Food allergies and sensitivities have always been a public health problem but are becoming more prevalent worldwide. The U.S. Food and Drug Administration (FDA) reports that millions of Americans have allergic reactions to food each year. More than 17 million Europeans have a food allergy, and hospital admissions for severe reactions in children have risen sevenfold over the past decade, according to the European Academy of Allergy and Clinical Immunology.
Peanut allergies, in particular, have increased and are a leading cause of food-allergy-related deaths in the United States (about 200 every year). Approximately 3 million Americans are allergic to nuts, one of the most common food allergens with the potential to cause severe, potentially fatal, allergic reactions. Meanwhile, more and more Americans are reporting sensitivity to the wheat product gluten, prompting countless restaurants and food manufacturers to offer gluten-free items.
With no cure available, people suffering from food allergies cope by strict avoidance of major allergens such as milk, eggs, fish, shellfish, nuts, wheat, and soybeans. That’s because even just a tiny taste of an offending food can cause severe symptoms in some people, potentially leading to anaphylaxis and death. Aside from allergies, many others suffer from food sensitivities and intolerances that may not necessarily cause a severe reaction but can negatively impact quality of life. Although consumer protection laws require labeling of packaged foods, eating out can still be a gamble, as misinformation and cross contamination are frequent.
The technology to break down food and other materials to see what lies inside (via light techniques or chemical reactions, for example) has been available for a long time—but for science labs, not for consumers. While a number of devices are emerging to help people find out what’s in their food and steer clear of certain ingredients, affordable, portable, and practical products that can detect life-threatening allergens—like peanuts—on a sensitiveenough scale to be useful are still a way off, but perhaps not more than a few years.
Avoiding Allergens
Just as with everything else, there are a plethora of apps available to help consumers learn what’s in a food they may potentially buy. One of the more popular ones, ipiit, scans labels at grocery stores to quickly warn users of problematic ingredients.
The ipiit app (Figure 1) will alert users if packaged food products do or do not meet their guidelines (for example, organic products only). The app, launched in 2013 by San Francisco-based cofounders Rosalie Schill and Betty Toth, has several hundred thousand downloads to date. Right now, the app will search for 16 ingredients or preferences, saving users the need to read all the fine print on every product they are considering buying. It can also suggest alternative products according to preferences, favorites, and ratings.
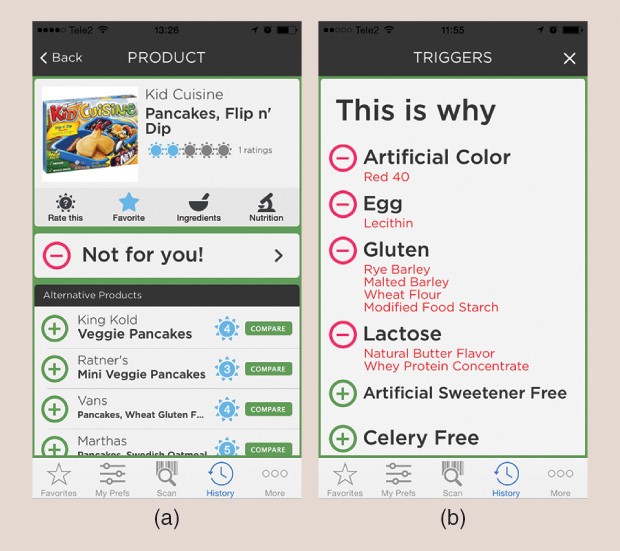
“The app isn’t just for those who are food sensitive or allergic,” says Schill. “Neurologists have recommended the app to patients to help them exclude potentially migraine-triggering ingredients, like artificial sweeteners.” The team is not targeting peanuts and severe nut allergies right now, as packaged food can contain trace amounts of peanuts, for example, that don’t necessarily make it into the product database the app is tapping into.
Among users to date, gluten is by far the most commonly excluded ingredient, according to Schill. The team has about 100 requests for items people want to exclude due to allergies or medical issues, including beeswax, cabbage, caffeine, and other chemicals. Schill has noticed an interesting trend in data among users: women have tended to exclude corn syrup, and men have tended to exclude artificial sweeteners and dyes.
Apps, however, can only go so far. New in this area are handheld products promising to deliver information on foods outside the grocery store.
“One of the major challenges is that a consumer technology has to be extremely simple and rapid to use without the need for any expensive or bulky instrumentation or lengthy sample preparation steps,” says Aydogan Ozcan, Ph.D., a professor of electrical engineering and bioengineering with the University of California, Los Angeles, and associate director of the California NanoSystems Institute.
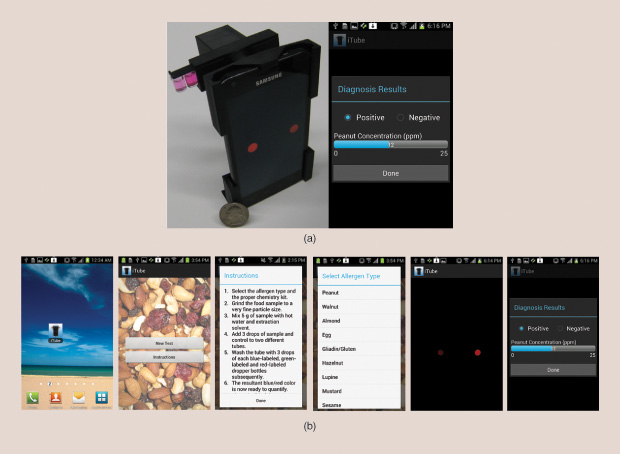
A few years ago, Ozcan created the iTube (Figure 2), a portable device that attaches to a smartphone and uses the phone’s camera to analyze food samples. After a food sample is ground up and mixed with water, a solvent, and other reactive liquids, it is measured optically for allergen concentration through the iTube platform. The kit digitally converts raw images from the cell phone camera into concentration measurements detected in food samples, according to Ozcan. Beyond just a “yes” or “no” answer as to whether allergens are present, he says, the test can also quantify how much of an allergen a sample contains in parts per million, a sensitivity needed for users to be reasonably sure that an allergen won’t cause a life-threatening reaction. His team successfully demonstrated a test for the presence of peanuts in commercial cookies in 2012. The device, which Ozcan plans to commercialize, could potentially test other allergens as well, although one drawback presently is that it takes about 20 minutes for a sample to be analyzed.
Testing Food with High-Tech Tools
Other companies have looked to near-infrared spectroscopy— a light-based technique for identifying materials based on reflected wavelengths—to design portable food testing kits to scan food quickly but with less accuracy than the iTube.
SCiO is one such scanner, able to analyze materials with an optical sensor and spectrometer and send that data to the cloud to identify materials. Right now, the device is in beta testing, and the company says there may be a variety of applications for it, including food sensitivities.
“Using our technology is not adequate for the level of sensitivity required by people with severe allergies,” says Dror Sharon, SCiO chief executive officer (CEO) and cofounder. “Having said that, there is a possibility where it might be helpful; for example, we’re able to tell different types of oils and identify milk, which could be useful.”
Another such device, TellSpec, was developed by Arizona-based Isabel Hoffmann and her team (Figure 3). CEO Hoffmann founded the company after her daughter developed a gluten reaction following their move to the United States from Europe. In one recent situation, a friend gave her daughter a cookie, insisting it was gluten free. The daughter took a bite, felt her lips swell, and used the scanner to confirm it had gluten. A trip back to the bakery where the cookie was bought confirmed that while the cookie was gluten free, the icing on it was not. These types of mistakes and oversights are dangerously common occurrences, as anyone with food sensitivities knows.
The TellSpec food sensor is not just about food preference but food security, says Hoffmann. TellSpec uses a combination of machine-learning and bioinformatics techniques to test for food ingredients and contaminants—currently the algorithms can identify dairy, gluten and soy, calories, fats, proteins, fiber, carbohydrates, sugars, and glycemic index, with programs in the works to spot eggs and chemicals such as melamine (which, according to Hoffmann, is often illegally used as a replacement for protein in food adulteration). “Our goal is to create a clean food revolution,” says Hoffmann, “and help people see what they didn’t even know they were exposed to.”
While handheld spectroscopy cannot now detect allergens with an accuracy of parts per billion, the technology may become robust enough to do so in a few years. “The full spectral range of nearinfrared detection is 780 to 2,500 nanometers,” says Hoffmann, whose product goes to 900–1,700 nm. “We can’t go to 2,400 today in a small device—there are some constraints in terms of the detection chips used, the scanner size, and the price. But it does not mean we won’t have this n a few years.” Hoffmann likens food scanners to cell phones, which used to be clunky, cumbersome, and expensive but evolved into something portable, now readily adopted by consumers.
Having a wider spectral range allows the scanner to detect more organic bonds, and so it is able to detect more ingredients. However, those suffering from serious allergies would still need to do a comprehensive scan of the whole item to ensure that it’s allergen free.
Harnessing Chemistry

Aside from spectroscopy, another approach for detecting allergens has been through chemistry: testing samples of food using antibodies. The Nima sensor (Figure 4), launching in 2017 by San Francisco-based 6SensorLabs, does just that. CEO and cofounder Shireen Yates, who can’t eat egg, dairy, or soy products because of severe sensitivities, met cofounder Scott Sundvor while attending the Massachusetts Institute of Technology. “We were excited about the idea of bringing people better data about what they’re putting into their body,” she says.
Nima consists of a mini testing kit based on developments in antibody technologies. A user can discretely insert a sample of the food to be tested into a one-time-use capsule, place it in the sensor, and a few minutes later see whether it contains what is being tested for. The device currently detects gluten at the FDA standard for gluten-free—20 parts per million.
“Integrating chemistry in a consumer electronic is a very big challenge, in part due to the nature of chemistry development, reproducibility, and scaling,” Yates explains. “Eventually, we want to get to a point where we can customize the product, so whatever ingredients you are concerned with could be in the capsule, such as, in my case, gluten, dairy, and soy.” The product is currently available for preorders and set to launch later this year.
Another device, the Allergy Amulet, will make use of test strips in a portable, pendant-like mechanism to let users test their food to confirm whether it is allergen free. The company that created the Allergy Amulet, a finalist with the Boston-based startup accelerator MassChallenge, aims to launch the device in 2018 with strips that can test for peanuts. The test strips consist of a polymer whose imprints match the shape and molecular properties of the allergens. The approach could be sensitive enough for peanut-allergy detection on the levels needed for sufferers, as the method has been tested at concentrations as low as parts per trillion with other molecules.
Tackling Sensitivities Before They’re a Problem
When it comes to life-threatening allergies, some companies are tackling the problem before consumers even get to a table.
French-based DBV Technologies created a peanut patch and a milk patch to help those with severe allergies desensitize to their allergen and increase their tolerance to peanuts or milk. The patches work by placing a small amount of the substance onto the skin to coax the immune system to become used to the allergen. The Viaskin Peanut Patch, slated to launch in 2018, is currently in phase III clinical trials after successful initial tests demonstrating that patients became more tolerant of peanuts after using the patch.
Similarly, San Francisco-based Aimmune Therapeutics is testing a pill that will prime users to become habituated to their allergens. The company is also in phase III trials for its pill, AR101, designed to help reduce peanut allergies.
As handheld devices and portable food test kits continue to miniaturize, speed up, and improve in conjunction with technologies aimed at lessening allergies, it may not be too many more years before we can forge forward, safe and confident in our food options.



