Mental disorders, characterized by impaired emotional and mood balance, are common in the West. Recent surveys have found that millions of people (age 18–65) have experienced some kind of mental disorder, such as psychotic disorder, major depression, bipolar disorder, panic disorder, social phobia, and somatoform disorder [1]. Specifically, in 2010, 164.8 million people in Europe were affected by such illnesses [1].
Such disorders are often chronic conditions that can be life-threatening, damaging relationships and performance. Depending on the specific disease, patients experience a sad and desperate mood with a lack of interest together with several other neurovegetative symptoms, including loss of appetite and sleep. Other symptoms, such as cognitive retardation, somatic pain, or functional symptoms (headache, dyspepsia, etc.), are frequent as well. Depressed patients might also experience thoughts of ruin, guilt, or death, including suicidal thoughts that might end in suicide attempts. On the other hand, maniacal patients express an increase in activity and an acceleration of thoughts. Rather than being a positive effect, these conditions are the cause of attention loss and prevent the patient from expressing a coherent stream of thoughts [1]–[4].
From the clinical point of view, the diagnosis of such psychiatric pathological conditions is based on clinical evaluations of symptoms self-reported by patients through interviews and scores on psychopathological rating scales. Although these interviews are “structured” (i.e., questions and their order are established and defined in specific manuals) and high rates of consensus can be achieved among specialists (psychiatrists and clinical psychologists), the diagnosis is always based on the clinician’s observations, the patient’s subjective description, and the physician’s interpretation of such a description. In other words, there are neither specific physiological nor biochemical markers that can be taken into account to objectify the diagnosis.
To give a pragmatic example, the most important diagnostic system is based on the criteria proposed by Diagnostic and Statistical Manual of Mental Disorders (DSM) edited by the American Psychiatric Association. According to this manual, the diagnosis of major depression, for instance, is based on the presence of five out of nine symptoms (similar cutoffs are applied for the diagnosis of other disorders). In line with this approach, a patient who has four symptoms of depressive episodes is not formally considered to be depressed. These considerations clearly lead to subjective interpretation and inconsistency.
This description portrays a dramatic scenario in which research and technological advances could greatly contribute and bridge the current gaps. Despite the fact that many studies have been carried out on several biomarkers, e.g., sleep quality, circadian heart rate rhythms, cortisol dynamics, and dysfunctions of the central nervous system and autonomic nervous system (ANS), none has attained an acceptable level of accuracy in clinical use to evaluate and predict the development of mental disorders. A possible explanation of such a failure could be related to the reduced observation time of assessment that has been taken into account. Moreover, continuous feedback to clinicians and patients on the status of the illness has been totally disregarded.
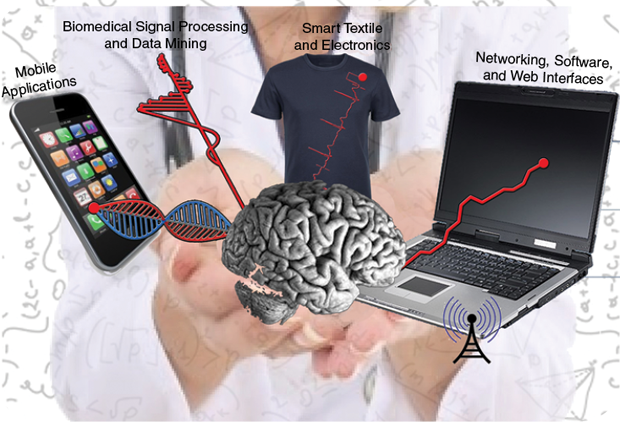
To overcome these clinical drawbacks, technology should be involved so as to play a crucial role in diagnoses and improvement of patients’ lifestyles. It is possible to use commonly available high-tech devices such as smartphones, personal computers, the Web, and social networks as viable tools for patient monitoring that provide feedback to clinicians and help achieve good affective balance.
A step toward this goal has been carried out through a research project funded by the European Commission: the Personalized Monitoring Systems for Care in Mental Health (PSYCHE) project [2]–[4]. PSYCHE identifies a personalized, pervasive, cost-effective, and multiparametric platform for the long-term acquisition of data gathered from patients affected by mental disorders. The mission of the project is to include a technological platform in mental health care, where a closed loop between clinicians and patients is implemented. Patients are monitored by means of sensorized clothes and can interact with user-friendly interfaces on smartphones to communicate with clinicians, who, in turn, can check the mental status of patients by means of professional Web-based interfaces.
PSYCHE considers a wide set of behavioral and physiological parameters that are continuously monitored through the smartphone and a sensorized t-shirt. More specifically, the sensorized t-shirt [developed by Smartex s.r.l, Pisa, Italy] is able to comfortably monitor cardiac activity by means of an electrocardiogram acquired by dry textile-based electrodes, the respiration activity by means of textile piezoresistive sensors, and physical activity using a triaxial accelerometer. A smartphone collects these data, sending them out to a remote data server. Moreover, the smartphone supports digital agendas, digitalized questionnaires, voice analysis, and scheduling of dedicated affective elicitation protocols. Accordingly, the main idea is that standard clinical practice is not modified, i.e., questionnaires and interviews continue to be used for diagnosis, but at the same time, an appropriate unobtrusive system continuously collects physiological and behavioral data to be further analyzed and used as support to the clinical diagnosis.
More specifically, a huge amount of data is preprocessed by embedded electronics and smartphones and sent daily to a centralized server for further advanced analyses. In particular, advanced signal processing algorithms are automatically launched on the remote server to effectively remove artifacts and extract significant features. Then, techniques of machine learning and data-mining are implemented to obtain an objective mental-state indicator (see Figure 1).
![FIGURE 1: The general architecture of the PSYCHE system. (Figure used with permission from [4].)](https://www.embs.org/wp-content/uploads/2014/05/34556.png)
Case Study
Bipolar disorder is a chronic mental illness in which patients experience episodes of altered mood states ranging from depression with sadness, hopelessness (including suicidal ideation), loss of energy, anhedonia, and psychomotor retardation, to mania characterized by euphoria or irritability, excessive energy, hyperactivity, hypertrophic self-esteem, reduction in the need of sleep, and psychomotor acceleration. The moderate form of mania is called hypomania (at this stage of mania, change in behavior is so obvious that hospitalization is needed). Accordingly, it is possible to identify four possible types of mood episodes associated with such a disease: depression (DP), mania or hypomania (HY), and mixed state (MS), which corresponds to the simultaneous presence of depression and mania, and euthymic state (ES) or remission, where patients experience periods of relatively good affective balance. A bipolar patient starts using the system while experiencing a depressive, manic or hypomanac, or mixed episode. Each patient is evaluated and monitored from the day of hospital admission toward remission, i.e., until reaching a euthymic, or normal, state.
Once enrolled, the core monitoring platform of the PSYCHE system (smartphone and sensorized t-shirt) is given to the patient, who is asked to wear the sensorized t-shirt at all times, also during the night. Therefore, while collecting data during this unstructured activity, there is no need of particular experimental conditions, as the patient is free to perform normal activities. However, the patient is also asked, but left free to refuse, to fill out the digitized mood agenda, answer specific questionnaires, and perform some emotionally driven tasks such as describing emotional-content pictures (e.g., the Thematic Apperception Test) or readings. Data from such a structured activity also comprise significant parameters and indices estimated from voice analysis. During the morning, the smartphone collects and sends all the physiological and behavioral data to the centralized server for further evaluation. The clinician, according to DSM IV criteria, decides the frequency of the clinical visits and assigns a mood label (DP, HY, MS, and ES). The mood label assigned to each patient evaluation is assigned independent of previous labels.
As mentioned above, once the centralized server receives new data, a feature space is built and associated with the respective mood label. After the definition of the training set, i.e., the first few acquisition sessions in which the patient experiences different mood states, the PSYCHE system is able to effectively serve as a decision support system for diagnosing the next mood state diagnosis. For each new acquisition, in fact, trends of significant physiological and behavioral variables, collected over time, are shown in the Web-based professional interface along with the result of the current mood state indicator. Such a classification result is provided as the probability associated with each mood state.
The PSYCHE system is currently under clinical validation through the enrollment of 20 psychiatric patients followed for 14 weeks. Preliminary results are very promising and encouraging for creating advanced technologies in treating mental disorders. Our studies also demonstrated that a single-variable approach, as usually proposed by previous studies, is not sufficient to robustly characterize mood episodes. Instead, a multiparametric and personalized approach (i.e., mood episodes are identified as an intrasubject analysis with ad hoc wearable monitoring systems) is much more effective.
From a purely speculative point of view, technology in mental health could go beyond the rigid application of DSM IV labels, but introduces the new concept that the clinical diagnosis is looking backward. Better understanding of the patient’s mood status can be achieved considering the dynamics of the disorder rather than the single observation treated as completely independent. For instance, patients with bipolar disorders present different clinical signs whether a depressive episode follows or precedes a manic status.
Studying mood swings over time demonstrates that changes in mental disorders have intrinsic dynamics that must be taken into account. This approach has been suggested also by clinical observations: it is widely accepted that clinical status differs over the course of bipolar illness. For instance, one can diagnose a depressive episode both in a patient that has just entered an episode and in one who is going to terminate the epsiode the next day. Although the rigid diagnostic criteria of the two episodes are equal, from a clinical point of view, they are very different.
All of this research points to a link between the ANS dynamics and bipolar disorders, i.e., links from the peripheral nervous system to a disorder of the central nervous system. In-depth psychophysiological reasons for such a link are still debated, although few hypotheses can be drawn. In particular, it is important to note that the ANS is indirectly affected by central nervous system activity: anxiety, fear, disgust, and the other primary emotions have both a central and peripheral correlates. For instance, the central activity of some brain structures such as the amygdala, anterior cingulate, hypothalamus, and ventromedial prefrontal cortex can directly affect ANS discharge through the modulation of sympathetic and vagal nuclei of the brain stem. We believe that since this modulation is present in healthy subjects, it is also present in an anomalous way in patients with mood disorders and dysfunctions of emotion expressions and regulations.
The impact of this research surely opens new opportunities to create a closed loop between patients and clinicians through continuous communication and feedback that facilitates disease management by fostering a new collaboration, with more autonomy and empowerment for the patient. We believe that constant monitoring of patients and feedback to physicians are the new keys to managing mental illness, helping patients, facilitating interaction between patient and physician, and alerting professionals in case of relapse and depressive or manic episodes, and, as an ultimate goal, identifying signal trends to predict critical events.
Technology in mental disorders, therefore, introduces the idea that mood disorders cannot be considered to be a series of independent and standalone states but rather a chronological sequence of mood states that are related to each other. Previous studies have not considered this issue, which may be one of the possible reasons for their failure to discriminate mood status at single-subject levels. Considering mood episodes as interlinked will possibly lead not only to a better characterization of the mood state and a better comprehension of psychophysiology of mood disorders but also to the possibility of predicting the clinical course of the disorder itself.
Acknowledgment
The PSYCHE system has been developed thanks to the collaboration of ten research and industrial partners among six European countries: the University of Pisa, Smartex s.r.l., Polytechnic University of Milan (Italy); Centre Suisse d’Electronique et de Microtechnique and the University of Geneva (Switzerland); Strasbourg University Hospital, INSERM U1114, the University of Strasbourg (France); Polytechnic University of Madrid (Spain); Maytec GmbH Informationssysteme (Germany); and Dublin City University (Ireland).
The research leading to the PSYCHE system received funding from the European Union Seventh Framework Programme under grant agreement 247777. Combining the efforts of both physicians and technicians, the system has been tested and focused on a specific kind of mental disorders, i.e., bipolar disorders.
REFERENCES
- H. U. Wittchen, F. Jacobi, J. Rehm, A. Gustavsson, M. Svensson, B. Jönsson, and H. C. Steinhausen, “The size and burden of mental disorders and other disorders of the brain in Europe 2010,” Eur. Neuropsychopharmacol., vol. 21, no. 9, pp. 655–679, 2011.
- G. Valenza, C. Gentili, A. Lanatà, and E. P. Scilingo, “Mood recognition in bipolar patients through the PSYCHE platform: Preliminary evaluations and perspectives,” Artif. Intell. Med., vol. 57, no. 1, pp. 49–58, 2013.
- G. Valenza and E. P. Scilingo, Autonomic Nervous System Dynamics for Mood and Emotional-state Recognition: Significant Advances in Data Acquisition, Signal Processing and Classification (Series in BioEngineering). Switzerland: Springer International, 2014, p. 162.
- G. Valenza, M. Nardelli, A. Lanata, C. Gentili, G. Bertschy, R. Paradiso, and E. P. Scilingo. Wearable monitoring for mood recognition in bipolar disorder based on history-dependent long-term heart rate variability analysis. IEEE J. Biomed. Health Inform., [Online].



