Since the dawn of additive manufacturing technologies in the 1980s and 90s, now commonly named 3D printing, the possibility of processing raw materials into freeform designed objects with unprecedented shape complexity opened new avenues for the development of medical devices. Indeed, the geometries of nature and the human body are extremely multifaceted, with even fractal-like or multiscale levels of detail, counting with functional gradients of properties, including topology and topography optimizations, to cite some interesting features. In consequence, classical subtracting manufacturing technologies, shape forming tools, and mass production chains are suboptimal for personalizing medical devices and adequately emulating life.
New manufacturing paradigm is transforming health care
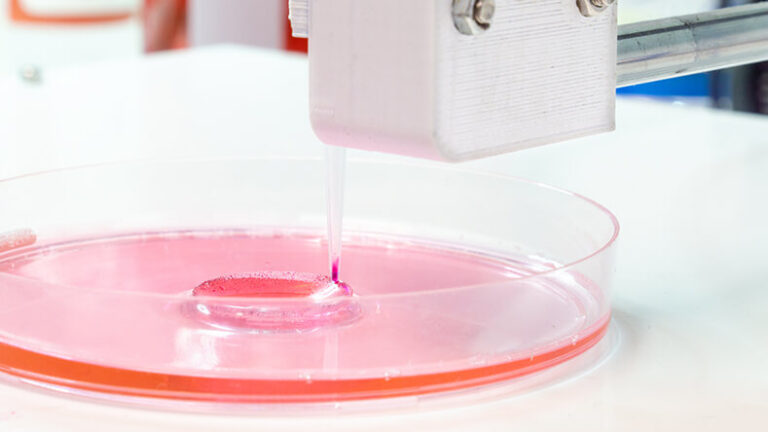
Already in the last decade of the 20th century, 3D printing led to a wide set of interesting medical applications linked to surgical training and planning, orthoses and surgical guides for safer interventions, ergonomic appliances, and even personalized implants designed using patients’ medical images as input. 3D printing was also crucial in the birth of tissue engineering, as additively manufactured scaffolds employing biomaterials found extensive application as in vitro cell culture systems and in vivo solutions for tissular repair [1]. Subsequently, a progressively increasing materials portfolio, along with the enhanced precision, improved performance and throughput of industrial printers, and the advent of bioprinting (for additively processing biomaterials and living cells) have made us dream of fabricating patient-matched functional tissues and organs for regenerative medicine [2].
However, 3D printed medical devices (and even 3D bioprinted constructs in almost all cases) still lack the dynamism of living tissues and organs, do not evolve according to patients’ healing and growth processes, and cannot radically transform their shape to foster the improved interactions with the environment that 4D printed biodevices would enable. Such fourth dimension, as usual, is time: 4D printed objects can go through one or several metamorphoses, sometimes in a reversible manner, after being created by employing special combinations of geometries, materials, and additive manufacturing technologies.
4D printing in medicine: Potentials and challenges
Interestingly, for almost two decades now, researchers in additive manufacturing have explored ways of obtaining shape-morphing or “smart” devices, normally resorting to the promotion of inner stresses during printing, to the printing of mechanisms, kinematic chains and textiles, to the design of soft stimuli-responsive structures, or to the additive manufacturing with shape-memory and multifunctional materials, among other options [3], [4]. The coining of “4D printing” as integrative term is more recent [5], [6]. In any case, the 4D printing movement synergizes with previously investigated applications of 3D printing to health care and contributes to the ongoing paradigm shift in the biomedical industry, aimed at massive customization as an alternative to traditional mass production, as further explained.
Shape transformations are intrinsic to life and drive our fate since embryonic development and organogenesis, through birth and childhood, along adulthood and toward death. Smart medical devices, taken to the extreme, should not only be able to monitor their own state and the health of their hosts and to respond to external stimuli adjusting their functioning parameters, but should also be able to transform their shapes during their interactions with humans, according to the needs of surgical and therapeutic procedures and to the healing, growth, and remodeling processes of patients. Exploring design principles oriented to 4D printing and research efforts aimed at the development of 4D printed medical devices, would arguably bring us closer to the desired smart and personalized medical devices of the future.
Among clear applications for 4D printed medical devices, it is important to highlight:
- surgical micromanipulators capable of repeated actuations printed in working position and bound to outperform medical actuators obtained by assembling several components;
- thrombectomy devices for treating stroke, meshes for percutaneous nephrolithotomy, and transcatheter stone extractors and retrieval baskets;
- personalized and minimally invasive cardiovascular implants including shape-morphing valve structures for reducing leakage and stents for aneurysms in Y-shaped bifurcations;
- smart printed textiles as cardiac support patches or meshes for reinforcing soft tissues (i.e., hernia repair), in all cases implantable in a folded way for subsequent deployment;
- minimally invasive tissue engineering scaffolds and articular implants obtained by self-assembly of tiny building blocks delivered using endoscopic or laparoscopic procedures;
- evolutive implants capable of modifying their shape during patients’ healing, of special relevance for large defect restoration involving several months of postoperative treatments;
- dynamic implants able to modify their shape during patients’ growth processes, of great significance for pediatric cardiovascular surgery and for articular and maxillofacial repairs.
Despite the enormous potential benefits of 4D printing, especially if the additive manufacturing of high-performance structures using smart alloys and ceramics is further developed, it is necessary to carefully analyze fundamental ethical aspects related to this emergent paradigm. As happens with artificial intelligence, internet of things, human-machine interfaces, smart robotics, and other rapidly advancing technologies, 4D printing provides us with new ways to interact with (and even reengineer) the human body. The fact that the potentials and impacts of this new manufacturing paradigm are not yet clear enough, together with the current limited access to medical 4D printing technologies and to the related knowledge on design strategies for 4D printing, raise important ethical concerns, which should be clarified and taken into account in parallel to any research carried out linked to 4D printed medical devices, as examined below.
Ethical issues of 4D printed medical devices
Before approaching the ethical issues of 4D printed medical devices, it is important to analyze already existing pioneering and inspiring studies on the ethical issues of 3D printing technologies [7], [8] and of 3D printing applied to medicine [9], [10], [11], [12]. Compiling from selected references, experts tend to agree that 3D printed medical devices may be ethically concerning with regard to the following points:
- Safety: 3D printing is redefining product design and production, and a shift from centralized toward decentralized manufacturing is perceived. In the medical field this can promote personalization and point-of-care solutions, although the risks associated to decentralized quality controls should be carefully addressed and raise ethical concerns.
- Environmental impacts: The mentioned decentralized production should minimize environmental impacts related to transport, thanks to products and even medical devices downloadable and printable from the cloud. Positive as it may seem, some unknowns should be answered, linked to the use of innovative materials like printing filaments or sintering powders, whose health and environmental risks should be systematically addressed, also connecting with safety. Tracking and recovering used products, through reconditioning, reusing, or recycling, in decentralized production and supply chains is also more challenging, which may have negative environmental impacts. Life cycle analyses for 3D (and 4D) printed medical devices should be performed and compared with the statu quo.
- Economic challenges: Reformulating the biomedical industry through 3D printed personalized solutions will impact labor demand, as through automation fewer workers will be needed in traditional production chains. However, other profiles will be needed, including managers and technicians of printing “farms,” technology developers, materials researchers, and designers for additive manufacturing. The final goal would be to contribute to decent work worldwide, through interconnected design and printing hubs, and through this paradigm change, which involves the sharing of knowledge and good practices, reach high-quality personalized and affordable medical devices.
- Responsibility and intellectual property: Traditionally, medical devices’ manufacturers were responsible of efficacy and safety, and accountable for eventual damage inflicted to patients through malfunctioning products. In 3D-printed health care technologies, the responsibility chain should be probably adjusted, especially if delocalized printing of designs shared online becomes mainstream. The accountability of designers (and users) sharing designs (and design modifications) of medical products through online cocreation environments, as well as the measures established to follow design modifications, to document the designs and their evolutions, to control quality in delocalized production, should be carefully analyzed by regulators. At the same time, innovative ways of recognizing and rewarding intellectual property in the emerging collaborative design and printing platforms should be also explored.
- Privacy and patients’ data: 3D printing has evolved in parallel to the makers’ movement, users and designers that cocreate and share 3D printable models, modifications for existing designs, and add-ons for 3D printing hardware and software, among others. Many medical applications of 3D printing have emerged in these collaborative platforms and their results are shared through environments like Thingiverse, GrabCAD, and GitHub, to cite a few. In these online infrastructures, among usually shared “objects” we can find 3D printable models of several human body parts including bones and digitalized heads, faces, etc. Many of these models are created by employing medical imaging and scanning technologies combined with specific software for segmentation and 3D geometry generation. This exchange of information may importantly affect patients or users’ privacy, which should be considered for implementing ad hoc information management procedures. In any case, informed consent should be obtained if patients’ data are going to be used for fostering research and innovation in the field of 3D printed medical devices.
- Equity and health care for all: 3D (and 4D) technology developers should focus their efforts on employing these innovative tools, not only for fostering health care revolutions, but also guaranteeing that the medical solutions achieved will be as accessible as possible, even leading to personalized solutions that both technically better than the state-of-the-art and cheaper for health care systems and users. Through knowledge-based approaches to additive manufacturing this may be possible.
- Human enhancement: 3D printing technologies and 3D printed orthoses and prostheses can be employed for body repair and reconstruction, but may be also used for human enhancement purposes and even for frivolous body modification practices (i.e., subdermal horn implants). These latter practices and the resources committed to them are ethically concerning and should be carefully analyzed. Debates on the enhancement of human capabilities and on the accessibility of human enhancing technologies are critical.
- Lack of regulations and standards: Overall, 3D printing resources and 3D printed medical devices seem to be advancing at a much more rapid pace than the regulations and standards of the biomedical industry. Existing regulations, even the newer ones like the EU Medical Device Regulation 2017/745, are still unsuited to the radical health care transformations that 3D (and 4D) printing technologies herald. These include not only open-source medical devices, but also eventual do-it-yourself medical devices, which are challenging to regulate and track, and could become potentially harmful.
Besides, 4D printing affects the aforementioned issues, making them even more critical from an ethical perspective, and brings new concerns into play.
- Regarding risks for users and patients, it is important to understand that designing for 4D printing is essentially much more challenging than following current design for additive manufacturing strategies focused on 3D printing. The use of quasi-living smart materials and unconventional structures, the eventual incorporation of autonomous decision-making subsystems for triggering the shape transformations when needed or the stimuli employed for the metamorphoses, which may include heat, electricity, light, chemicals etc., can importantly affect patients’ health and safety if inadequately designed and managed, which includes possibilities like piracy and hacking of 4D devices. Therefore, risk management procedures and usability risk assessment strategies should be adapted to 4D printing technologies, taking into consideration not only the mentioned design challenges, but also the fact that many 4D processes are triggered thanks to the use of special printing materials, involving nanofillers and smart nanomaterials, whose health impacts are concerning. These increased health concerns affect patients, but also users of the devices, like surgeons and nurses, and the actual manufacturers employing the 4D printers.
- About environmental impacts, 4D printable materials and 4D printing technologies are yet not so well understood, and so are their environmental impacts, which may be more concerning than those arising from 3D printing, again due to the use of functionalizing nanoparticles for the development of smart printable materials and for the triggering of shape changes in 4D components. Systematic application of lifecycle assessment procedures to 3D and 4D printing should be an essential part of the documentation asked for certification purposes.
- In terms of responsibility and intellectual property, new ethical concerns arise being the designs more challenging, potentially risky, and innovative, as previously explained. Furthermore, 4D printed implants may provide solutions for pediatric surgery, by means of evolutive implants or prostheses with delayed actuation, according to the grow processes of children. Some of these devices may be implanted in children, for which their parents normally decide and assume the responsibility following doctors’ indications. However, part of the therapeutic action of the 4D implant may be performed once these children are already adults and want to decide by themselves. Hence, irreversibility may become of vital importance and should be considered from the design stage. In addition, 4D approaches are per se highly innovative, and intellectual property management becomes even more relevant than in 3D printing.
- Concerning, equity and health care for all, 4D printable materials and 4D printing technologies are more expensive than their 3D counterparts, which may delay their potential benefits reaching health care and affect the desired democratization. As explained below, educational initiatives may be fundamental for compensating this.
- Considering human enhancement possibilities, 3D printing (and 3D bioprinting) technologies have been employed for human enhancement purposes, in most cases righteously compensating for a lesion or disease. However, these technologies also connect with the concept of technological immorality, and the emergence of 4D printing (and 4D bioprinting) resources just expand these potentials for transhumanism and should be researched and developed under the supervision of ethical committees. As mentioned, the triggering of metamorphoses can rely on decision making subsystems, which may be biased, if relying on wrongly trained artificial intelligences, or may be even hacked in unusual but highly concerning cases. The human enhancement technology might thus become a wicked human control tool in fatalistic but still conceivable scenarios. In addition, in some straightforward designs or configurations, 4D printable medical devices could remain latent after implantation, until employed for assisted suicide purposes, which leads to additional ethical debates. Finally, eventual dual uses of these 4D technologies and products should be carefully analyzed and prevented.
Toward the future
4D printing emerges as a shape-shifting manufacturing paradigm for the health care industry, with remarkable potential for fostering smart and personalized medical devices that reach patients worldwide, even in remote and in low- and middle-income settings, if these technologies are adequately deployed and if innovative design strategies for sustainable and equitable 4D printing are developed. As with any innovative transformative set of technologies, education is pivotal for ethical application, straightforward and safe societal transfer, sustained economic growth, and minimal undesired side effects. In the areas affected by 4D printing, designers, materials developers, and manufacturers should receive the adequate training; but also, health care professionals, users and patients should be instructed in the future uses of 4D biodevices and involved in the achievement of these progresses.
The incorporation of these topics into already existing engineering programs of study can be quite directly accomplished, through seminars and workshops, resorting to dedicated final degree theses or by including new modules into manufacturing courses or arranging new courses on 4D printing and its applications. Likewise, specialization or even Ph.D. programs on 3D and 4D printing for health care would provide professionals with in-depth knowledge and contribute to research in the field. In all these actions, finding space for addressing the ethical issues of 3D and 4D printing and understanding how to address them along innovative product design projects would be essential. As regards users and patients, user-centered design methods and design for usability, through which safer products are achieved, should be fostered. Activities for the joint interaction of technologists and end users should be organized, either as seminars and workshops, through service-learning cocreation actions or even linked to the collaborative organization of scientific-technological fairs, open-days, and exhibitions focused on 4D systems. Policy makers and regulators should be also involved in the training process, which should in turn lead to well-trained taskforces contributing to correcting the highlighted lack of specific standards. Through the promotion of educational actions related to open-source medical devices and technologies it is expectable that 4D printing will impact society more rapidly and based on equity principles.
Finally, it is necessary to point out that this study has not considered the specific (and even more complex) ethical issues linked to 4D bioprinting, processes involving both biomaterials and cells and directly related to the biofabrication of tissues and organs. The ethical issues of 3D bioprinting have been already covered in detail by colleagues [11], [12] and 4D is not yet mature enough for clearly addressing how it will transform bioprinting. This will be the central topic of future studies.
Acknowledgment
The author acknowledges the support of two research and innovation projects dealing with the design of innovative 4D printed medical devices and with the development of innovative materials and technologies for medical 4D printing: 1) “iMPLANTS-CM: impresión de metamateriales empleando aleaciones con memoria de forma y gradientes funcionales para una nueva generación de implantes inteligentes,” funded by the “Convocatoria 2020 de ayudas para la realización de proyectos sinérgicos de I+D en nuevas y emergentes áreas científicas en la frontera de la ciencia y de naturaleza interdisciplinar” funded by Comunidad Autónoma de Madrid (ref. del proyecto: Y2020/BIO-6756) and 2) “BIOMET4D: Smart 4D biodegradable metallic shape-shifting implants for dynamic tissue restoration,” funded by the European Union’s Horizon Europe Research and Innovation Program under Grant 101047008. Views and opinions expressed are those of the author only and do not necessarily reflect those of the funding bodies.
References
- A. D. Lantada and P. L. L. Morgado, “Rapid prototyping for biomedical engineering: Current capabilities and challenges,’’ Annu. Rev. Biomed Eng., vol. 14, pp. 73–96, Apr. 2012.
- R. Langer, “Tissue engineering: Perspectives, challenges, and future directions,’’ Tissue Eng., vol. 13, no. 1, pp. 1–2, 2007.
- G. Ehrmann and A. Ehrmann, “3D printing of shape memory polymers,’’ J. Appl. Polym. Sci., vol. 138, no. 34, p. 50847, 2021.
- A. D. Lantada, Handbook of Active Materials for Medical Devices. PAN Stanford Publishing, CRC Press, Taylor & Francis, 2012.
- S. Tibbits, “4D printing: Multi-material shape change,’’ Architectural Des., vol. 84, no. 1, pp. 116–121, 2014.
- A. S. Gladman et al., “Biomimetic 4D printing,’’ Nature Mater., vol. 15, pp. 413–418, Jan. 2016.
- J. Maric, F. Rodhain, and Y. Barlette, “3D printing trends—Discussing societal, environmental and ethical implications,’’ Manag. des Technol. Organisationnelles, vol. 6, pp. 127–138, 2016.
- S. Dodds, “3D printing raises ethical issues in medicine,” ABC Sciences, Feb. 11, 2015.
- E. Neely, “The risks of revolution: Ethical dilemmas in 3D printing from a US perspective,’’ J. Sci. Eng. Ethics, vol. 22, no. 5, pp. 1285–1297, 2016.
- S. Wild, “3D printing and the murky ethics of replicating bones,” UNDARK, Oct. 1, 2020.
- N. Vermeulen et al., “3D bioprint me: A socioethical view of bioprinting human organs and tissues,” J. Med. Ethics, vol. 43, no. 9, pp. 618–624, 2017.
- A. Kirillova et al., “Bioethical and legal issues in 3D bioprinting,” Int. J. Bioprinting, vol. 6, no. 3, p. 272, 2020.