Virtual, augmented, and mixed reality environments are increasingly being developed and used to address functional rehabilitation goals related to physical, cognitive, social, and psychological impairments. For example, a child with an acquired brain injury may participate in virtual rehabilitation to address impairments in balance, attention, turn taking, and engagement in therapy. The trend toward virtual rehabilitation first gained momentum with the adoption of commercial off-the-shelf active video gaming consoles (e.g., Nintendo Wii and XBox). Now, we are seeing the rapid emergence of customized rehabilitation-specific systems that integrate technological advances in virtual reality, visual effects, motion tracking, physiological monitoring, and robotics.
The main draw of virtual rehabilitation is the capacity it allows clinicians to control the characteristics of the virtual environment while modifying the degree of challenge to suit individual patient needs. For example, by reducing the number and speed of visual stimuli, removing visual clutter and auditory feedback, and directing stimuli to one side of the body only, therapists can enable a child with a brain injury to participate in virtual reality in a way that optimizes success and recovery. Augmented feedback (e.g., visual, auditory, and haptic) and opportunities for motivating repetitive practice make this approach particularly appealing for motorlearning applications [1]. Stroke patients and patients with brain injury, orthopaedic and musculoskeletal injuries, cerebral palsy, and other neurodevelopmental diagnoses are the most frequently reported clinical populations receiving virtual rehabilitation by occupational and physical therapists in Canada [2]. In pediatrics, cerebral palsy, stroke, brain injury, autism spectrum disorder, and chronic pain populations are among the top five [2]. However, as a developing field, additional work is needed to gather information about usage habits in other countries and by other professions involved in rehabilitation.
Barriers and Facilitators of Clinical Adoption
Despite their advantages, challenges exist in implementing virtual rehabilitation technologies into clinical practice. A recent national survey in Canada identified the most significant barriers as lack of time, funding, treatment space, appropriate patients, and support staff [2]. Low self-efficacy in using the technologies (with respect both to their technical operation and to applying them clinically in a way that optimizes patient outcomes) is also reported as a consistent barrier in implementation studies [3]. Encouragingly, clinicians report a strong interest in learning how to integrate these new treatment approaches into practice.
Additional barriers (and facilitators) include the following:
- the characteristics of the technology itself (e.g., the ability to modify software parameters to adjust the patients’ degree of challenge)
- the awareness of, access to, and quality of research-based evidence supporting its use
- a personal interest in using it
- competing treatment approaches and technologies
- the extent to which the features of the technology match or address patient needs and goals
- peer influence
- client motivation
- the environmental and resource contexts in which the technology is being implemented [3].
For example, housing the technology in multiuse spaces restricts access for patients during nonclinical room bookings. Virtual rehabilitation treatment spaces must also be in close proximity to typical treatment areas to make their use feasible for clinicians, and technical support must be readily available to support clinicians in the technology’s use. Figure 1 summarizes these factors, along with the pediatric considerations and support strategies discussed in the following section.
Specific Considerations in Pediatrics
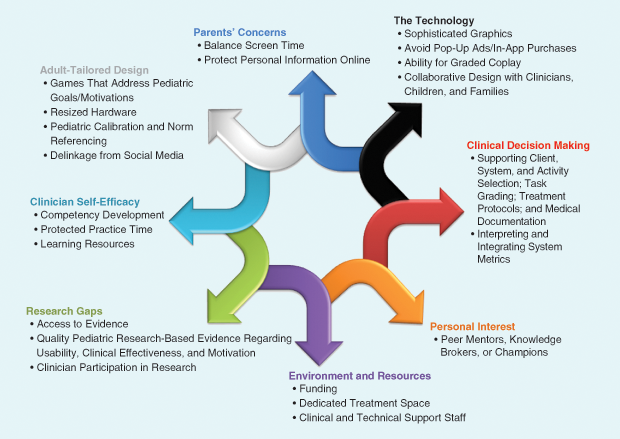
Additional considerations increase the complexity of virtual rehabilitation technology design and implementation in pediatrics. The majority of these technologies are developed for adult populations, which limits the range of systems and activities available or appropriate for pediatric therapy. The nature of the tasks (e.g., sorting recyclables or laundry) may not be as engaging to children or match their personal goals, while calibrations or norm-referenced metrics embedded within evaluation algorithms are often established using adult populations, decreasing their validity for children and adolescents. The hardware, such as virtual reality headsets, haptic gloves, and robotic devices, are also typically designed to fit adults. The industry may not find it immediately cost-effective to adapt these features for the pediatric market.
In addition, parents may be hesitant to consent to therapy that increases their children’s screen time. They may also have concerns related to the privacy of their children’s health or personal information, particularly when the data are not stored locally but sent to external servers managed by industry developers. When using web-based commercial applications, pop-up ads and in-app purchases introduce distractions and potential liabilities, especially for those with cognitive impairments. Some such applications may not even be accessible to preadolescent children. For example, those integrated with social media platforms to provide opportunities for social engagement often require users to meet a minimum age threshold (e.g., 13 years).
Family and peer involvement in therapy sessions is a strategy used often with children to support motivation, recovery, and community reintegration. Virtual rehabilitation systems that allow multiple concurrent users (e.g., a therapist or family member) and remote users (e.g., siblings connecting from a rural community) as well as social interaction, cooperation, or competition are less prominent in the rehabilitation market than in mainstream markets. Equally problematic is that most systems do not adequately compensate for the level of cognitive and physical challenge faced by children undergoing therapy to enable them to participate on a level playing field with peers during tandem play. As a result, a child with a limited range of motion may not be successful in playing or competing alongside a friend or parent who does not have such an impairment, which can decrease the child’s willingness to participate. Finally, fewer scientific studies on usability, clinical effectiveness, and motivation have been conducted with pediatric participants, leaving evidence-informed applications of these technologies more challenging for pediatric clinicians.
In our digital age, children’s interaction with computers is commonplace. Young people have grown up exposed to the latest technological developments in functionality, visual appeal, and interactivity. In this context, children and adolescents used to the sophisticated graphics and visual effects afforded by mainstream recreational gaming programs may be put off by the more limited capabilities provided by current commercialized virtual rehabilitation technologies. As collaboration in the virtual reality and rehabilitation fields improves and access to more ecologically valid and technologically advanced virtual environments becomes more cost effective, the rehabilitation field will benefit from more motivating systems with greater therapeutic utility.
Support Strategies
The implementation of virtual rehabilitation technology requires support for clinicians as they learn how to optimize applications to benefit these patients. In addition to competency development through interactive and online continuing education, clinicians new to the approach require resources to guide their clinical decision making about system and activity selection, task grading, and medical documentation [3]. They require support for interpreting and integrating system-embedded evaluation metrics (e.g., the center of pressure values during a balance task) into their existing clinical evaluation processes, as well as time to practice using these new treatment tools outside of patient appointments [3].
Technical troubleshooting, dedicated treatment space, and supervisor support are also necessary facilitators [3]. The identification of peer mentors, knowledge brokers, or champions may also support competency development, access to evidence, and adoption; moreover, user participation in research not only ensures its clinical relevance but also facilitates future implementation efforts [3].
Future Directions
Collaboration among technology developers, researchers, health professionals, patients, and families is required to design, refine, evaluate, and implement compelling rehabilitation-specific systems that meet the physical, cognitive, and psychosocial needs of both adult and pediatric patient populations as well as the health professionals delivering the treatment. Gaining insights into how user experience is influenced by the characteristics of virtual environments, first- or third-person perspectives, avatar embodiment, augmented feedback, and/or immersion will require more research to assess rehabilitation outcomes in relation to these features across populations and treatment goals. Research is also required to examine the effectiveness of targeted strategies to support technology adoption in clinical sectors. This work will facilitate more streamlined implementation of these technologies and augment their impact on functional improvement in patients across the health system.
References
- P. L. Weiss, H. Sveistrup, D. Rand, and R. Kizony, “Video capture virtual reality: A decade of rehabilitation assessment and intervention,” Phys. Therapy Rev., vol. 14, no. 5, pp. 307–321, 2009.
- D. L. Levac, S. M. N. Glegg, P. Miller, and H. Colquhoun, “Virtual reality and active video game-based practice, learning needs, and preferences: A cross-Canada survey of physiotherapists and occupational therapists,” Games for Health, vol. 4, no. 4, pp. 217–228, 2017.
- S. M. N. Glegg and D. L. Levac, “Enhancing clinical implementation of virtual reality: An evidence-based perspective and call to action,” presented at the Int. Conf. Virtual Rehabilitation, Montreal, QC, June 2017.


