“It may sound like it’s on the scientific fringe, but it’s not a pipe dream. This is actually happening.” When stem-cell researcher Dr. Kyle Orwig, of the University of Pittsburgh Department of Obstetrics, Gynecology, and Reproductive Sciences, made this remark, he was talking about the groundbreaking work that is generating eggs and sperm from skin cells. But he could have been talking about any number of assisted reproductive technologies (ARTs) that are rapidly advancing in research labs around the world and, in some cases, are starting to make their way into the clinic.
Most people are familiar with fertility drugs that induce a woman to produce eggs and with in vitro fertilization (IVF), in which sperm and eggs are combined outside the body and the resulting fertilized eggs are then transplanted into a woman’s reproductive tract. While both are still commonly used in clinics, new technologies are pushing the envelope on just how much science can do to improve men’s and women’s chances of becoming fathers and mothers.
The skin-to-gamete research is perhaps the most sensational of the technologies. In this work, researchers Mitinori Saitou of Kyoto University in Japan and Katsuhiko Hayashi of the University of Cambridge in the United Kingdom announced in 2013 that they had taken mature skin cells from an adult mouse and, from those cells, generated pluripotent stem cells that developed into primordial germ cells, which they implanted into sterile mice. About a quarter of the male and female mice began producing sperm and eggs, respectively. Hayashi followed up by combining the sperm and eggs in a petri dish and transplanted the subsequently fertilized eggs into female mice, which successfully carried the embryos to term and resulted in baby mice.
“That means that in principal, we could take a biopsy from the skin of either a man or a woman and turn it into eggs or sperm, so he or she could have their own genetic child from their skin cells,” Orwig says.
Saitou and Hayashi’s work still has significant safety and feasibility issues to overcome, but that doesn’t discount the achievement, Orwig notes. “It may be at least ten years before it makes it to the human clinic, and it may never make the transition, but just the concept of taking the skin, converting it into a pluripotent cell, and differentiating it all the way to eggs, sperm, and babies is a gargantuan developmental process to recapitulate this in vitro/in vivo model.”
This work in mice has yet to be replicated in humans, although several labs are trying. Orwig is collaborating with three of them, including the labs of Dr. Gerald Schatten, the director of the Pittsburgh Development Center; Dr. Renee Reijo Pera, the former director of the Center for Human Embryonic Stem Cell Research and Education at Stanford University and now at Montana State University; and Dr. Amander Clark of the University of California, Los Angeles Department of Molecular Cell and Developmental Biology.
“Dr. Schatten has shown that you can make round spermatids from stem cells, which is the step right before the production of spermatozoa, and Dr. Reijo Pera and Dr. Clark are also making good progress along those lines,” Orwig says. “In all cases, they’re using human stem cells, and although nobody’s made a mature sperm in a petri dish, these labs are doing work that is getting pretty close and is very intriguing.”
Stem Cells for the Clinic
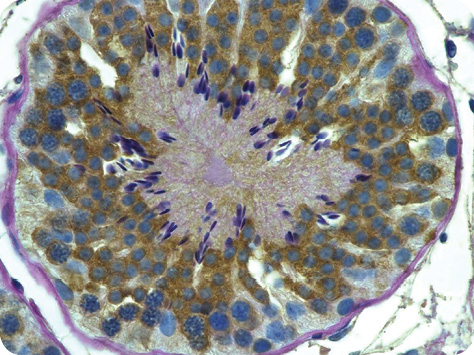
A bit closer to the clinic is Orwig’s own research designed to allow young male cancer patients to have children someday. Some cancer treatments can cause permanent infertility in men and prepubertal boys. Adult men have the option to freeze a semen sample containing sperm before initiating treatment to preserve their future fertility. This option is not available to prepubertal boys, who are not yet producing sperm, but Orwig hopes to change that by retrieving testicular tissue and using stem cell-based technologies to reinitiate spermatogenesis.
“We and others have developed the technology in a variety of animals, including monkeys, to retrieve sperm-producing stem cells from the testicular tissue,” Orwig explains. The idea is that the testicular tissue can be frozen prior to the initiation of the treatment, thawed at a later date, and processed to produce a suspension of cells, including spermatogonial stem cells, that would be transplanted into the testis of the now cancer-free but infertile individual to regenerate normal spermatogenesis. “Then he could have a baby the normal way by sexual intercourse, or if he could generate only a fraction of normal sperm rather than normal fertility, we could use ARTs to get the most out of the few sperm that he has,” he says.
Based on their success in animals and on several encouraging studies on human cells, Orwig and his collaborators think the technology is almost at the point where it can be used on humans. At present, 500–600 patients have had their testicular tissue frozen, he notes, and he is also recruiting patients to obtain additional biopsied testicular tissue. While some safety and feasibility studies need to be done, he believes the technology is mature and could be translated to the clinic within the next five years.
Perhaps the biggest challenge currently is obtaining a sufficient number of stem cells from the patient. “We anticipate that the number of stem cells in the testis is relatively low, and the number that we can retrieve in a small biopsy from the patient will be even lower, so we need to develop cell-culture technology that will allow us to amplify those cells before we do a transplant,” Orwig says. His and several other labs around the world are working on that issue.
In addition, this line of technology has another consideration: Is it safe to reintroduce tissue that was harvested prior to cancer therapy? “If we’re putting cells back into a patient, there’s a risk of putting a cancer back in too because you got the cells before they started their therapy,” he says. “That’s a critical issue, and we should not be too cavalier about taking these technologies to the clinic if it means putting a patient at risk.”
A Good Egg, a Good Embryo
As technologies advance and parents have more options available to them to improve their odds of having a child, one thing hasn’t changed. Parents still want a healthy baby. And that is another burgeoning area of ART research: What is the best way to tell the premium eggs and embryos from the others?
“One of the Achilles’ heels of in vitro fertilization is identifying which embryo is going to make a baby, and we’ve gone from the approach of transferring multiple embryos in the early days of their development—that’s what we used to do in the early to mid-1990s—to transferring fewer embryos at a later stage of development,” says Dr. Barry Behr, professor of obstetrics and gynecology at the Stanford University Medical Center and director of its IVF lab. In the mid-1990s, his interest was in developing an extended culture system to keep blastocysts (late-stage embryos) alive as long as possible. Some would die off, presumably because they were inferior, and that left the strongest, which became the candidates for embryo transfer. “IVF has evolved significantly since then to be more one of actively seeking those embryos that have the potential versus eliminating those that don’t,” he says.
A few possibilities arise. In one, the timing of cell divisions, or morphokinetics, is observed because those embryos that divide regularly are considered the best-suited embryos, Behr says. That hypothesis grew from tedious research that involved growing embryos on time-lapse microscopes, removing them at different stages of development and doing gene-expression analyses, and then making correlations between the gene-expression profile, the time-lapse, and the embryo’s ability to make it to the implantation stage. “That allowed us to come up with an algorithm that predicts viability,” he says. With that algorithm, Behr and his two coinventors could systematically watch cell divisions in an embryo over time without having to disturb the embryo or even take it out of its environment.
The three coinventors—a basic scientist, a clinical embryologist, and a photonics engineer—founded a company called Auxogyn in Menlo Park, California, and then stepped back to let the company further develop the technology and seek clearance from the U.S. Food and Drug Administration (FDA). The FDA granted approval in August 2014.
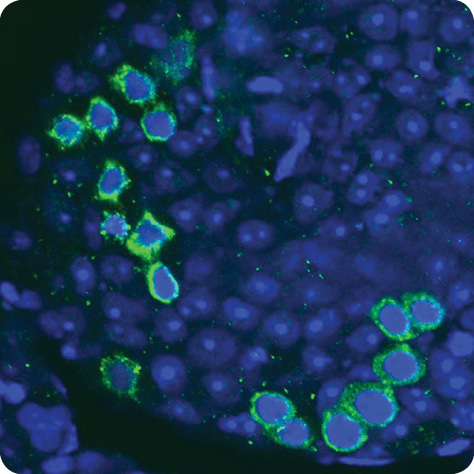
Morphokinetics is not the only way to select embryos for transfer. Numerous research groups are working on more accurate ways to assess whether embryos have any chromosomal abnormalities before they are transferred. One of them is a collaborative project involving molecular karyotyping, which scans chromosomes using molecular probes attached to arrays, explains Eric J. Forman, who is an assistant professor of obstetrics and gynecology and reproductive sciences at Rutgers Robert Wood Johnson Medical School and also a reproductive endocrinologist with Reproductive Medicine Associates of New Jersey.

Forman’s joint research group turned to single nucleotide polymorphism (SNP) arrays and comprehensive chromosome screening. “We did a study where we transferred two embryos on day three, one of which just had a single-cell biopsy. We were able, with this SNP array, to fingerprint the biopsied embryo so we could determine when it implanted and resulted in a baby and compare it to the embryo that had not been biopsied,” he says. In parallel, they transferred two embryos that were at the blastocyst stage (at least five days old) to each patient. One embryo had a trophectoderm biopsy, in which about five cells are removed from the outer layer of the blastocyst.

From this work, which was published in 2013, they discovered that a biopsy of a day-three embryo made it less likely that it would implant and result in a baby, but that a trophectoderm biopsy of a day-five embryo had no negative effect. At about the same time, they also realized that they needed to boost the processing time with the SNP array so that they could transfer the embryo while the woman’s body was still receptive. That led to the development of a quicker approach that utilized several marked polymerase chain reaction (PCR) assays on each chromosome. “A lot of preliminary testing and blinded cell-line studies were done to demonstrate that it was effective and accurate, and that it could be completed within four to six hours,” Forman says. “As a result, an embryo could potentially be biopsied on the fifth day of its development, a PCR could be done overnight, and a normal embryo could be transferred on the morning of the sixth day still within the window of time that a woman’s uterus would be receptive.”
Since their results showed that the SNP approach worked, the biopsy was safe for the embryo, and the technology could accurately identify a chromosomally normal embryo, the research group came to a decision, according to Forman. “We didn’t see any logical reason why single-embryo transfer shouldn’t become the standard for IVF not only for those older women who were the traditional candidates for preimplantation genetic screening but for all women.” Single-embryo transfer is a better option than the traditional IVF method of transferring two (or more) embryos because it reduces the potential for multiple births. Multiple births can cause complications for the babies and the mother, including preeclampsia, gestational diabetes, preterm delivery, Cesarean section, hemorrhage, and even mortality.
This conclusion led to another study headed by Forman to see whether single-embryo transfer with CCS was just as successful as double-embryo transfers (without CCS). The results, which were also published in 2013, showed no significant difference in successful delivery rates between the two groups (61% in the single-embryo transfer group versus 65% in the double-embryo transfer group). In addition, single-embryo transfer resulted in no twins, while nearly half of the mothers in the multiple-transfer group had twins. An ensuing study published in 2014 went further, revealing that the single-embryo transfer group had a significantly lower risk of preterm delivery, of having low-birth-weight babies, or of having any of their babies stay in the neonatal intensive care unit. In all, he says, “Not only did we get a similar number of deliveries, but the deliveries were safer and had healthier outcomes.”
The next step is to figure out why more than a third of embryos do not implant and result in a live birth even though they looked normal and tested as chromosomally normal. “We’re trying to figure out what else there is besides genetics that is having an influence. It could potentially be endometrial/uterine, hormonal, or other nongenetic factors that impact the embryo and embryo quality, possibly mitochondria or the energy metabolism of embryos,” Forman says. “There’s a lot that we still need to learn, but we’re making strides to continue to improve success rates and make this single-embryo transfer even more effective.”
Make it Natural
Another way to improve ART success rates is to look to the woman’s body. In particular, some researchers are culturing externally fertilized embryos in the female reproductive tract. IVF has traditionally required embryos to be cultured in incubators and clean-room environments, and while they are good systems, they have one big drawback. They are costly.
“The incubators are expensive to build because they have to have very sophisticated air-handling systems just to remove potentially harmful particles or organic compounds or to catalyze some of the volatile organic compounds (VOCs) that are found in ambient air,” says Dr. Kevin Doody of the Center for Assisted Reproduction of Dallas, Texas (Figure 6). “And because the incubators are electromechanical devices that can fail, there’s a whole lot of expense that’s involved in quality control and monitoring.”

The idea, then, is to replace the electromechanical incubators with a small device that utilizes the woman’s vagina as a natural incubator to support embryo development. Doody is now involved in a clinical trial to test such a vaginally placed incubator, called the INVOcell. Developed by INVO Bioscience, Inc. of Beverly, Massachusetts, the INVOcell device has an inner chamber designed to contain the culture medium and the eggs with sperm for fertilization and an outer chamber that isolates the inner chamber from vaginal secretions but still allows the passage of carbon dioxide and oxygen.
In Doody’s trial, he actually exposes the eggs to the sperm for a couple of hours in his lab and then puts up to ten eggs in the INVOcell and places it into the vagina, where the device remains undisturbed for five days. Afterward, the device is removed and the embryos are evaluated to determine which are optimal. “One or two are transferred back into the woman and if they are genetically healthy and normal, they should ‘hatch’ within 24 hours and proceed with the pregnancy in the normal way,” he explains.
For his trial, Doody randomly divided 40 patients so that 20 underwent IVF using a traditional incubator in the lab and 20 used INVOcell. As of late September 2014, when his study was nearly complete, he reported a more than 50% ongoing pregnancy rate in both groups of patients. “We’ve found that we’re able to grow embryos really well in the INVOcell device,” he remarks.
The major benefits of the system are that it cuts costs because it eliminates the need for quality control and a clean room, and it also makes IVF available to more people. “Currently, IVF is limited to metropolitan urban areas because it’s just not economically feasible to invest a couple of million dollars in an IVF lab in small towns, even in those with 100,000–150,000 people. INVOcell, on the other hand, could be available in more geographic areas, and because it’s a far simpler system, it would likely decrease the cost of an IVF cycle,” he says. “That’s important,” he adds. “Right now, a good percentage of the U.S. population is either priced out of IVF because it’s just not affordable for them or because it’s not available in rural areas.”
“Some expensive new technologies can be used to eke out the very highest in pregnancy rate, which is all well and good,” Doody adds, “but those technologies aren’t available to everybody, and ultimately our goal is to try to help all people build families.”
As of early October 2014, the FDA was reviewing INVOcell for use in the United States. Other countries are also running trials, and medical facilities in India began offering the INVOcell process in their practices in 2013.
Looking Ahead
Alternative embryo culture techniques, single-embryo transfer, and gametes from stem cells are just a few of the many possibilities afforded by advanced ART. Exactly how far science will be able to go, however, remains to be seen. “Many of these technologies are really in their infancy, and while there are considerable data out there to suggest that some will have application in the clinic, a lot of work remains to be done to establish feasibility and safety,” Orwig says. “It’s important that all of these technologies are developed robustly and responsibly.”
Safety is a number one consideration, Forman agrees. “As a field, the ART focus has begun to be on improving safety. In the earlier days of IVF, when laboratory conditions and technology were not as good as they currently are, the focus was primarily on trying to achieve pregnancy, so physicians and embryologists in this specialty compensated for the inefficiency of the whole system by placing multiple embryos into the uterus and hoping that at least one of them would take and result in a pregnancy.” Unfortunately, that sometimes led to multiple births, which extensive obstetrical literature has shown to come with higher risks of complication for the mothers and babies.
Things have changed in the past couple of years. “We’ve gotten better at culturing the embryos to a point where we can select fewer of them to transfer, and we’ve also gotten much better at freezing embryos (see “The Big Chill: Freezing Sperm, Embryos, and Now Eggs”) so that it’s not an all-or-none kind of thing where you’re concerned that you might lose embryos if you don’t replace them to the uterus,” Forman says. “All of those advances have really driven us to focus more on improving safety.”
[accordion title=”The Big Chill: Freezing Sperm, Embryos, and Now Eggs”]

Many of the ARTs rely on the ability to preserve sperm, eggs, and/or embryos, and that means freezing them. Sperm were frozen first, beginning as early as the 1940s with bull semen and 1953 with human semen. Embryos followed in 1983, but the freezing of eggs (oocytes) lagged. “There was a pregnancy in 1986 using a frozen egg, but the overall success rates for frozen eggs were much poorer compared to fresh eggs, partly because when the eggs were thawed, they just would not fertilize well,” says Lynn Westphal, associate professor of obstetrics and gynecology–reproductive endocrinology and infertility at Stanford University Medical Center.
The interest in oocyte cryopreservation returned after intracytoplasmic sperm injection (ICSI) resulted in the first births in the early 1990s. In ICSI, individual sperm are injected directly into an egg. This gave very good fertilization rates even when people substituted thawed eggs for fresh eggs, so the race was on again for new and improved egg-freezing techniques. “Initially people were using this method called slow freezing, which was the standard for freezing embryos at that time. Now people have moved to quick freezing, or vitrification,” Westphal says.

In the late 1990s, Stanford became one of the first places in the United States to use vitrification to freeze eggs, and although the initial users of the technology were prechemotherapy cancer patients, the audience soon expanded to include women who were delaying pregnancy but knew that age impacts egg viability. “As women get to be around age 40, at least half of their eggs are chromosomally abnormal,” Westphal explains.
The vitrification process has gone through many improvements, according to Barry Behr, who worked with Westphal to develop Stanford’s fertility-preservation program. He is also the national trainer for the Cryotech method of vitrification, which he describes as the latest and best method for quick-freezing. Invented by Masa Kuayama of the Repro-Support Medical Research Centre in Japan, Cryotech includes improvements in the storage vessels that contain oocytes as well as the culture media used to grow embryos. “As we learn about more stable and safer compounds, for instance, the media are continually updated and modified so that we now have this robust, evidence-based, and proven technology that we use for cryopreservation,” Behr says.
His lab’s contribution to the method has been in the operational aspects of using Cryotech for embryos that have been genetically screened. “We’ve made some modifications so that when we thaw them out, we can tell which embryo is which.”
At the same time, Westphal has begun conducting research to determine whether cancer patients who take advantage of fertility preservation have a higher disease recurrence rate than those who don’t and, so far, has found no difference in recurrence rates or in mortality, but that work is proceeding. She is also taking part in other studies to discover which women are and aren’t using their frozen eggs and why oncologists don’t always recommend cryopreservation to their patients who would be good candidates.
As that work carries on, the research behind cryopreservation will continue to advance because so many other ARTs depend on it. For example, the research group of Nicole Noyes, a reproductive endocrinologist at New York University’s Fertility Center, has reported as good a pregnancy rate with egg freezing as that achieved through conventional IVF cycles. Other programs have had similar success rates with oocyte freezing, and in 2012, the American Society for Reproductive Medicine removed the “experimental” label from oocyte preservation.
With every passing year, the ART options available to men and women multiply, and in many cases, they depend on the availability of viable and chromosomally normal eggs. Cryopreservation can help to provide them and allow for the birth of healthy babies.
[/accordion]
Research is also continuing to heighten the success rates of IVF. While they have risen, Forman asserts, “they still are nowhere near where we would like them to be, and that has led to this new movement toward improving the effectiveness of IVF and ART, and gaining more confidence in which embryos we transfer back to the woman’s uterus will result in a healthy ongoing pregnancy and delivery of a baby.” He adds, “This is an exciting story with increasingly better and safer outcomes, but we still have a way to go.”



