITRI) has joined with teams at Japan’s Waseda University (led by Prof. Masakatsu G. Fujie) and Kikuchi Seisakusho Company, Ltd., on a tactile-controlled upper-limb exoskeleton (Figure 6).
Called the Higher Sensitivity Tactile-Film System for Wearable Orthosis (HSTS), the externally worn device incorporates sensor cells in a novel “tactile film” that lies on the inner side of the orthosis near the wrist [4]. “The sensor cells are basically resistors that vary when mechanical strain is applied,” explains Jui-Yiao Su, research manager at ITRI’s mechanical and systems research laboratories. Combined with a data-acquisition circuit box and monitoring/image-process software, the HSTS interprets the user’s movements by reading pressure variations between the arm and the orthosis—even through clothing—and mechanically suppresses tremor while allowing for voluntary movement.
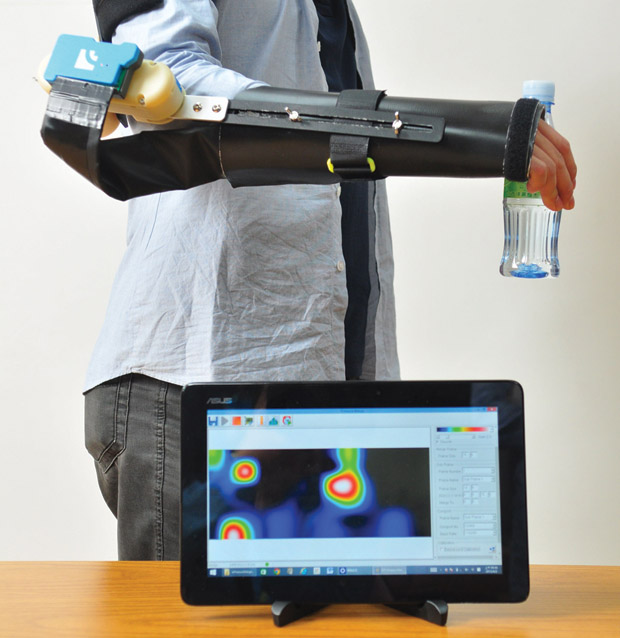
The researchers are now developing the next-version device for preclinical studies and evaluations in Taiwan and Japan. Su remarks, “It is very likely that in the next two years we will produce an orthosis that is built to understand the wearer’s intentions and then to perform adequately.”
Making a Difference
All of these devices and technologies share the same goal: to improve the lives of people who have essential tremor. “The beautiful thing about the whole story of Liftware is that when we first started working on essential tremor, patients were very receptive to the fact that someone was recognizing the condition and dedicated to working on ways to help,” says Pathak. As they moved forward with the project, he says it became clear just how common and how devastating essential tremor is, which reinforced their desire to help.
With the technologies that are already available and new technologies being investigated, patients have an increasing number of options to treat the condition or to dampen the symptoms of essential tremor. Dr. Lyons believes that the biggest obstacle now is getting the word out: “That awareness piece is so important in the professional and the lay community so that people can 1) get the right diagnosis, 2) get treated, and 3) hopefully become part of new research studies to advance the medications, devices, and surgical therapies that may be successful treatments for essential tremor.”
She adds, “There’s definitely a new interest in the field, and several companies are becoming involved in developing new technologies and treatments for essential tremor. That’s very exciting.”
References
- E. D. Louis and R. Ottman, “How many people in the USA have essential tremor? Deriving a population estimate based on epidemiological data,” Tremor Other Hyperkinetic Movements, vol. 4, p. 259, Aug. 2014.
- Liftware. [Online].
- GyroGlove. [Online].
- Industrial Technology Research Institute. (2015, Fall). Higher Sensitivity Tactile-Film System for Wearable Orthosis (HSTS). ITRI Today [Online].



