Forty years ago, Les Baugh lost both of his arms in an electrical accident. With bilateral shoulder-level amputations, his options for prosthetic arms were limited. That changed two years ago, when Baugh underwent a surgical procedure at Johns Hopkins Hospital in Baltimore that allowed him to control state-of-the-art robotic arms using nerves that had been rerouted to his chest. Within ten days of training, he was able to control both arms simultaneously and move a cup from a lower shelf to a higher shelf—a task that previously had been impossible—just by thinking about how he wanted to move his arm.
This is only one example of the impressive technological advancements that have been made in the world of prosthetic devices in recent years. Researchers around the globe continue to find ways to make prostheses even better—from more closely emulating the human knee joint to controlling a robotic arm with brain signals. Equally exciting are advancements in orthotic devices that help soldiers carry heavy loads in combat, patients recover from the side effects of stroke, and seniors retain mobility as they age.
Building a Better Knee
It turns out you can learn a lot from studying the physics of rubber bands. Heike Vallery, Ph.D., did just this to develop a new type of prosthetic device designed for people who have above-the-knee amputations and want to maintain a very active lifestyle. “The current devices limit how much they can do,” says Vallery, who is an associate professor of mechanical engineering at the Delft University of Technology in The Netherlands. “We’re trying to replicate the flexibility of the human knee joint.”
The ANGELAA (for ANGle-dependent ELAstic Actuator) leg is a lightweight, motorized knee prosthesis that replicates the physiological changes in stiffness that occur in a human knee when a person takes a step (Figure 1) [1]. To develop this prototype, Vallery and her collaborators at the Swiss Federal Institute of Technology in Zurich looked at how torque and stiffness change in the human knee during the gait cycle. They then built a prosthetic knee that mirrored these measurements so the stiffness of the knee changed as a function of the joint angle. “We don’t need to have the peak torque and peak stiffness everywhere; we just have it where people also have it,” Vallery explains. By emulating the limitations of the human knee joint, they were able to downsize the prosthetic knee’s motors and make a lighter device. Right now, the prototype weighs about the same as a human leg.

So far, patients have successfully used the ANGELAA leg for walking and climbing stairs in a lab setting with a remarkably smooth gait. Theoretically, it could also be used for running and jumping, although the developers haven’t tested those applications yet.
The ANGELAA leg gets its flexibility through the use of rubber cords. Rubber has its benefits in a prosthetic device: it is light and inherently pliable. However, this pliability also makes it trickier to use in a joint because rubber is viscoelastic and will continue to expand once stretched. “If you look at our paper on the prostheses, you’ll see a large portion of it devoted to how do we measure force in a rubber band,” Vallery continues.
Vallery hopes to use more lightweight materials in future prototypes. “It’s quite functional; it works, but it’s still too heavy,” she says. Weight is an important consideration because it can be painful for patients when a prosthesis pulls on the interface with their biological leg. Lightening the device would also open it up to more people who don’t currently have access to active knee prostheses and, instead, are using fairly rudimentary devices.
According to Vallery, there are some other challenges for the future of powered knee prostheses. One is energy supply—the ANGELAA leg is currently tethered to a computer and a power supply, but some groups are working on harvesting the body’s kinetic energy to power prostheses. For example, two companies—Bionic Power, based in British Columbia, Canada, and KCF Technologies, based in State College, Pennsylvania— are developing technology that could allow the batteries of lower-limb prostheses to be recharged by walking.
Another challenge is improving the interface between the leg and the prosthesis. Vallery would also like to make the leg more “intelligent,” so it can be controlled by the existing human neuromuscular control system. She says that the ultimate goal is to “make the person really be the master of this device.”
Myoelectric Leg Prostheses
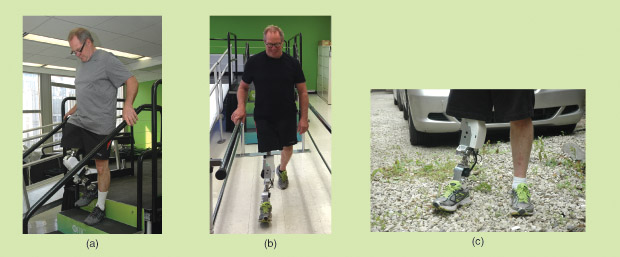
Other groups are hard at work on developing myoelectric prosthetic devices. Levi Hargrove, Ph.D., the director of the Neural Engineering for Prosthetics and Orthotics Laboratory at the Rehabilitation Institute of Chicago, and his multidisciplinary team use skin electrodes to collect electromyogram (EMG) signals that are decoded to control robotic legs (Figure 2). “They just record the natural signals that your muscles generate—even amputated muscles generate these,” explains Hargrove. “We decode them and tell the leg how to move.”
The EMG signals are integrated with signals from sensors on the prosthetic leg to create a control system that automatically changes how the leg moves based on the activity the user wants to engage in, such as standing up, climbing stairs, and walking up or down slopes. Hargrove remarks, “Rather than react to how the person is pushing on the leg, you can predict how they’re trying to move their amputated limb.”
This is a big change from existing prostheses, which require a remote or an exaggerated movement to signal a change in the activity mode of a limb. A 2015 study by Hargrove’s group found that integrating EMG signals into the control of lower-limb prostheses significantly improved the accuracy of the patient’s ambulatory mode and allowed for smoother transitions between modes [2]. “The feedback from [patients] was overwhelmingly positive.” The team receives weekly requests from people who want to buy the device or participate in a study.
The technology is at a point where a patient could expect to have an error similar to stubbing a toe about once every 1,000 steps and a more serious jolt every 10,000 steps. And the team has just started a trial in which people will test the device in their own homes. “That’s going to be very important for us to check that it’s safe, reliable, [and] useful for the patients,” Hargrove points out. Depending on the outcome of this study, Hargrove foresees a product going to market in about five years. “That’s a fairly short timeline in the prosthetics field,” he notes.
Robotic Hands
Legs aren’t the only prostheses to benefit from the integration of EMG signals. The newest generation of commercially available prosthetic hands is also controlled myoelectrically. The German prosthetic company Ottobock has developed the Michelangelo prosthetic hand, which contains a main drive that controls seven possible grip types. Its middle finger, index finger, and thumb are actively driven, and the thumb is under the control of its own drive, allowing it to be positioned independently based on EMG signals. The bebionic3 hand from the British prosthetic company Steeper has individualized motors for each finger and 14 selectable grip patterns.
These myoelectric robotic hands allow patients with belowthe- elbow amputations to use their hands for many activities of daily living, such as eating, typing, carrying objects, tying their shoes, and opening doors. There is one thing, however, that these hands cannot do: offer tactile feedback to the user about what the hands are doing.
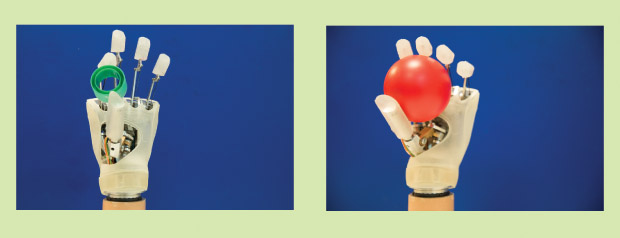
Christian Cipriani, Ph.D., an associate professor with the BioRobotics Institute at the Scuola Superiore Sant’Anna in Pisa, Italy, and his colleagues have been developing myoelectrically controlled robotic hands that provide sensory feedback to the user via discrete vibrotactile bursts on the forearm (Figure 3). “Every time you touch and release an object, you can get this small vibration,” he explains. These vibrations are relayed to the brain, where they help improve motor control. For example, when a person reaches for a cup to take a drink, he or she will feel a vibration on the forearm as his or her hand touches the cup, and this will tell the brain to automatically move on to the next stage: lifting the cup.
In a 2015 study conducted by Cipriani and other members of the BioRobotics Institute, five patients tried out a discrete event-driven sensory feedback control glove (the DESC glove) that was integrated with commercially available myoelectric prosthetic hands. Results from a one-month home trial and tests in the lab showed that the integrated sensory feedback improved the control these patients had over their prostheses [3]. “It improves the way they control the hand grasp,” notes Cipriani. “For example, to support eggs without crushing them—without even needing to watch them.”
Moreover, Cipriani continues, patients in this trial were “very happy” with the hands: “Some of them actually kept the system. I think it’s been a year already, and they’re still using it at home.”
“We are actually looking for investors or companies that can come and take this and bring it to the market,“ Cipriani comments. “It would be a very simple device. But the market is very small. This is a problem, and it’s difficult to put in new products.”
Targeted Muscle Reinnervation
For people like Les Baugh who have amputations above the elbow or at the shoulder, a more invasive technique called targeted muscle reinnervation has the potential to be a real game changer—especially because most shoulder-level amputees don’t currently use any prosthetic devices.
“I’ve literally seen people burst into tears,” says Michael McLoughlin, M.S., the chief engineer for the Johns Hopkins Applied Physics Laboratory (APL). “After ten years of an amputation or even longer, all of a sudden they’re moving an arm again. It’s a really powerful experience for the patient.”
In targeted muscle reinnervation, the nerves that previously controlled arm, wrist, and hand movements are surgically moved to other muscles, such as those on the chest. Surface electrodes collect EMG signals from these muscles, and pattern-recognition algorithms translate these signals so they can be used to control the movement of robotic prosthetic arms. “We essentially rewire the nerves so that if you think, ‘flex my wrist,’ we can measure that from a muscle surrogate,” McLoughlin explains.

The robotic arms developed by the APL, which receives funding from the Defense Advanced Research Projects Agency (DARPA), are engineering feats in their own right (Figure 4). They have 26 joints that are controlled by 17 different motors. Each arm weighs about nine pounds—similar to an average man’s arm. The fingers can be moved individually, and the hand can form very complex hand grasps. “It’s strong, lightweight, and looks and moves like a human arm,” says McLoughlin.
The arms also contain almost 200 sensors, including pressure sensors on the fingertips and torque sensors on the wrist. Information from these sensors can then be used to provide sensory feedback to the reinnervated nerves, although it takes six months or more for the nerves to grow enough to receive this feedback. For one patient, this feedback worked so well that he was able to discriminate between hard and soft objects while his eyes were shielded.
McLoughlin says close to 20 people have tested their prototypes at the APL over the past several years. This includes people with amputated limbs as well as people with spinal cord injuries. For the latter group, electrodes implanted into the brain collect neural signals about the patient’s intention to move his or her arm, which are then used to control the robotic arm [4].
Despite these advancements, the arms developed by the APL are still in the prototype stage, and patients aren’t yet able to use them at home. As McLoughlin notes, “The wife of one of the people we worked with said to me, ‘You know if you can’t give him an arm to take home, you’re just going to have to keep him.’ ”
McLoughlin says there’s not yet a large enough market to make the arms commercially viable, “but certainly the technology is ready to go.” So finding a way to get the arms to the people who need them is now his priority. “I see all kinds of applications for this, but we’ve got to get it out of the laboratory. That’s the thing we’re really focusing on now.”
One way to expand the possible uses of this technology— and therefore its market—is to apply it to orthotic devices. Think of something like an exoskeleton that can support the arm of, say, someone who’s had a stroke. In fact, orthotic exoskeletons are already under development.
[accordion title=”And Something Else New in Assistive Technology – BMW’s Racing Wheelchair”]
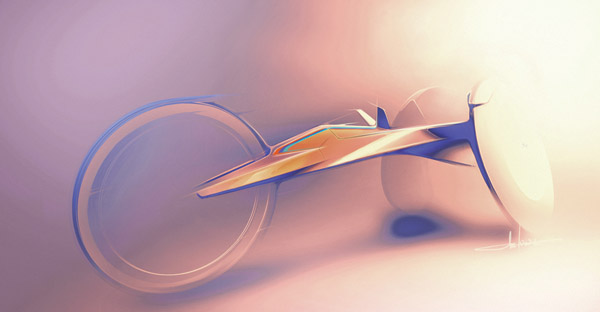
Some athletes on the U.S. Paralympics Team have an extra reason to be excited about this year’s games in Rio de Janeiro, Brazil. That’s because BMW is in the process of designing a new state-of-the-art carbon-fiber racing wheelchair for the team. The chair is specifically designed for track and field race events, including sprints and marathons.
“The wheelchair project is a unique opportunity for BMW to apply the design and performance technology used in our vehicles to help these amazing athletes achieve their goals,” says Brad Cracchiola, an associate director of project management at Designworks, a BMW Group company. “Our goal is to develop the highest performance racing wheelchair for the U.S. Paralympic track and field team.”
According to Cracchiola, the racing wheelchairs currently used by athletes are based largely on “old bicycle technology, but far from the level of current racing bicycles.” The standard design includes a welded aluminum frame, exposed steering mechanics, and a “somewhat boxy cockpit area.”
BMW’s new prototype takes advantage of higher performance materials, such as carbon fiber (pictured above). The developers applied an iterative design process that uses computer simulations to test ways to reduce aerodynamic drag and to analyze the structural stiffness and integrity of possible designs. “This approach helps us design a racing wheelchair that is lighter weight, more aerodynamic, with a stiffer chassis, and ultimately more efficient,” notes Cracchiola.
The design team at BMW is also working on making the fit of the wheelchair customizable. “Paralympic athletes each have unique bodies and require different kinds of support and restraint,” Cracchiola adds. “Improving and customizing the athlete–wheelchair interface will help create a seamless transfer of an athlete’s power into speed.”
Completely redesigning a wheelchair like this is no easy feat. “This is a unique challenge and not a trivial one,” according to Cracchiola. “It’s a tricky balance because improving one aspect of the wheelchair design can lead to potential compromises in another area.”
The designers created a rough proof-of-concept prototype to evaluate the carbon chassis design and the ergonomics of the wheelchair. Smaller proof-of-concept prototypes have been used to evaluate the braking and steering systems, wheel design, and athlete-customization methods. The developers are now in the process of building a second complete prototype that will be used for more rigorous performance testing.
“Testing with athletes will begin in the near future,” says Cracchiola. “So far, the athletes and coaches have been very excited about the design and the performance innovations we are exploring.” And, they hope, the new design will help bring them success in Rio.
[/accordion]
Wearable Robots
Conor Walsh of the Wyss Institute at Harvard University is working on a DARPA-funded project to develop an exosuit (Figure 5) [5]. “It’s a soft wearable robot that uses textiles to interface with the human body,” he says. “We use motors and cables to apply forces to those textiles that provide assistance to joints of the leg of the human body.”

Although the device is still in the early development stages, the team has already tested it on several soldiers and continues to conduct testing. The exosuit could help military personnel carry heavy loads in the field or otherwise more easily complete difficult tasks. And the technology is on its way. “There’s still a lot of technology development that has to be done to make these a reality, but we’ve seen definitely very exciting kinds of proof-of-concept results,” Walsh adds.
The group is also testing the device on patients who have suffered strokes and have difficulty walking. “We can help them walk with less energy, and we can make their gait more symmetric,” Walsh explains.
People who wear the suit gradually adapt to it so it doesn’t feel significant—until the suit is turned off. According to Walsh, “It doesn’t change the way you walk, it’s very flexible and nonrestrictive, it’s very lightweight, and then as soon as you turn the assistance off, all of the sudden, at the end, people feel like their legs are very heavy.“
There were a number of challenges in developing the exosuit, but the largest was making the suit soft and flexible. “How do you apply assistance to the legs without the use of a rigid device?” Walsh asks. “Definitely the textile and apparel component has been one of our big innovations.”
“I think probably the most interesting scientific challenge going forward is how do you make sure the suit is always doing the right thing for every different type of person,” Walsh comments. “We all walk a little bit differently.” He imagines that there will be different versions of the suit for different people, depending on whether someone needs more help with his or her hip, knee, or ankle.
Walsh projects it will realistically be at least five years before soldiers in the field will be wearing exosuits. But for clinical applications, the time frame may be faster, perhaps as fast as three years from now.
Although challenges remain in terms of making the next generation of prosthetic and orthotic devices commercially ready, these innovations and the dozens of other devices under development by other groups are changing the way users view these devices. “We’re moving from a perspective where the patient says, ‘Hey, this is a prosthetic arm, it’s some tool that I use,’ to, ‘This is actually an extension of my body, myself,’” McLoughlin concludes. “That, I think, is really exciting.”
References
- S. Pfeifer, A. Pagel, R. Riener, and H. Vallery, “Actuator with angle-dependent elasticity for biomimetic transfemoral prostheses,” IEEE/ASME Trans. Mechatron, vol. 20, no. 3, pp. 1384–1394, June 2015.
- L. J. Hargrove, A. J. Young, A. M. Simon, N. P. Fey, R. D. Lipschutz, S. B. Finucane, E. G. Halsne, K. A. Ingraham, and T. A. Kuiken “Intuitive control of a powered prosthetic leg during ambulation: A randomized clinical trial,” JAMA, vol. 313, no. 22, pp. 2244– 2252, 2015.
- F. Clemente, M. D’Alonzo, M. Controzzi, B. Edin, and C. Cipriani, “Non-invasive, temporally discrete feedback of object contact and release improves grasp control of closed-loop myoelectric transradial prostheses,” IEEE Trans. Neural Syst. Rehab. Eng., 2015. doi: doi.org/10.1109/TNSRE. 2015.2500586
- K. D. Katyal, M. S. Johannes, S. Kellis, T. Aflalo, C. Klaes, T. G. McGee, M. P. Para, Y. Shi, B. Lee, K. Pejsa, C. Liu, B. A. Wester, F. Tenore, J. D. Beaty, A. D. Ravitz, R. A. Andersen, M., and P. McLoughlin, “A collaborative BCI approach to autonomous control of a prosthetic limb system,” in Proc. 2014 IEEE Int. Conf. Systems, Man, and Cybernetics, San Diego, CA, 2014, pp. 1479–1482.
- A. T. Asbeck, K. Schmidt, and C. J. Walsh, “Soft exosuit for hip assistance,” Robot. Auton. Syst., vol. 73, pp. 102–110, Nov. 2015.



