Advancements in ablation techniques have paved the way for developing safer and more effective medical devices for treating various cardiac maladies such as atrial fibrillation. However, the inability to monitor treatment outcome-dependent features, such as tissue temperature and lesion formation, poses an unmet clinical need. This study aims to (a) develop a novel theranostic endoscopic system and (b) evaluate its ability to monitor the thermal lesion formation and tissue thermometry during ablation procedures. A novel theranostic endoscopic system was developed by retrofitting a traditional intracardiac echocardiography (ICE) catheter with laser ablation and photoacoustic (PA) imaging capabilities. Laser ablation provides distinct advantages over radiofrequency ablation because of its well-controlled heating, which protects against vascular damage and charring of the endothelium. It also allows for well-demarcated and homogenous lesion formation. Laser ablation was incorporated into the endoscope through an optical fiber coupled to a continuous wave laser ablation system. The dependence of the PA signal on the ambient temperature variations enables the endoscope to provide real-time non-invasive tissue thermometry. Moreover, the differences in wavelength-dependent absorption properties of ablated and non-ablated tissue allow PA imaging to identify the location of the thermal lesion. The endoscope was made PA-compatible by adding six pulsed laser-coupled optical fibers. The theranostic features were evaluated by analyzing its ability to monitor tissue temperature and lesion formation during the murine myocardial tissue ablation and distinguish between tissue types during pre- and post-ablation, confirmed by tissue staining. The tissue sample was successfully ablated over a targeted 16 mm2 area. By quantifying the deoxyhemoglobin spectra between λ = 740-760 nm, the ablated tissue was distinguished from the surrounding non-ablated tissue. Lastly, the variation of PA amplitude measured during ablation highlighted the tissue’s temperature. In summary, the developed theranostic device can potentially improve the safety and efficacy of laser ablation procedures.
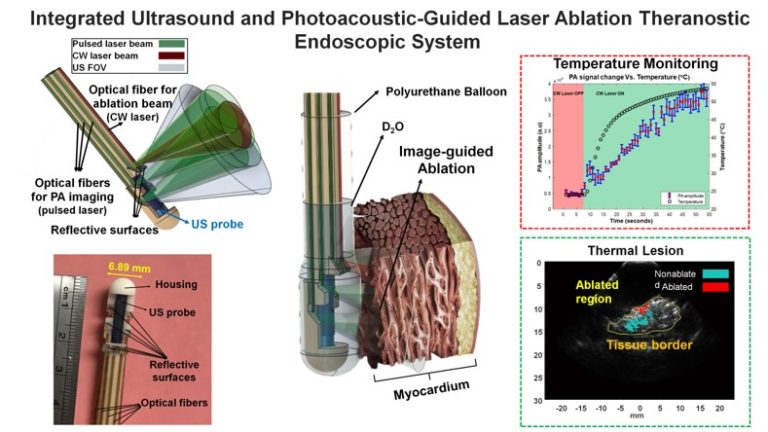
Integrated Ultrasound and Photoacoustic-guided Laser Ablation Theranostic Endoscopic System
Sign-in or become an IEEE member to discover the full contents of the paper.