Joint replacement and other orthopedic surgeries are the perfect venue for new robotic technologies
Robotic technologies are already becoming part of joint replacement operations in many hospitals, but the need for research groups to come up with both small and large innovations remains great, according to Harpal “Paul” Khanuja, M.D., chief of joint replacement surgery for Johns Hopkins University School of Medicine (Figure 1), and Daniel Wiznia, M.D., an assistant professor of both mechanical engineering and materials science in the Yale University School of Engineering, and the director of technology and innovation in the Yale Department of Orthopedics (Figure 2).

Figure 1. Harpal “Paul” Khanuja, M.D., chief of joint replacement surgery for Johns Hopkins University School of Medicine. (Photo courtesy of Harpal Khanuja.)
When asked which research areas could have a big impact on robotic knee and hip replacements in particular, Wiznia said, “One big focus should be on improving personalized medicine, so how do you really customize the implants, the surgery, the technique, and the positioning of the components for each patient because each patient’s anatomy is different and unique. And then there’s implant design, robotic 3D planning, and perhaps materials innovation.”

Figure 2. Daniel Wiznia, M.D., an assistant professor of both mechanical engineering and materials science in the Yale University School of Engineering, and the director of technology and innovation in the Yale Department of Orthopedics and the co-director of Yale University’s Master’s Program in Personalized Medicine and Applied Engineering (seas.yale.edu/pmae). (Photo courtesy of Daniel Wiznia.)
These areas—and more—are waiting for research groups to explore, Khanuja said. “I’m very excited about the potential, and I’m convinced that in the next 10 years, robotic technologies will become a mainstay of what we do.”
Surgical tech today
At present, the American College of Rheumatology estimates that 790,000 total knee replacements and more than 450,000 hip replacements are performed annually in the United States [1]. In projecting forward, a recent study based on U.S. Medicare data forecast that total hip replacements will increase 176% by 2040, and 659% by 2060; and total knee replacements by 139% by 2040, and 469% by 2060 [2].
Technologies in use for joint replacements today are mainly focused on what Khanuja called “fancy navigation,” or using imaging and navigation to help guide the surgeon preparing the bones for hip and knee replacements (Figure 3). “The one thing about orthopedics that lends itself really well to robotics is bones are fixed structures that aren’t moving like a heart or deforming like soft tissue, and the anatomy can be pretty well-defined with imaging,” he explained.
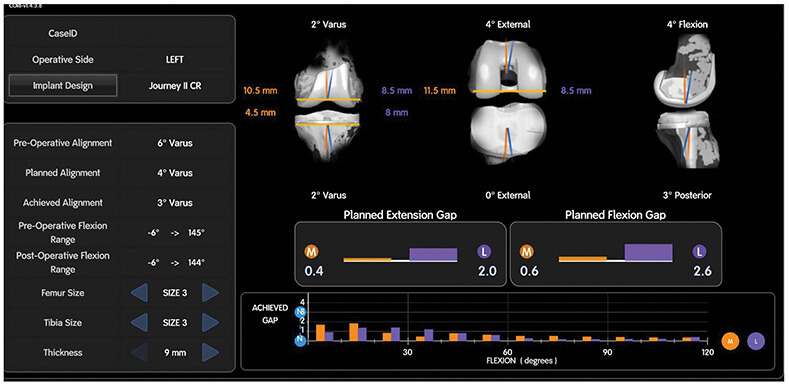
Figure 3. Imaging data can be used to align the knee-replacements implants precisely and balance the ligaments. This data was gathered during a recent surgery conducted by Khanuja and his surgical team. (Image courtesy of Harpal Khanuja.)
Some of the current navigation systems employ a presurgical computed tomography (CT) scan of the patient. “This allows the surgeon to create a 3D model of the bones, and virtually implant the components on the computer before the surgery,” Wiznia described. “Then during the surgery, the surgeon collects additional ligament-balancing data to make adjustments to that model on the computer, and in that way it helps the surgeon to accurately position the components in 3D space.” Other “imageless” systems are also available, and may begin with an X-ray as a basis, and then construct a 3D image as the surgeon runs a sensor-equipped probe over the bone surfaces during surgery.
The images can also be used to assist with robotic instruments. “One of the system designs robotically puts the cutting jig in place based on the coordinate systems and the location of the bones to be cut, whereas I would normally put the jig on myself. It’s really more navigated robotic alignment of your jig than it is a robot doing the cutting. But this is what we call robotics,” Khanuja said. Another system also aligns the saw using computer navigation and allows the surgeon to make the cut.
Wiznia noted that the robot assistance is just that: assistance. “Think of the robot as a very precise measuring system that is providing the surgeon with a lot more information, so that the surgeon is more accurate, but the surgeon does the entire surgery. The robot is not conducting the surgery autonomously.”
Another benefit with new technology is the information it is providing, Khanuja said. “For a knee replacement, what’s really important is balancing the ligaments around the knee, and you can do it somewhat with conventional instruments, but it’s really how everything feels to the surgeon.” With updated software and navigation, tools that collect precise data about alignment and ligament balance will allow for follow-up retrospective analysis (Figure 3). With this data combined with patient outcomes, he said, surgeons will have a much clearer understanding of the optimal placement.
That information is extremely important for many reasons. Proper alignment means less wear and tear on the implants so they last longer, but more importantly, allow for better function, Khanuja said. “If I misalign someone’s knee, they may not walk straight, or they may not get their full range of motion,” he remarked. “On the hip side, proper alignment means less risk of dislocations, and getting the legs the same length, which is an issue that we have. I’ve been doing these surgeries for 20 years, and one thing we’re studying more than ever and understanding better is the relationship of the hip and spine and how they work together, and companies are now developing preoperative robotic models to help with that.”
Surgical tech tomorrow
Although less than 15% of total knee and hip replacement surgeries use these newer technologies [3], Khanuja and Wiznia expect that percentage to rise as more hospitals adopt them and surgical teams become more comfortable using them, and additional data is collected to show improvements in patient outcomes, such as the need for fewer corrective surgeries and longer-lasting implants, and particularly as new advances surface.
Wiznia’s own research group has been doing work in this area. “With robotic knee replacements, I’ve been examining the ability to balance a knee more accurately, so using a robot to make sure the implants are properly positioned and that the ligaments are tensioned properly,” he said. For the latter, they gather such measures as how well the patient can bend the knee, plus patient opinion on whether the “new” knee feels natural kinematically and balanced biomechanically.
Another project in Wiznia’s lab involves ways to reduce the risk of dislocation in hip replacements by conducting preoperative 3D modeling of patients sitting in a chair, walking up a flight of stairs, or doing any number of activities of daily living, and accessing retrospective patient outcome information. “If you know someone who has had a joint replacement, they are often told not to cross their legs, bend down, or kneel on the floor after the surgery, and we give patients a lot of those precautions because of the risk of dislocation. Using robotics, we’re able to virtually in 3D simulate the patient in all of those positions, and see whether the implants are at risk of dislocation based on how they are rotating,” he explained.
Wiznia is also contributing to other Yale collaborative projects, such as integrating robotic data being measured during the surgery and feeding it into virtual and augmented reality 3D glasses for the surgeon. The idea is to provide guidance to align bone-cutting instruments and position implant components precisely, but to do so without overwhelming surgeons with superfluous information. This balance is where multidisciplinary teams are critical. “Here at Yale University, we have a very strong relationship between the School of Medicine and the School of Engineering, and between physicians and biomedical and mechanical engineers who are robotic experts.” Along those lines, Yale kicked off a “Personalized Medicine and Applied Engineering Master’s Program” that draws medical, dental, and engineering students, and gives them hands-on experience working with orthopedic companies on their robotic systems.
Utilizing many of these imaging technologies, Wiznia has also co-developed a new 3D navigated surgical technique to treat avascular necrosis of the femoral head, and co-lead’s Yale School of Medicine’s Avascular Necrosis Program. The goal of the technique is to conduct a personalized surgery and limit the morbidity that is associated with traditional techniques [4].
Underlying all of the technology is the all-important data it is collecting for retrospective analysis, reiterated Khanuja. “I think it’s going to be like everything with machine learning and information: we’ll be able to see exactly how we should put this knee in this type of person. Right now, we’re putting them in the way we think, but once the computer can tell us where to do that, that’s where the real advances come in,” he said.
Another area that Khanuja would like to see more researchers focus is in tactile feedback. For example, he looks forward to robotics that can sense the changing texture from the inside to outside of bone when making cuts, or steadily press hip implants into the proper place rather than the currently used impacting method. “In my world of orthopedics, which is very hard structures, I think things that can sense the difference between tissues along with the forces of impaction are really going to add to what we’re doing now,” he said.
Khanuja speculated that tactile feedback will be a big step toward partially autonomous joint replacement surgery: The surgeon will still be present and managing the operation, but robotics systems will be able to accomplish many of the tasks. “As an example, with mechanical jigs for knee replacements, I first make sure the angle aligns from the bone canal, put on the jig, and cut the distal femur. Then, I measure the distal femur, make holes and reposition the jig, and make four other cuts on the femur, which fit the femoral component,” he described. “I believe that can be done better down the road if I can just line things up, push a button, and the computer takes over. That’s how these surgeries will become more cost- and time-efficient.” He noted that this kind of partial automation will also help make joint replacements more consistent from surgeon to surgeon and hospital to hospital.
Joint replacement and other orthopedic surgeries are the perfect venue for new robotic technologies, Khanuja asserted. “Because the bones are hard, fixed structures, I do think this will be the first area to have more automation.” He added, “I believe these automated technologies are absolutely going to be the mainstay in what we do in orthopedics. And I’m hoping it’s sooner than later.”
References
- B. Shah. (Feb. 2023). Joint Replacement Surgery. American College of Rheumatology. Accessed: Oct. 16, 2023. [Online]. Available: https://rheumatology.org/patients/joint-replacement-surgery
- I. Shichman et al., “Projections and epidemiology of primary hip and knee arthroplasty in Medicare patients to 2040–2060,” JB JS Open Access, vol. 8, no. 1, Jan./Mar, 2023, Art. no. e22.00112, doi: 10.2106/JBJS.OA.22.00112.
- V. Hedge et al., “Highlights of the 2022 American joint replacement registry annual report,” Arthroplasty Today, vol. 21, Jun 2023, Art. no. 101137, doi: 10.1016/j.artd.2023.101137.
- Yale Medicine, Fact Sheet. Avascular Necrosis & Osteonecrosis Program. Accessed: Nov. 15, 2023. [Online]. Available: https://www.yalemedicine.org/departments/avascular-necrosis-and-osteonecrosis-program