As the number of coronavirus 2019 disease (COVID–19) cases in the United States began mounting in the early weeks of March, healthcare workers raised the alarm about a looming shortage of ventilators to treat patients. On March 30, Ford Motor Company announced plans to produce 50,000 ventilators in 100 days (1), and General Motors followed suit on April 8 stating that it would deliver out 6,000 ventilators by the end of May and another 24,000 by August (2).
By the time these big-corporation announcements were made, innovative companies and research groups across the country were already well on their way toward developing effective, low-cost, and quick-turnaround breathing machines that could potentially begin saving lives even sooner. IEEE Pulse features three of those groups here: a healthcare team that is repurposing a bilevel positive airway pressure, or BiPAP, machine from a device used for sleep-apnea to one that can help COVID-19 patients; a university/hospital group that is using 3D printing, or additive manufacturing, to construct an emergency ventilator; and a medical-technology company that put its other projects on hold to construct a portable ventilator nearly from scratch.
BiPAP Conversion
For the project to convert a non-invasive BiPAP machine into an invasive ventilator (Figure 1), just 48 hours transpired from the initial idea through the working prototype, according to Hugh Cassiere, M.D., medical director for Respiratory Therapy Services at North Shore University Hospital, which is part of Northwell Health of New York, NY. The notion originally came to him in the wee hours of the morning when he was thinking about all of the underused V60 BiPAP machines at hospitals. “It kind of hit me that these machines are just pressure-cycled ventilators,” he recalled. The V60s work by supplying pressurized air to patients through a mask, keeping patients’ airways open while they sleep.
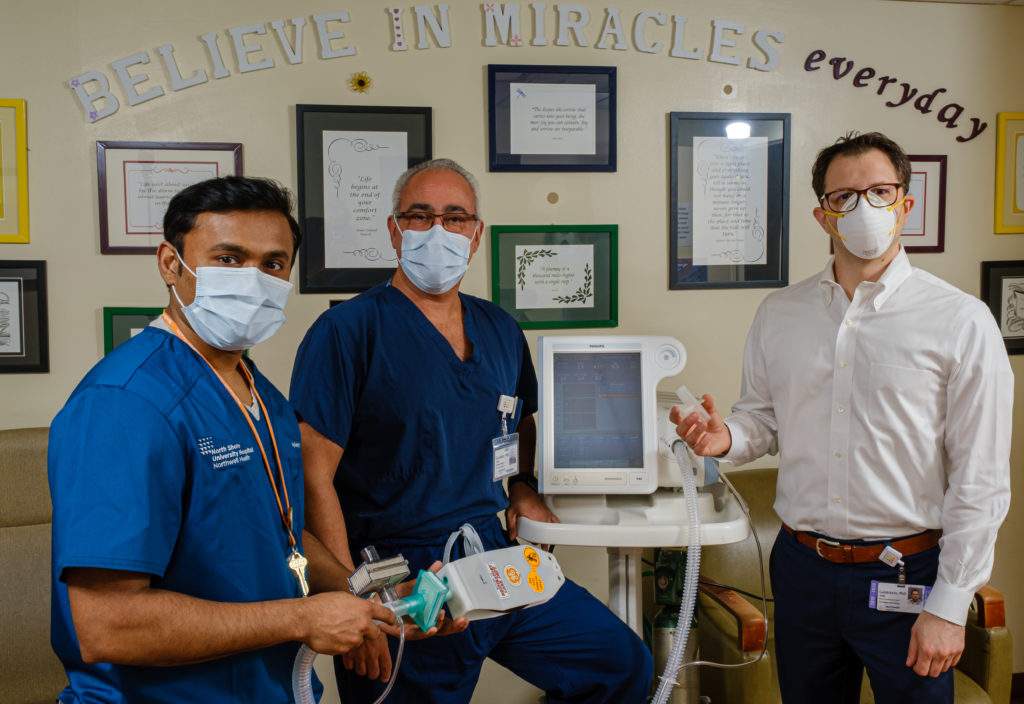
A few hours later, Cassiere met with Stanley John, director of respiratory therapy, to hash out the idea of taking a device that was approved by the U.S. Food and Drug Administration (FDA) as a noninvasive ventilator for spontaneously breathing patients and transforming it into an invasive version that can help COVID patients who are not spontaneously breathing. “When we looked at it, one thing was evident right from the beginning: it was possible,” John said. To make it work, however, they would need a part, specifically a T-adaptor, but COVID-related supply shortages made it nearly impossible to get their hands on it. So they consulted Todd Goldstein, Ph.D., director of 3D Design and Innovation at Northwell Health.
Goldstein obtained the specs for the adapter, did his own precise measurements, and printed the plastic-resin piece with one of the department’s 3D printers (Figure 2). “It was actually a very straightforward project because we knew exactly what we needed to do and we had the equipment, so we just had to make the adaptor fit perfectly,” he described.

The group then put it all together, inserting the hot-off-the-printer adaptor, incorporating two high-efficiency particulate air (HEPA) filters to the two ends of the oxygen hose to ensure a clean air supply, and reconfiguring the V60’s already-existing computer menus to work as an invasive, pressure-controlled ventilator. The team successfully ventilated patients who had respiratory failure not due to COVID-19, which Cassiere said would be a way to free up true hospital-grade ventilators for the non-COVID-19 patient population, and then it tried the modified V60 on COVID-19 patients. “We did proof of concept and we were able to ventilate a patient with very sick COVID-19 lungs for six hours with very good effect and results,” he reported.
All the information, including the 3D printing file, has been open-sourced and is available to anyone in a hospital setting who wants to do a similar conversion of BiPAP machines for COVID-19 use (3).
Additive approach
An Illinois team’s work on an emergency ventilator got started back on March 13 when bioengineer Rashid Bashir, Ph.D., dean of the Grainger College of Engineering, University of Illinois at Urbana-Champaign (UIUC), heard from local healthcare providers about the imminent need for ventilators. He immediately contacted colleague Bill King) Ph.D., UIUC professor of mechanical engineering, about how they might be able to help (Figure 3, a and b).

Within a matter of hours, Bashir and King had galvanized a team of more than three dozen others across campus and the Carle Foundation Hospital in Urbana, IL, to come up with a working prototype (Figure 4). Other partners included the machine shop Tekmill of Champaign, IL, and the engineering consulting company Creative Thermal Solutions Inc. or Urbana, IL. In less than two weeks, the team had developed RapidVent (4), a fairly simple mechanical device that attaches to the oxygen supply already present in most hospital rooms, Bashir said. To properly ventilate the patient, the RapidVent device is built with two pressure sensors: one that detects low pressure and starts delivering oxygen to the patient, and one that detects high pressure and stop the air flow when the lungs are properly inflated.
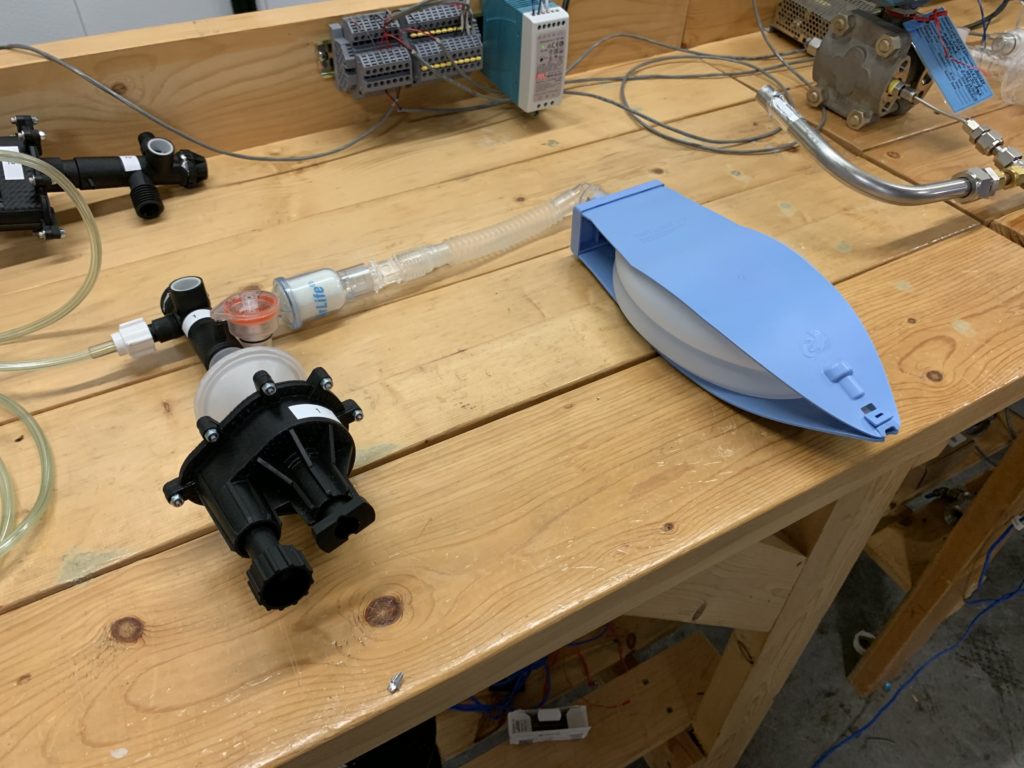
Altogether, RapidVent has 20 parts, five of which the researchers were able to buy ready-made. For the remaining 15, they turned to additive manufacturing to print exactly what they needed. “There was a lot of intricacies in the actual components to make sure they all could interface together and then be assembled together,” Bashir said. Their very first prototype functioned just as they had hoped, delivering consistent ventilation over multiple days of testing.
The group is now offering a non-exclusive open license to anyone who is interesting in producing the RapidVent. So far, about three dozen licenses have been executed, and Bashir is optimistic that some of the companies will now be able to obtain the necessary FDA approvals to produce hospital-ready machines quickly. In recent news, consumer electronics giant Belkin announced on 12 May 2020 that they are producing an emergency ventilator based on the RapidVent concept and plan to make at least 10,000 ventilators.
Ventilator From Scratch
Quadrus Medical Technologies focuses on data-collection and -analysis software for disease detection and prediction, but when the pandemic hit, founder and CEO Nicolas Chbat, Ph.D., shifted its focus to designing a basic and effective ventilator (Figure 5). The change in direction actually wasn’t much of a leap for Chbat, who had years of prior experience as principal researcher and head of the Cardiopulmonary Lab at Philips Research North America, where he spent a good portion of his time working on ventilators.

For the new ventilator project, Chbat didn’t want just a miniature version of an already existing ventilator. Rather, he wanted to start from a control-systems point of view, and to develop a machine that would put all the essential respiratory tasks into a small and efficient package. At the same time, he wanted to include protection against the lung damage that can sometimes occur due to excess air pressure or volume during artificial ventilation. “So we came up with a technology that controls the pressure, and at the same time ensures that the right amount of tidal volume goes into the lung,” he said, noting that even the large hospital ventilators today don’t always have both pressure and volume controls. In addition, he is incorporating an oxygen-concentration controller into the ventilator that allows physicians to set the percentage of oxygen in air delivered to the patient.
Chbat hopes to have two finalized prototypes to bring to the FDA in May. One has some added automation, which would allow even minimally trained individuals to operate it. Under the FDA’s Emergency Use Authorization, it can potentially turn around an approval in two weeks, so he said he plans to camp out near the FDA’s Washington D.C. office and wait for it. In the meantime, he is rushing to find a mass-manufacturing partner who can get production started just as soon as the FDA approval comes through.
While he envisions the Quadrus ventilator as a life-saving device during the COVID crisis, he also sees its longer-term use as a low-cost, efficient option for healthcare systems in rural communities and developing countries that lack a full complement of medical equipment.
Fast, but right
A key to the Quadrus ventilator and indeed all COVID projects is to hurry, but not to the detriment of the project, cautioned Chbat. “Just because we are in a ‘war situation’ and we want to develop something quick, it doesn’t mean we have to develop something kludgy. We need to do minimal right engineering.”
Likewise, Bashir commented about the importance of focus on the RapidVent and other COVID-related projects. “If you think about translational work, the partnership between engineering and medicine, and having an impact, this is it,” he said. “This has been a call to all engineering communities, and especially biomedical engineering communities, to respond to the need and what can we do now to help our healthcare workers on the front line of this pandemic.”
References
1) Ford Motor Company, “Ford to produce 50,000 ventilators in Michigan in next 100 days; partnering with GE Healthcare will help coronavirus patients,” March 30, 2020. Available online at https://media.ford.com/content/fordmedia/fna/us/en/news/2020/03/30/ford-to-produce-50-000-ventilators-in-michigan-in-next-100-days.html. Accessed 13 April, 2020.
2) Domonoske, C. “GM Will Build 30,000 Ventilators For U.S. Government,” NPR, April 8, 2020. Available online at https://www.npr.org/sections/coronavirus-live updates/2020/04/08/829657257/gm-will-build-30-000-ventilators-for-u s-government. Accessed 13 April, 2020.
3) See the file “Final Instructions_for_v60_conversion_with_photos.pdf” available at https://drive.google.com/drive/folders/1YA8wwh72UGzI1ExW3rHe0 smGiLFnX0f.
4) Illinois Grainger College of Engineering, “Illinois RapidVent: Working prototype of an emergency ventilator for COVID-19 patients. Available online at https://rapidvent.grainger.illinois.edu/. Accessed 13 April, 2020.
5) Quadrus Medical Technologies, http://quadrushealth.com/. Accessed 13 April, 2020. 6) U.S. Food and Drug Administration, “Enforcement policy for ventilators and accessories and other respiratory devices during the coronavirus disease 2019 (COVID-19) public health emergency: Guidance for industry and Food and Drug Administration staff,” March 2020. Available online at https://www.fda.gov/media/136318/download. Accessed April 13, 2020.


