At the age of 14, Linda Griffith experienced such abnormally painful periods that her doctor had already put her on birth control pills. They helped but only a little. In graduate school, a boyfriend convinced her to go off the pills, and her periods became so painful, she couldn’t walk.

Griffith (right) was a high achiever, but her busy life at the University of California at Berkeley became unavoidably structured around her menstrual cycle. By the time she began her postdoctoral work in 1988, the pain was so intolerable that she was visiting her doctor monthly. Eventually, an ultrasound revealed a “small cyst” that her doctor recommended removing laparoscopically. The procedure, which was supposed to take only a few hours, lasted into the night. She didn’t wake up until later the next day. The flummoxed surgeon notified her that he’d discovered disease so extensive, he had to fully open her up. Only then, at 28, was it discovered that Griffith had endometriosis.
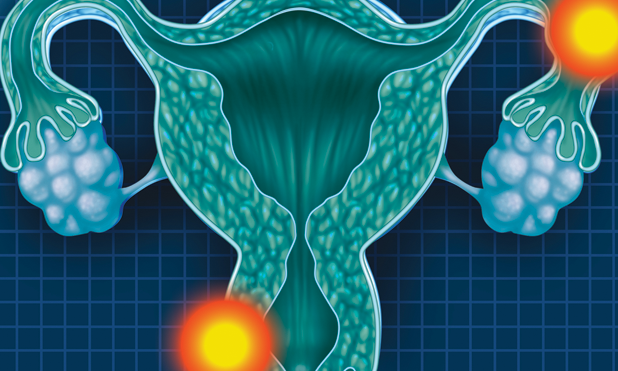
Endometriosis occurs when the endometrial tissue normally expelled from the uterus at the end of a menstrual cycle is instead trapped inside the body. There, like cancer, it continues to grow, eventually irritating the surrounding tissue. Over time, that irritated tissue can eventually form scar tissue, which, in severe cases, can cause pelvic tissues and even organs to adhere to each other like superglue. Women with the disease can suffer extreme pain and, in many cases, infertility. Although up to 10% of women in the United States are thought to have endometriosis, the cause remains elusive. There is no one culprit but rather a constellation of genes influenced by environmental factors like chemical exposure and stress, creating a degree of complexity that has made the condition extremely difficult to treat.
Linda Griffith: Researcher and Endometriosis Patient Advocate
Despite the disease, Griffith’s career still boomed. She landed in the Chemical Engineering Department at the Massachusetts Institute of Technology (MIT), where she continues to run a molecular biomaterials and tissue engineering lab. In the 1990s, she gained fame for growing tissue-engineered cartilage in the shape of a human ear on the back of a mouse. In 2006, she was awarded a MacArthur Genius Grant for her work developing cell scaffolding for liver cell regeneration, and, in 2009, her lab developed a new way to culture liver tissues that revolutionized the field. This three-dimensional (3-D) organ-on-a-chip model allows cell cultures from multiple tissues to be organized on a microchip-like surface and so mimic the structure and function of native tissue. These devices make it possible to conduct experiments on and test drugs using real, live tissues outside the body.
And throughout all of those accomplishments, hidden from public view, Griffith struggled to treat her endometriosis, trying experimental drugs that damaged her liver, induced menopause, and whittled away 12% of her bone mass. For five subsequent years, she underwent extensive surgeries to address expansive areas of disease covering her intestines. Ultimately, she had a hysterectomy. She kept it all from her colleagues.
It wasn’t until her niece, at 12 years old, started having abnormally painful periods that Griffith was called to action. She suspected early on it might be endometriosis and alerted the doctor, who met the suggestion with sharp resistance. Her niece must be making things up to get out of school, the doctor said. Griffith was furious. “No one ever took me seriously,” she said, “and this just all came back.” Eventually, she persuaded her niece, then 16, to switch doctors and undergo a procedure that revealed a pelvis filled with painful lesions. Her appendix was so covered with endometriosis, it had to be removed.

“Recognition of this as a disease is really important, because a pediatrician is really not trained to recognize endometriosis,” explains Asgi Fazleabas, professor and director of the Center for Women’s Health Research at Michigan State University (right). Girls with very severe menstrual pain are often told this is part of growing up and that they should just put up with it, he adds.
Around this time, Griffith’s doctor, Keith Isaacson, began pushing her to start working on the disease. Endometriosis researchers needed a model system of the uterine lining to see how the tissue invasion occurs in the first place. Griffith had been making these types of models for the liver, and Isaacson thought a similar model could be useful in this case. Griffith was reluctant to undergo the risky business of changing tacks in her research, but her niece’s experience was fresh on her mind, and she realized that she was in a unique position to make a difference. As a patient, she understood that experience intimately, but as a member of the National Academy of Engineering, she also had a podium. “I can speak as the patient to the doctors in a way that no one else can, and they listen,” she says. “It’s a very powerful platform to have, and I take it very seriously.”
The Center for Gynepathology Research
In 2009, Griffith teamed up with Isaacson to form the Center for Gynepathology Research (CGR) at MIT. They kicked off with funding from an anonymous foundation grant of just under a million dollars and launched the center with a star-studded event featuring Padma Lakshmi, host of the television series Top Chef, who herself suffered from endometriosis and has established her own endometriosis foundation.
The center was originally built on Griffith’s and Isaacson’s skill sets—systems biology, tissue engineering, and clinical gynecology—but today includes more than eight core researchers, all at MIT, and 11 collaborators and advisors representing a spectrum of biological and engineering fields across the country. CGR is unique in that it takes an engineering approach to tackling gynecological diseases, whereas most facilities approach them in other ways, Griffith explains.
CGR’s first major milestone came in 2014, when researchers there identified a group of 13 proteins present in the pelvic fluid of women suffering from particularly severe forms of endometriosis. These were all cytokines produced by macrophages, cells such as white blood cells that are usually found around the sites of infection. This was a breakthrough discovery, the first in a long time for the disease, and a promising one for developing a noninvasive test. Currently, the only existing diagnostic involves surgery. The work also identified a drug which inhibits the specific immune reaction that ultimately produces these proteins, suggesting there might already be a ready-made, targeted way to reduce inflammation in patients severely inhibited by the disease. The results still need to be replicated, so investigations are under way in a number of countries, including Brazil and Norway.
Going Beyond Endometriosis

But the center is also tackling more than just endometriosis. Katharina Ribbeck (right), a professor of tissue engineering at MIT and a core investigator at the center, studies the properties of cervical mucus to assess risk for preterm birth. Ribbeck’s studies used 3-D tissue engineering principles to model 3-D mucus matrices. “We see the same exact phenomenon for microbes in that the mucus matrix around microbes influences microbial growth,” Ribbick says. Something about the structural features of the mucus is significant in acting as a barrier, but what, exactly, remains a mystery. In her previous work, Ribbick determined that the physical and chemical properties of cervical mucus play a much larger role in determining pregnancy outcomes than was previously thought. The interplay between cervical tissues and mucus is poorly understood, but it is likely a significant piece to the puzzle, she thinks.
Ribbeck is angling for a collaboration with another affiliated CGR researcher, Caroline Mitchell, an obstetrics and gynecology practitioner at Massachusetts General Hospital who studies the vaginal microbiome, specifically bacterial overgrowth and imbalances in the vagina known as bacterial vaginosis. Infections can cause a plethora of problems if they ascend the cervix, including infertility, preterm birth, and pelvic inflammatory disease, and may also increase vulnerability to sexually transmitted infections like HIV. Using Ribbeck’s 3-D mucus matrices, the two scientists hope to collaborate on a project to systematically study the interplay between the microbial environment, mucus, and tissues to better understand the factors contributing to infection.
Better Together
Gynecological diseases are poorly understood not only because they are complex but also because research is desperately underfunded. “It’s actually almost a scandal how little funding there is at the National Institutes of Health [NIH] for gynecology problems,” Griffith argues.
It was only about a year ago that an NIH gynecology branch was even created. Previously, all gynecology was under fetal/maternal medicine. “It’s like everything about you that’s important is having a baby,” say Griffith. “It’s not that fetal/maternal medicine isn’t important—that’s incredibly important—but it puts a huge burden on a relatively small budget to have to fund all of gynecology,” she continues.
“Endometriosis alone is a [US]$22 billion to [US]$95 billion problem,” explains Fazleabas, one of the few recipients of NIH funding for gynecological research. The amount available, he says, is only enough to provide for maybe one or two grants, and, “as a result, many of these diseases continue to be just continuous problems.” His research center and CGR, for which he is a collaborator and advisor, have therefore turned to philanthropy and previously obtained grants.
Griffith has used her organ-on-a-chip program, funded through the Defense Advanced Research Projects Agency, to build a 3-D model of the endometrium she has shared with other institutions. “You find ways to not compete with the people who are already in the field, because they need to continue being funded,” she offers. She sees the center’s role in the field as a provider of tools for clinical researchers such as Fazleabas.

That’s worked well so far. One collaborator, Kevin Osteen, director of the Women’s Reproductive Health Research Center at the Vanderbilt School of Medicine in Nashville, Tennessee (right), is using Griffith’s organ-on-a-chip model to investigate environmental triggers for endometriosis. He, in turn, consults with CGR about how they might use their bioengineering techniques to focus on cell behavior associated with the disease. Osteen developed his own research center in the late 1990s that at first focused primarily on endometriosis but has since expanded to work on preterm birth and, more recently, ovarian cancer. Over the years, Osteen has also helped colleagues across the country develop other centers at their own universities, including Yale, the University of California San Francisco, Northwestern, and Griffith’s program at MIT. “We help each other get grants and collaborate,” he says. “There are a lot of people who are motivated to do this kind of work, and we all have to go find funding for it.”
Looking to the Future
However dire the funding environment for gynepathological research currently may be, many in the field, including Griffith, Fazleabas, and Osteen, are optimistic that the situation is changing. At the moment, the change is largely taking place at the societal level. “Women have not felt, really, that they could talk about things associated with painful periods and such, or painful intercourse,” Osteen explains. “These were not subjects that women of my generation were comfortable talking about.”
But these days, younger women are taking ownership of their health, talking about their below-the-belt health issues on blogs, researching them online, and coming to their doctors already educated about these conditions, Osteen continues. “I think the young, millennial generation in particular, they will change the face of this. They’re not going to be silent about it, nor should they be.”
Fazleabas thinks this grassroots awareness is what will ultimately lead to more opportunities for funding at the federal level, and then it’s up to the scientists to share their findings. “We need to do a better job as scientists,” he says. “It’s our responsibility to go out there and let people know what we do is important.”
But making the science appealing to scientists, Griffith believes, is important too. “My job is partly to just frame things so that my colleagues can see them as exciting problems, and not, ‘Ew, it’s that period.’”
For More Information
- A. S. Critchfield, G. Yao, A. Jaishankar, R. S. Friedlander, O. Lieleg, P. S. Doyle, G. Mckinley, M. House, and K. Ribbeck, “Cervical mucus properties stratify risk for preterm birth,” PLoS ONE, vol. 8, no. 8, pp. 1–7, 2013.
- American Society for Reproductive Medicine. (2017, Mar. 3). Resources, ASRM Patient Fact Sheet: Endometriosis. [Online].
- S. Simoens, L. Hummelshoj, and T. D’hooghe, “Endometriosis: Cost estimates and methodological perspective,” Human Reproduction Update, vol. 13, no. 4, pp. 395–404, 2007.
- M. T. Beste, N. Pfaffle-Doyle, E. A. Prentice, S. N. Morris, D. A. Lauffenburger, K. B. Isaacson, and L. G. Griffith, “Molecular network analysis of endometriosis reveals a role for c-Jun-regulated macrophage activation,” Sci. Translational Med., vol. 6, no. 222, p. 16, 2014.
- National Institutes of Health, U.S. Department of Health and Human Services. (2016, Apr. 4). Budget. [Online].