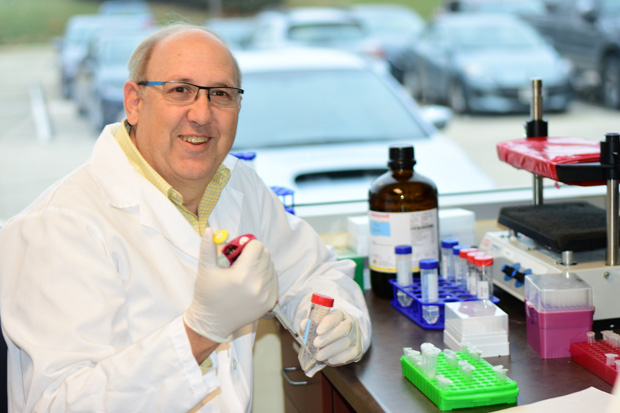
Only a few years ago, leading autism expert David Amaral described the disorder as a lifelong disability. Today, he acknowledges that description is no longer true. “Research lately shows that a substantial proportion of children with autism spectrum disorder (ASD)—something on the order of 30%—show really substantial improvements in their autism symptoms,” says Amaral, founding research director of the MIND Institute, an autism center at the University of California, Davis, CA (Figure 1). He adds that about 5% of the children, he and his colleagues, study at the MIND Institute actually lose their diagnosis over time.
Trained clinicians can diagnose autism by the time when a child is two years old, and provenbeneficial therapies can then start right away. Unfortunately, he points out, the average age of autism diagnosis in the United States is 4.3 years. The late diagnosis is due in large part to a lack of trained personnel to conduct the qualitative assessment and properly evaluate children, including those who have milder forms of ASD. “That’s a problem because we know that the sooner you start therapy, the better the child will do. If we don’t get a diagnosis until after four years of age, and then parents find that it can take another six months to a year to get a behavior therapist lined up, that means that you’ve lost a valuable 2- to 3-year window of opportunity for treating the child,” he remarks. The key to good results is catching ASD early, Amaral asserts.

Part of the solution may be a new and quantitative strategy to diagnose autism [1]. Amaral is working with a company to develop an assay for biomarkers associated with certain subtypes of ASD (Figure 2). Stemina Biomarker Discovery of Madison, WI, and its diagnostic division NeuroPointDX recently released results showing that it had identified an alteration in amino acid metabolism in nearly one in five children with autism, and had developed a tool to detect it.
Stemina originally approached Amaral in 2011 with the idea of collaborating on a metabolomics study to identify the different subtypes of ASD. Amaral thought it was a great idea. “We had realized at the institute that trying to understand autism without understanding the subtypes would be like trying to understand cancer without specifically going after lung cancer, breast cancer, or other cancers, because there might be different causes and treatments,” he says. In fact, the MIND Institute had already begun work to define the subtypes through its Autism Phenome Project and had dabbled in a metabolomics strategy in the early 2000s.
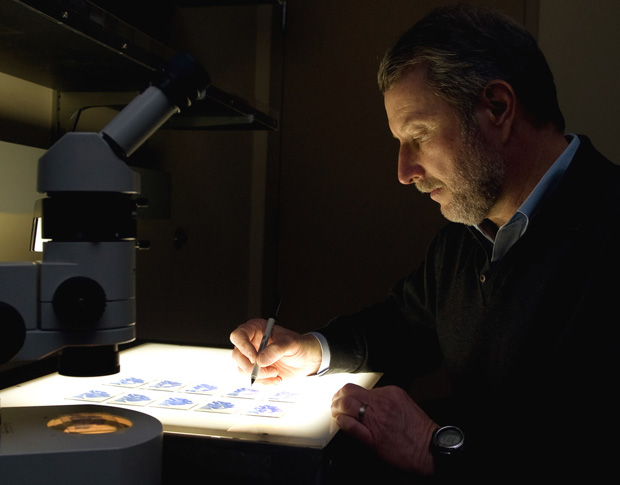
The first phase involved an initial test of Stemina’s metabolomics platform. Amaral provided a small collection of banked blood samples from a previous study, and Stemina ran them through its algorithms and analyses to determine whether it could distinguish a child with autism from a typically developing child [2], according to Robert Burrier, PhD, chief operations officer and vice president of research and development at the company (Figure 3). The platform was able to find an autism signature, but it was not a clear-cut yes or no, because autism is such a broad disorder, he says. “It was clear that the question should be whether we can identify children who share the same subtype of autism—we now call the subtypes metabotypes—so we can understand more about the diagnosis of children and what their potential therapeutic strategies might be.”
That led to a much larger study, called the Children with Autism Metabolome Project (CAMP). For this project, the MIND Institute and seven other clinical sites around the country collected samples from 1100 children aged 18 months to 4 years old, including about two-thirds of who had been formally diagnosed with ASD by research-reliable psychologists. The researchers specifically looked for altered metabolism of branched-chain amino acids, which previous research had suggested might lead to some autism-like symptoms, Amaral explains. “We wanted to know whether we would see any indication of these alterations in kids with autism, and in the end, that is what we found.” Of the samples in the CAMP study, 16.7% of children had the altered metabolism of branched-chain amino acids.
“The fact that we found 17% is pretty phenomenal on the one hand, but this is just step one,” Amaral reports. “We are continuing analysis of the samples that we’ve collected to look for other perturbations, and we already have findings related to other amino acid changes, which brings the test up to about 30% detectability.”
Stemina, through its diagnostic division NeuroPointDX, began offering the diagnostic test (NPDXAA) commercially on 1 November 2018. “We are doing a rolling, limited launch because we want to make sure that if we’re going to get a blood sample from a child, it’s done right,” Burrier says. Once the sample is taken, the blood-draw tube is packaged in dry ice and sent to Neuro- PointDX for analysis. Currently, about a dozen sites around the United States have demonstrated they can draw the samples and prepare them to be sent to NeuroPointDX, he says, and additional sites “are being added all the time.” He remarks, “Our test is highly quantitative for all 32 of the amines that we measure, and that allows us to set very precise thresholds and therefore provide a highly predictive test to the market.”
This test is part of a much more far-reaching strategy, Amaral notes. “We see this as one component of what will ultimately be a whole series of biomarkers that could be evaluated all at the same time to see whether a child has one of these metabotypes.” The test would not only provide diagnostic confirmation but would also detect metabotypes in siblings, who have a heightened risk for ASD.
Even more importantly, Amaral contends, metabolomics will suggest possible innovative routes for therapy that could improve the quality of life for people with autism. He adds, “In the fullness of time—and it will probably take us several years—we hope to have additional metabotypes that will bring the number higher, possibly to 50%, 60%, even 70% of kids with autism. That would be amazing.”
References
- P. R. West et al., “Metabolomics as a tool for discovery of biomarkers of autism spectrum disorder in the blood plasma of children,” PLoS One, vol. 9, no. 11, p. e112445, Nov. 2014.
- A. M. Smith et al., “Amino acid dysregulation metabotypes: Potential biomarkers for diagnosis and individualized treatment for subtypes of autism spectrum disorder,” Biol. Psychol., vol., 85, no. 4, pp. 345–354, 2019.



