First, Deliece Hofen drops the pill into hot water to soften the outside coating. Then, she slices through the center of the pill with an X-ACTO knife and squeezes the isotretinoin inside into a syringe. With the drug in liquid form, she can now administer it to her ten-year-old son Brandon. “The problem is...some of [the isotretinoin] is still left inside of the capsule and I’m not getting an exact dosage,” admits Hofen.
Every day, sometimes several times a day, parents around the country are giving their children drugs that are not officially approved for them, strapping too-large masks onto their small faces, and plugging their kids into devices that have been hacked. These are good parents—not corner cutters—but tireless mothers and fathers who are making an effort, under the most trying of circumstances, to provide their sick children with treatment and care through the only means available. Often, the available means are inexact or even painful—because they are designed for adults, not children.
Due to the small size of the pediatric market (approximately 13% of the health care market), pediatric medical products lag behind those for adults [1]. Pediatric care frequently involves repurposing drugs and products intended for the much larger, older bodies of adults. The consequences are clumsy workarounds, uncomfortable fittings that necessitate added clinical protocols and time, and a hampered quality of life for patients and their families. This “making do” sometimes works just fine; caregivers accept it as a matter of course. But for many, it’s a source of deep, persistent frustration.
“I actually called the manufacturer and they could tell me the weight of the capsule, but they couldn’t tell me the exact dosage of each of those capsules,” says Hofen in a video uploaded to the Web [2]. Her son Brandon has been fighting cancer since he was three; he is also autistic and cannot take pills. So, she began the soaking-slicing-squeezing routine to extract the drug in liquid form.
Like Hofen, parents of children who need ongoing medical care can come to realize after much research, many phone calls, and dead ends that, in some ways, they’re on their own when it comes to administering or improving their children’s care.
[accordion title=”This Invention Needs a Mother (Who Is an Engineer)”]
Alexis Schnaderbeck was born nine years ago with a complex set of medical problems. By the time she was one year old, her challenges numbered close to 15, including developmental delay, trouble swallowing, a blocked nasal airway, deafness, and visual impairment. Her mother, Catherine Rose, clocked hours at her daughter’s bedside over the course of several surgeries. She was watching over her daughter, of course, but she was also scrutinizing the machines that hummed through the night as part of her daughter’s care. Rose could not help it. “I’m one of those engineers that looks at how the hospital process works and notices a lot of things. Some days it was good that I noticed a lot, and some days it probably wasn’t the best.” One of the things the mechanical engineer observed was how many of the devices—24-hour monitors, X-rays, computed axial tomography scans, and CPAP masks—involved technology built by Philips.
Three years later, still shepherding Alexis through her medical treatments, stalled diagnoses, and ongoing care, Rose approached Philips about a job. “I want to work for you because I believe in what you’re doing,” Rose told them. Philips hired her and, in turn, came to believe in what she was doing: In 2013, they launched LightAide, a product Rose designed incorporating Philips Color Kinetics’ lights in a low-resolution screen. The device looks like the Lite-Brite toy from the 1970s but has no pegs and much brighter lights. Users interact with the screen through a switch, changing the lights’ color mode for example. It’s a captivating (and delightful, judging by the squeals of one user) way for visually impaired children to gain confidence and skill in their interactions with external stimuli (below).

Rose acknowledges that a big part of how she found support for LightAide was having the confidence to ask. She recalls sending the idea for the device to an executive who liked the idea but was not able to fund it. The idea could have stopped there, but Rose took it as implicit encouragement and a nudge to take another tack. She moved her idea on, approached another executive, and secured the backing she needed to proceed. Rose explicitly recommends this blend of “persistence and belief”—the idea that others are “trying to help even if they can’t give you the answer you want them to give you.” Innovators need momentum, and sometimes that momentum has to be sustained by how you perceive the world.
For parents who are not engineers or who cannot seek out jobs at a company with a health-care devices division, Rose advises networking. “You have no idea what connections the people you meet may have.” Rose is also enthusiastic about the growing prevalence of hacking events that seek out parent participation such as the MedStart hackathon at Tufts and Hacking Pediatrics (Boston Children’s Hospital). At these events, a parent acts as a subject matter expert, getting paired with a team of specialists who will have the technical competence or programming skill the parent may not possess. All the parent needs is a “crazy idea” or a pain point, something they want the medical device or care issue to tackle. It’s a little like a matchmaking event, bringing together people who have a problem and quickly pairing them up with those who can help solve the problem.

Hackathons notwithstanding, is Rose’s invention story so unusual that other parents of children with unmet pediatric health care needs cannot realistically emulate it? It’s true that as a mechanical engineer, she was uniquely positioned to address a medical need close to her heart by setting out to make it herself, with corporate backing. Yet, to examine the path that Rose took from the neonatal intensive care unit to, years later, a product launch, is to be reminded that what invention needs is not just a mother, but a mother with a serious case of persistence—and belief.
For More Information
LightAide in Action:
[/accordion]
“A lot of drugs used in pediatrics—the market’s not big enough to pay the cost of approval,” says pediatric pulmonologist Dr. Thomas Kinane. So, for example, even if a common drug may be known to help a certain type of heart lesion, the cost to manufacturers in obtaining U.S. Food and Drug Administration (FDA) approval far outstrips the market size, so that use of the drug is never approved. Using products and drugs off-label in pediatric health care is commonplace.
“There’s a fundamental gap in the marketplace and lack of incentive for major companies to invest in this area,” says Donald Lombardi, founder and chief executive officer of the Institute for Pediatric Innovation (IPI), a Massachusetts-based nonprofit that promotes pediatric device and drug development. Not only is the pediatric market small but it is fragmented into submarkets (from premature baby to teenager), further discouraging investment. (For a discussion on how a small pediatric market affects advances in pediatric cardiology, see “The Heart of the Matter” by David Chandler on page 12 of this issue of IEEE Pulse.)

And while there are challenges in bringing pediatric drugs to market, the pathway to commercialization for drugs looks like a freeway compared to the less-traveled road that pediatric devices take if they even go anywhere beyond “good idea.” Can strides made in pediatric drug development, then, model a better way forward for devices? This question was raised at last year’s Pediatric Surgical Innovation Symposium organized by the Sheikh Zayed Institute for Pediatric Surgical Innovation in Washington, D.C. Dr. Kolaleh Eskandanian, executive director of the institute, believes there are transferable lessons. “The government has done a great job both in terms of carrots and sticks to provide incentives to the pharmaceutical world. As a result, that industry has benefited and children have benefited from drugs that were tested specifically for kids,” she says.
Through legislation such as the Orphan Drug Act of 1983, economic benefits were tied to developing drugs for small markets (in this case, drugs for treating rare, or “orphan,” diseases). This type of legislation models how tax credits, boosted patent protection, marketing exclusivity, and clinical research subsidies can encourage medical innovation that would not otherwise occur.
However, some aspects of the pharmaceutical incentives model do not transfer precisely to device development because drugs and devices have different development trajectories. Marketing exclusivity, for instance, would not work in the same way since devices have a shorter product life cycle than pharmaceuticals and move into further iterations as soon as six months after reaching the market. Nevertheless, Eskandanian urges, “We want to learn from that experience…what has been made available to [to the industry] by the FDA and improvements that were made in clinical trials and postmarket surveillance.”
The FDA has already embarked on offering financial support for device innovation in the form of funding. On the heels of medical device legislation passed by the U.S. Congress in 2007 (and reauthorized in 2012), the FDA established the Pediatric Device Consortia Program. The most recent grant cycle of that program delivered seven grants totaling about US$3.5 million in 2013. To some, these funds (roughly a third of which is for actual product development) feel small in relation to the need. What the program can do, Lombardi explains, is enable “a few successful case studies that demonstrate…practices for augmenting the market system to make it work for babies and children [and] to set the stage for investment by the government at a scale that the challenge warrants.”
Kids-Only Design Complexities

The mandate for these grants acknowledges the specific challenges of pediatric device innovation (above and beyond the inherent difficulty of attracting big companies to invest in it). Designing products for use by children entails its own set of distinct starting points. In the first place, what is a child? “Pediatric” designates patients ranging in age from a preterm baby to a teenager. “The size and site that a particular device is interfacing with can vary by an order of magnitude over the course of a child’s development into an adult,” notes Lombardi. “So, at a simple level, if you’re doing something size dependent, you have to make a lot of them to address the range of sizes, and if you’re doing something that’s implantable, what do you do when the body quickly outgrows what you just stuck in there?”
There’s also the need to think holistically when designing for children. With adults, Lombardi observes, you may be able to think in terms of one organ system at a time, but with a preterm baby, a treatment could have myriad ramifications. A device that does not aerate a child’s lungs correctly could adversely affect the baby’s neural development. Additionally, as far as biocompatibility, the standards for bench, animal, and clinical tests in many instances have yet to be created for the youngest babies. And then there’s the social factor: the best product designs allow children, as much as possible, to do the things that healthy kids do and to not look like patients at school if they must wear devices all day.
Manufacturers are also designing for users who—at the youngest end of the spectrum—cannot speak for themselves. David Groll, who has developed and manufactured medical devices for several decades, points out another facet of designing for the youngest patients. “They can’t answer you directly,” he says, “so you rely on third parties, either the doctor, the nurse, the caregiver, the parents. Somebody who is not physically using the product is having to provide feedback on it.” Clues come from watching closely. “Does the baby seem comfortable? Are they squirming around, trying to pull the mask off their faces or able to rest comfortably wearing it and not trying to fight it?” asks Groll. “They get [the answers] through observation of the child’s behavior.”
In the case of respiratory masks, the ill effects of the mask have been obvious to clinicians and parents for years when they cause skin wounds or pressure ulcers on children’s faces. Adult masks are routinely used on children, and, to maintain the needed pressure, the masks are often secured so tightly as to injure babies’ more tender skin. Invasive respiratory masks, meanwhile, can erode a child’s septum or cause endotracheal tube damage. “You’re trying to fix the baby, give them the oxygen they need, and you’re causing damage, some of which will never heal and some that will heal only after months of pain and treatment,” laments Lombardi.

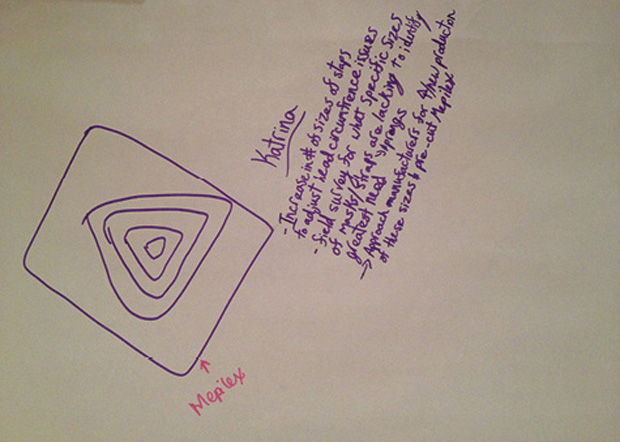
Because hospital-acquired conditions like these are no longer reimbursed by payers such as Medicaid and Medicare, hospitals now have added motivation to include them in their performance-improvement initiatives. A few years ago, as the payer policies changed, it occurred to Lombardi that this could alter the calculus of pediatric device innovation. His organization, IPI, which partners with a consortium of hospitals across the United States, examined these performance initiatives for instances where improved pediatric devices would mitigate a hospital-acquired condition and thereby lower the associated costs to the hospitals. Pressure ulcers rose to the top of the list, and IPI now has a 60-person working group focused exclusively on developing better pediatric respiratory masks (above and below). The Institute has also found a corporate partner and is negotiating an agreement to collaborate in the design of a pediatric-specific continuous positive air pressure (CPAP) mask.
“So we’ve got a model here where the end-user organizations, the customers, are funding the research to figure out what they need and to put together the opportunity plan to attract a corporate sponsor,” says Lombardi. In facilitating this alternate approach to need identification and investment, IPI found a way to link a sound business case to a historically neglected market.
This approach also exposes the back-door entry that may be needed to retrieve medical device data on a population that has not been properly tracked due to the proliferation of off-label usage. “Because these devices are used off-label, it’s hard to gather information on their effectiveness. Their indication is not necessarily for children; it’s for the general adult population, but clinicians use them for children,” says Dr. Eskandanian, who pioneered the first-ever Web-based adverse event reporting system used in clinical trials. “We only find out about these postmarket, off-label uses,” she continues, “when an adverse event is voluntarily reported or perhaps during case reports at conferences.”
In the case of the respiratory masks used on children, the adverse event data were not, so to speak, filed under “pediatric devices” but was instead buried within the category “hospital-acquired conditions.” That such data are effectively off the radar may come as a surprise, given the prevailing buzz about the era of big data. But, like many surprises, it’s also an opportunity. Consider what other insights around pediatric patient experiences and product effectiveness sit quietly in plain sight but unrecognized because the metrics around them have never been marshalled. A safe harbor that would permit data collection on off-label use that is the standard of care (as pediatric orthopedist Dr. Laurel Blakemore proposed several years ago) could offer one stab at reform.
“You cannot go buy a report and find out how many pediatric respiratory masks you need. No one is producing those reports,” Lombardi points out. “I’d like to see how we can pull together the data and [connect those] who are active in this area and have a consolidated marketplace where pediatric device innovations can be displayed and made available, and where the underlying data on the pediatric market and the market needs can be aggregated.”
Until such data are coherently, creatively, and more thoroughly collected, aggregated, and made accessible, the experiences of many pediatric patients will remain untold or tucked in a home video uploaded to the Internet by another tireless parent who hopes that maybe his or her story will reverberate beyond the ears of sympathetic friends and find its way to a research and development team somewhere.
References
- NHE Fact Sheet. [Online].
- Institute for Pediatric Innovation on Vimeo. [Online].



