In rural areas, it is not unusual for patients to travel 50 miles or more to reach their doctors’ offices or for doctors to refer patients to specialists whose offices are 80, 100, even 200-plus miles away. The sheer distance is a major obstacle for patients of all kinds: those who need urgent specialist care, those who have a chronic condition that requires regular visits, those who live in areas prone to poor weather-related driving conditions—really, anyone who has better things to do than spend hours traveling to and from a medical appointment.
“Most of the clinicians, specialists, and subspecialists are regionalized, and that makes sense in terms of efficiency and quality, but that creates access barriers for people who live in rural areas. There have been lots of studies and lots of data showing that [people from rural areas] are relative underutilizers of preventive care, specialty care, and subspecialty care because of those access barriers,” says James Marcin, M.D., director of the University of California Davis (UC Davis) Children’s Hospital Pediatric Telemedicine Program (Figure 1).

Although challenging in other aspects, this geographical expanse between rural residents and doctor’s offices presents an opportunity for mHealth, or health care supported by mobile-device and wireless technologies. The advent of advanced communications capabilities and equipment, including increasingly powerful and versatile smartphones, tablets, and other devices, is enriching the care that rural providers can offer, bringing rural patients the type of team care previously associated only with big-city medical centers and bettering community health in general.
Doctor to Doctor
One way mHealth is closing the distance between patients and health care is through the use of wireless technologies that connect rural providers to specialists at urban medical centers, a strategy that not only bridges the physical separation between them but also improves the speed, coordination, and quality of care, Marcin says. Often, it also decreases overall health care costs because patients receive the care they need more promptly, when, for many conditions, treatment is easier and less expensive to provide.
Marcin, who works in a pediatric intensive-care unit (ICU), uses outpatient pediatric neurology as an example. “There are kids who have seizure disorders, neurologic issues, or cerebral palsy and need their medications and symptoms addressed but who live more than an hour away from the closest regional medical center,” he says. This often means that parents have to miss at least a half-day of work due to travel time. No-show rates also increase with the distance the patient has to travel, he adds. “So with mHealth and telehealth technologies, what I do as a pediatric ICU doctor is hook up to rural emergency departments so I can provide some pediatric expertise virtually, which allows the rural clinicians to manage emergent care and keep it local.” This type of live, interactive videoconferencing is known as synchronous telemedicine.
In asynchronous telemedicine (sometimes called store-andforward telemedicine), a rural doctor might transmit an image of a rash or a lesion to a dermatologist or a diabetic-retinopathy screening image to an ophthalmologist, who then reviews it later as time permits. “UC Davis got involved in telehealth very early, probably more than 20 years ago, and we’ve used it in innovative ways, including store-and-forward telepsychiatry,” Marcin says. In asynchronous telepsychiatry, a medical assistant or nurse goes through a structured interview with a patient, records it, and transmits it to a psychiatrist who later reviews it quickly to help with the diagnosis and/or to adjust the medications. “This method is often as accurate as an in-person session, but it’s more efficient,” he asserts.
A third mHealth model that combines synchronous and asynchronous telehealth is UC Davis’s Pediatric Emergency Assistance to Newborns Using Telehealth (PEANUT) program. The program provides rural communities with access to subspecialties within pediatrics, such as neonatalology, cardiology, and neurology, according to Madan Dharmar, M.B.B.S., Ph.D., the principal investigator for the PEANUT program and associate professor in residence in the UC Davis Pediatric Telemedicine Program. “Our neonatologists are the primary contacts for the rural doctors, and based on the needs of the newborn, the neonatologists can bring in other specialists, again over telemedicine. So through that one portal, a newborn who is born in a rural nursery now has access to all these specialists who may be hundreds of miles away.” Protocols also ensure that specialists respond just as promptly to rural doctors using telemedicine as they would to clinicians in their own facilities. “The newborns get the same level of care 150 miles away as they would get if they were right there at the tertiary care center,” Dharmar notes.
“The physicians and health care providers in these rural communities are providing excellent care to these newborns,“ he continues, “but when a newborn needs a higher level of care, the PEANUT program is a tool in their tool kit to augment the care they are able to provide in their community.” The PEANUT program began in late 2014 with a goal of pairing with four rural hospitals but currently has a network of eight participating, Dharmar says. “There is definitely a need and interest for this program, and that has led us to be able to expand the program to more facilities and to help more newborns.”
Patient to Doctor

Patient access even to their rural doctors and local health care facilities is a big issue, too, one that is being addressed by nurse practitioner Jennifer Mallow, Ph.D., assistant professor of nursing at West Virginia University and Robert Wood Johnson Foundation Nurse Faculty Scholar. Her answer is a web-based system that greatly reduces the number of office visits that patients need to make. After attending a conference on mobile technologies, she tapped her husband, who happens to be a web designer and database administrator, to help her design a system (Figure 2) that would benefit the patients at a free rural clinic where she volunteers as part of her university service.
Called mI SMART (for mobile improvement of self-management ability through rural technology), the system employs data collected from sensors and mobile devices that patients with multiple chronic conditions—such as hypertension, diabetes, obesity, and depression—use to monitor themselves at home, transmits the information so that it can be easily incorporated into the electronic health record for that patient, and provides feedback to the patients in real time [1]. Patients who need to meet with a health care professional can often do so virtually via videoconferencing rather than traveling to the clinic. Mallow tested the mI SMART system in 2015 with very good results, and she now hopes to commercialize it.
To design the system, she followed a process for developing complex interventions that includes problem identification, practice analysis, identification of the overall objective, identification of theory or key principles, building and planning, modeling, and seeking an expert review. Brian Mallow created the necessary security protocols, worked out some Internet connectivity issues, and spent considerable time on the design so it was easy to use for everyone, including those with no prior computer experience. That meant using big icons, keeping it simple by going no more than three pages deep, and having a home button on every page so people would never get lost in the system (Figures 3 and 4). He remarks, “We made it so it was as quick as possible to get where you need to be.”


With a working prototype in hand, Mallow and her research group had to approach only 31 clinic patients to find the 30 they needed for the trial of mI SMART. After a little adjusting, as they conferred with both doctors and patients about what information to collect and how often, Mallow started the trial. Each patient received the Bluetooth-enabled mHealth devices they needed to measure such things as blood-sugar levels, weight, and blood pressure. The collected data went to the patient’s tablet.
“mI SMART gives patients an automated, color-coded response based on their own readings and what is normal for them,” Mallow describes. “As an example, green for blood-sugar means you’re doing great, and yellow means it’s a little high or low. If it’s red, you get an automated message saying your level is critically high or critically low, and here’s what you need to do now.” On the provider side, patient information is transmitted from the tablet to the clinic’s triage nurse, who monitors the data including those alerts that predicate a response for each particular patient. “The triage nurse might contact the patient or might contact the nurse practitioner, who may then need to change a prescription or do some other intervention,” she says.
Besides the automated and provider-side monitoring, the system allows patients to
- view their own progress
- receive reminders to take their medications or blood-sugar measurements
- learn about their medications, side effects, what improvements they can expect and when they will see the improvements, drug interactions, and what they should do if they miss a dose
- view upcoming virtual and in-office clinician appointments
- watch a series of relevant patient-education videos
- submit questions via secure messaging to the triage nurse, who forwards them to the person who can respond.
The 30-person pilot showed that the patients, even those without any computer experience, could use all aspects of the system and were happy with it. “Health care providers loved it too, and the clinic is working with me now to get more funding so we can expand it and offer it to more patients,” Mallow says. In evaluating efficacy, the team found that blood pressure and blood-sugar levels were statistically improved over the trial period. “The weight means also dropped by ten pounds over 12 weeks,” she adds.
The next step is to conduct a larger, randomized and controlled trial to determine whether the acceptability, feasibility, and efficacy hold true with a bigger population. Mallow and her husband are currently investigating commercialization of this system for patients with multiple chronic conditions, and she would like to see it adapted for other patient populations in the future.
Patient to Patient
Community health doesn’t always involve health care practitioners. Among older residents who live in a rural setting, sometimes it just means senior citizens helping one another. That was the concept behind a set of prototypes developed by Katherine Connelly, Ph.D., an associate professor in the School of Informatics and Computing at Indiana University, and Kelly Caine, Ph.D., an assistant professor at Clemson University, through a project they call Supporting Older Low-Socioeconomic Status (low-SES) Adults and their Caregivers Electronically (SOLACE) [2].
“When we started this, there had been a lot of research on aging already in place, but it often sampled upper-middle-class, older adults who were somewhat tech savvy and certainly had a good education. We wanted to take what we had learned from that population and see how well it translated to low-income, older adults,” Connelly explains.
The researchers sampled 50 lower-income, older adults—half from urban areas and half from rural areas—to see how they compared to higher-income seniors. A major difference was that the higher-income group tended to have one or more relatives or close friends who acted as informal caregivers, and they wanted technologies to connect them to those informal caregivers. The lower-income seniors, on the other hand, typically either had family members who had moved a long distance away or had nearby family members who were struggling financially, frequently with multiple jobs and little time to take on caregiver duties, Connelly says. Even if family members were willing, the older adults didn’t want to be a burden on their children or other relatives, whom they knew were facing challenges of their own. What the lower-income group did have, however, was a strong community-support network of older adults, and that’s what Connelly’s group homed in on.
One of their prototypes is what they call a “check-in tree” [3], which is set up for a group of eight adults. “We had a local craftsman construct eight actual, physical trees that can sit on a counter, and from the branches of each tree hang eight framed pictures with LED lights on them, one for each of the eight people in the group,” she describes (Figure 5). All the people in the group get an identical tree. During the night, the lights around the frames begin softly flashing, and in the morning when a group member wakes up, that person touches a button on his or her tree to turn the light shining on the appropriate photo from flashing to solid. The lights simultaneously go solid on that frame on the other seven trees, which lets everyone in the group know who is up and about, and who isn’t. A still-flashing frame would then prompt the others to follow up and make sure that person was okay, she says.

The team deployed a research prototype of the check-in tree in the homes of 16 low-SES adults for eight weeks. “It was a short time and a small sample, but we were able to get qualitative-type results showing that people liked the tree and used it a lot,” Connelly explains. “In many ways, the tree was more critical for rural people, who are often far from their neighbors, so they don’t see them on the porch or on the street, as urban people might with their neighbors.” That’s especially a problem when rural people have mobility limitations that can isolate them even more, she adds. Connelly’s research team also evaluated privacy options for the check-in tree, which give a user the choice to connect a tablet computer and control his or her own picture frame. This included what the researchers called “me time,” which made it look like a user was checking in every day if they were away from home.
A second prototype, which they call the “community window,” acts as a virtual front porch, according to Connelly. It uses a computer screen to display minute-by-minute snapshots of a frequently used place in each of the group members’ homes, such as a favorite living room chair. “The group could see who’s there, click on that snapshot, and open up a Skype session to have a conversation. Alternatively, if you didn’t want people to bug you, you could ‘close your curtain’ so people couldn’t see in your ‘window,’” she explains. “The point there is to promote socialization, especially when you’re starting to feel isolated due to mobility issues.” Such isolation can lead to depression and worsening health conditions, so it has potentially wide-ranging benefits for community health.
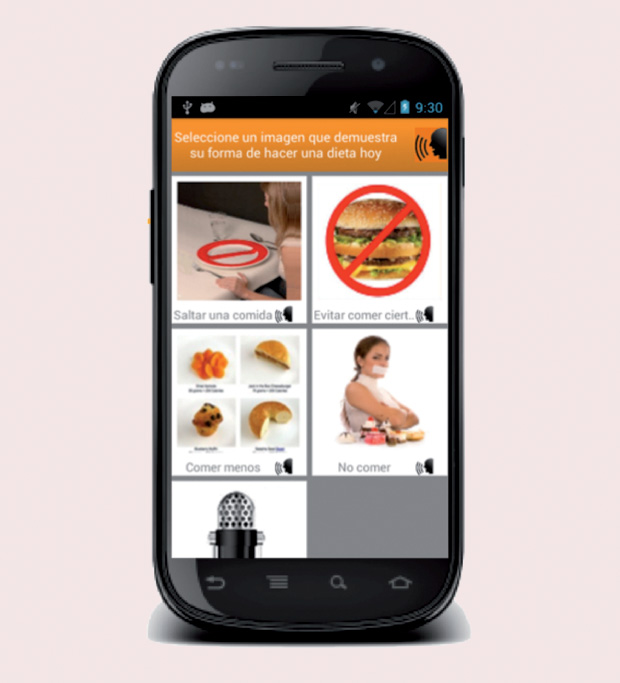
In yet another area of study, Connelly collaborated with Karen Stein, Ph.D., of the University of Rochester to develop a mainly icon-based app designed to understand eating disorders among low-income Mexican immigrant women in the United States (Figures 6 and 7). “This was supposed to be a pilot study in preparation for an R01 clinical trial [the National Institutes of Health defines an R01 trial as one that does not pose significant risk], but in the two-week field trial with 60 women, the data was so overwhelming on how many unhealthy behaviors the women were engaging in that we are [bypassing the clinical trial to demonstrate the prevalence of these behaviors, and] going straight to work on an intervention,” Connelly says. They anticipate that community ties will play an important role in helping the women counter unhealthy behaviors, such as purging or using laxatives to lose weight, but Stein and Connelly are just beginning on that project [4].

Trends and Troubles
All these programs and projects showcase the advantages of mHealth for people living in rural settings but also some of the obstacles that remain. One obstacle is iffy cell phone and Wi-Fi coverage. “We had to spend a lot of time driving out into rural New York and mapping the strength of the signals from the cell phone companies just so we knew which cell phone to give different women,” Connelly says. “This is something that technologists aren’t expecting because we live in very hightech areas, so it’s shocking to see how difficult it is to run a study just because of the lack of infrastructure.”
Wi-Fi access is also spotty, Mallow says. “We really need reliable access to the Internet. I did have some patients in the mI SMART program who said they needed to go on the front porch and lean over the railing to get a steady Internet connection, so that’s a big hurdle.”
Another hindrance to mHealth is insurance and how to pay for virtual office visits or other wirelessly provided care. “On the national level, Medicare does pay for some telemedicine, but, generally speaking, it’s quite restrictive. On the state side with Medicaid, it’s left up to the states as to whether they reimburse telemedicine and by how much,” says Marcin. Presently, he notes, about half of the states have parity laws that allow equal reimbursement for in-person and virtual office visits; fortunately, that number is rising.
The next step is to switch the focus of reimbursement from one that pays providers for services to help sick patients get well to one that pays providers to help well patients stay well. Marcin comments, “Currently, a hospital that invests a lot in technology and in efforts to keep people out of the hospital could end up with reduced revenues. With the Affordable Care Act and similar efforts, the pendulum is starting to swing from that kind of volume-based medicine to value-based medicine designed to keep patients healthy, but it’s got a long way to go.”
As reimbursement issues and Wi-Fi/cell phone accessibility lumber forward, technologies for rural populations are growing in number, and so is the promise to make lives better for all patients regardless of where they live, asserts Elizabeth Mynatt, executive director of the Institute for People and Technology at the Georgia Institute of Technology. She is designing apps for people who have either diabetes or breast cancer (see “What You Need, When You Need It”).
[accordion title=”What You Need, When You Need It”]
Diabetes and Breast Cancer Apps Help Navigate Disease

In designing apps for people who have diabetes or breast cancer, the patient should be the centerpiece, according to Elizabeth Mynatt, Ph.D., executive director of the Institute for People and Technology and professor in the College of Computing at the Georgia Institute of Technology (Figure S1). “Our approach to mHealth is focused on those consumer needs where health care is supporting them, as opposed to a lot of mHealth technologies that are centered on what the clinician wants from the patient.”
With that in mind, Mynatt and her research group developed a diabetes-management app that puts the patient in charge [1]. “We did that because, in working with diabetes education specialists, we learned that people with diabetes needed to be a detective to be successful; they had to learn how diabetes worked in their bodies,” she says. One way to do that is to give patients the opportunity to ask their own questions, via the app, about matters pertaining specifically to them and get a response from a diabetes coach. Both patients and coaches liked it. Patients appreciated the personalized assistance, and coaches were pleased to find that they could make a big difference in patients’ lives with only a few minutes a day of time investment, Mynatt reports. “One coach said it changed her job, because previously she felt like she was answering generic questions, but now she is actually getting to the heart of the matter and working with patients as individuals.”
Mynatt’s group, in partnership with a team from Columbia University, is currently finishing up a randomized clinical trial of the system. They are also building a web platform that will automate some of the personalized assistance to make the app more responsive and efficient. One of the lessons they learned while building the diabetes-management app was that patients often feel overwhelmed by everything they’ll have to do to keep their sugar in check and remain as healthy as possible. “Instead of asking the patient to try to solve everything at once, we need apps that peel off one level at a time so the patient can tackle a smaller skill first. Once the patient gains mastery and confidence, then they can move onto the next level,” Mynatt explains. “If you look at the weight-control apps that are out there now, they’re very good at showing you that in a week’s time, you haven’t made much progress in reaching your goal, but they’re not very good at coaching or helping people to break it into smaller steps to tackle, master, and stay motivated.”
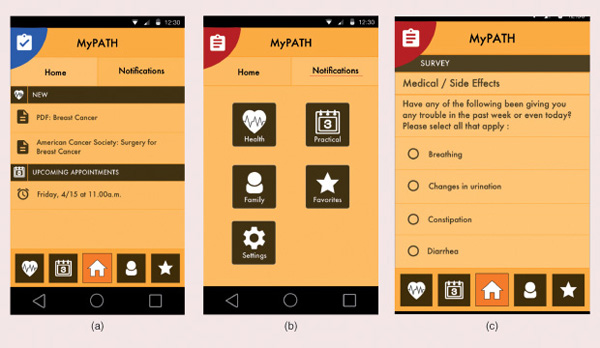
That led Mynatt’s group to build an app for newly diagnosed breast-cancer patients [2] that takes them one step at a time through the treatment journey, she says (Figures S2 and S3). “So what we’re doing is downloading all the mass of information about breast cancer into a tablet, along with the patient’s treatment schedules and data about specific medical issues or other hurdles, such as money, transportation, or childcare issues.” From that, the app shows the patient what’s coming up next and helps her prepare. “For instance, if you have a surgery coming up, the app might give you a virtual tour of the surgery center so it’s not totally foreign when you arrive. Or if you’re going to have radiation, it might tell you that radiation burns can be painful, so you won’t want to wear a bra for a few days and might want to coordinate with a friend to visit you at home afterward.” The tablet app also allows patients to ask questions and report concerns every day. “For instance, a patient might want to note a side effect, or say that she’s worried about finding a driver if she can’t drive following a procedure,” Mynatt says. That information goes to the patient’s “care navigator,” who can then follow up.
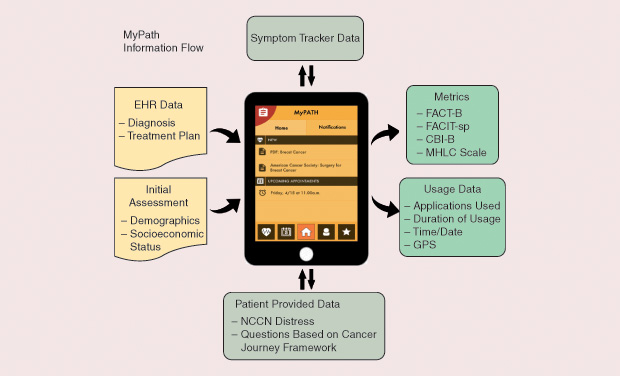
A pilot study of the breast-cancer tablet and app will run through late 2016, and a controlled trial funded by the National Institutes of Health will begin in January 2017. Eventually, Mynatt would like to see the tablet app commercialized, especially because chemotherapy is moving toward prescribed oral medicine that patients can take themselves at home. “That means patients will no longer have to come into the chemo center, so they won’t have the support of the staff around them, and they won’t have the interaction with other patients, [interactions that] can be very comforting.” She adds, “If chemo goes this route, and a patient is sitting alone in her house and staring at this bottle of pills that make her feel really lousy, then it’s going to be even harder to keep that patient engaged and staying on top of her treatment.”
Mynatt believes the app is one way to coach those patients through the cancer journey and toward health. She remarks, “As cancer treatment evolves, apps like this will be even more important.”
References
- L. Mamykina, E. Mynatt, P. Davidson, and D. Greenblatt, “MAHI: Investigation of social scaffolding for reflective thinking in diabetes management,” in Proc. Special Interest Group on Computer–Human Interaction (SIGCHI) Conf. Human Factors Computing Systems (CHI ‘08), 2008, pp. 477–486. [Online].
- M. Jacobs, J. Clawson, and E. D. Mynatt, “Lessons learned from a yearlong deployment of customizable breast cancer tablet computers,” in Proc. Conf. Wireless Health (WH ‘15), New York, 2015, pp. 1–7.
[/accordion]
“mHealth technology for rural care essentially becomes flexible care for the rest of us,” Mynatt says. For instance, pediatric mobile health is ideal for rural patients, but it’s also a boon, for example, to every parent who has a child prone to ear infections. “These parents want to be able to take a picture of a child’s ear, send it in to a clinician who can verify it’s an ear infection, and just get the meds dialed in to the pharmacy,” she says. “Being able to do that type of diagnosis and support through telemedicine not only overcomes barriers that are socioeconomic or that have to do with physical distance in the case of rural patients, but also results in more convenient health care for all of us.”
References
- J. A. Mallow, L. A. Theeke, D. M. Long, T. Whetsel, E. Theeke, and B. Mallow, “Study protocol: Mobile improvement of selfmanagement ability through rural technology (mI SMART),” Springerplus, vol. 4, p. 423, Aug. 2015.
- G. White, T. Singh, K. Caine, and K. Connelly, “Limited but satisfied: Low SES older adults experiences of aging in place,” in Proc. Ninth Int. Conf. Pervasive Computing Technologies Healthcare (PervasiveHealth), Istanbul, Turkey, 2015, pp. 121–128.
- I. Arreola, Z. Morris, M. Francisco, K. Connelly, K. Caine, and G. White, “From checking on to checking in: Designing for low socio-economic status older adults,” in Proc. Special Interest Group on Computer–Human Interaction (SIGCHI) Conf. Human Factors Computing Systems (CHI ‘14), New York, 2014, pp. 1933–1936.
- K. Connelly, K. F. Stein, B. Chaudhry, and N. Trabold, “Development of an ecological momentary assessment mobile app for a low-literacy, Mexican American population to collect disordered eating behaviors,” J. Medical Internet Res. Public Health Surveill., vol. 2, no. 2, p. e31, July–Dec. 2016.



