Slip on a set virtual reality (VR) goggles and connected gloves, and you are transported to another world. For the entertainment industry, that kind of immersive VR may mean shoot-‘em-up games where players have to blast blood-thirsty aliens or other bad guys to save the day. For the military, it may be simulations for pilot instruction or soldier training. And for a growing number of researchers— and now companies—the focus is on using VR systems to help patients deal with pain.
VR for Acute Pain

Numerous research studies have already shown that VR can alleviate pain. One that drew considerable attention tested whether the distraction of immersive VR had benefits over that of watching television to take a patient’s mind off the pain. It did [1]. The study, which included 120 patients who were experiencing moderate to severe pain due to medical or surgical conditions, showed a 52% reduction in pain in the group watching VR compared to the group that watched the same type of content on the TV screen, said David Rhew, MD, chief medical officer with Samsung Electronics America (Figure 1).
“What that means is that it wasn’t the content that was having the direct impact on the pain, but it was something to do with the immersiveness of VR that was dramatically impacting their pain scores,” he said. “And the more remarkable thing was that even after the individuals took off the VR headsets, they had sustained pain relief for 1–2 hours and sometimes even longer, so it had almost a therapeutic impact on these individuals that we had not anticipated.”
The results of these and other research [2], [3] suggest that immersive VR could potentially be used to reduce the need for pain medications, notably opioids, according to Rhew. As a result, Samsung is now actively involved with Cedars-Sinai and the American Hospital Association to explore how VR and possibly other technological tools can be used to address the opioid epidemic. In particular, he said, they are looking into VR as a potential alternative to opiates for postsurgical pain. “What if a patient used virtual reality as a first-line treatment to try to manage their pain and only used the opiate for breakthrough pain?” Reducing the reliance on pain medications would be a step forward, he said, because among individuals who begin taking an opiate in a hospital, about 6% are still taking an opiate 30 days later. He remarked, “We are very concerned that we are starting people down this path, but (at this point) we don’t have the options up front. VR could allow us to do that.”
In addition, there’s a potential to substitute VR for at least some of the pain medications that are currently used to treat chronic pain, Rhew said. That will involve resolving such questions as how to design it for optimum benefit, how to educate patients to use it on their own and outside the clinic, and how to pay for it. “Those are the kinds of things we need to figure out, and this is why we are working closely with other organizations on the healthcare provider side and the patient side, so we can understand what needs to be done.”
Ice to the Fire

Some pain-directed VR products are already being used. One of the best-known is SnowWorld, an immersive VR experience designed to lessen the agony experienced by burn patients during their treatments. Created more than two decades ago, the idea grew from a discussion between Hunter Hoffman (Figure 2), Ph.D., who was beginning to design early VR applications as a member of the University of Washington’s Human Interface Technology (HIT) Lab [4], and doctoral student John Everett, who was doing his dissertation on psychological techniques to reduce pain in burn patients at Harborview Burn Center in Seattle (with NIH-funded academic advisor Prof. David Patterson). “When John told me that distraction was one technique they used with burn patients, I said, oh my gosh, this virtual reality is extremely distracting!” Hoffman and Patterson put their heads together with virtual-world builders at MultiGen-Paradigm of San Jose, California, and came out with the first iteration of SnowWorld in 1999. It has undergone numerous improvements over the years, and has now graduated to commercial development, with the latest version built by Firsthand Technology, Seattle, WA, and designed specifically for clinical pain relief.
Hoffman and his research group are also now joining forces with another company, BigEnvironments of BigEnvironments of Seattle, WA, to develop a separate burn-pain VR system, called SnowCanyon, which is designed for the HTC VIVE headset. Both SnowWorld and SnowCanyon are based on the same approach: using VR to take the brain’s attention away from the excruciating pain of wound-cleaning and skin-stretching that are part of burn treatments (Figure 3). Once a patient dons the VR headsets, he or she enters a world of ice and snow that is detached from the sights and sounds of the real world and the treatment. “So instead of your visual cortex giving you the same information as your pain receptors, you now have a competition between what you’re seeing in the virtual world and the information coming in from the pain receptors,” Hoffman said. “It’s basically distraction on steroids.”

In creating what Hoffman called “the first immersive VR pain-managing system,” Hoffman and Patterson talked with patients and clinicians to find solutions that made sense to both. Patients, for instance, needed to go to a calm place that was “the opposite of fire,” Hoffman said, and that would encourage engagement and interactivity and a strong illusion of “being there” in the computer-generated world. Clinicians, however, needed the patients to stay relatively still, such as during staple removal [5], [6]. In the end, the researchers settled on a no-stress game set in an icy mountain setting, where patients earn points by simply pushing a button to throw snowballs at snowmen, penguins, and other nonmenacing targets. “While the patient can look all the way around if he wants, we put most of the interesting stuff straight ahead, so that minimized their head movements too,” he explained.
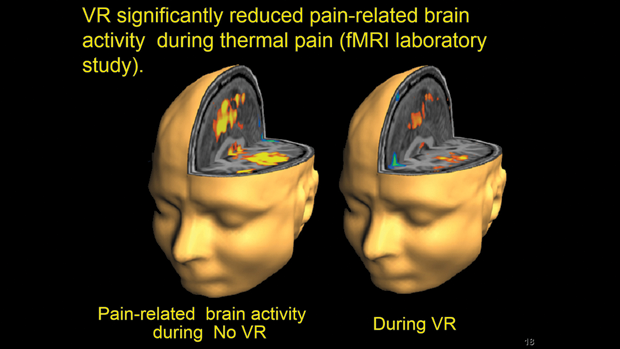
Another consideration in developing VR for these patients was to make the headsets compatible with the treatments, such as the water baths where treatment often takes place. For that, Hoffman worked with HIT Lab colleague Eric Seibel and instrument makers in UW’s Human Photonics Lab [7] to create a fiberoptic image-delivery system (Figure 4). “We built a pair of water-friendly virtual reality goggles that bring the images to the patients in the form of photons instead of electrons, so they can sit in water and use them,” Hoffman said. The nonferrous goggles are also suitable for use in a functional magnetic resonance imaging (fMRI) scanner, which the researchers have used to test VR’s pain-relieving capabilities (Figure 5). Those tests have shown an average 25%–50% reduction in pain-related brain activity, and demonstrated that immersive VR was comparable to a moderate hydromorphone dose (4 ng/mL target plasma level) for reducing acute pain [8], [9].

Currently, SnowWorld and SnowCanyon are both being tested and used on burn patients in about a dozen hospital settings, including one that’s under way with Walter Meyer III, MD, Shriners’ director of psychology and psychiatry services at Shriners Hospitals for Children, Galveston, TX, burn center that treats children with large burns (Figure 6). “Wound care for these children means pain that’s just off the scale compared to almost any other medical procedure in the world, so we’re bringing out the big guns to try to distract these kids during their wound cleaning, and also looking at using VR for longer treatments for these bigger burns and (determining) whether it continues to work time after time,” Hoffman said.

VR is showing great promise, but it still has a way to go, he remarked. “This is really the soldier science phase of iterative improvements. I think we’re in the transition phase with burn patients—between research and standard of care—so our goal is to get to the point where the patients are using virtual reality even if they’re not in research.” And once it does become a standard of care, Hoffman added, there will always be room for improvement. “We can’t call it a win and walk away, because there are a lot of emerging technologies and products that can potentially be brought into the treatment. It’s really a moving target.”
VR for Chronic Pain

Besides furthering the development of Snow- World, Firsthand Technology has been working on additional VR applications, including one called GLOW!, which is geared primarily toward alleviating chronic pain, and promoting relaxation and mindfulness, according to CEO Howard Rose (Figures 7, right, and 8, below).
Part of coping with chronic pain is learning ways to ease it, and GLOW! uses a heart-rate monitor to help teach patients how to take control of their respiration, which can lower anxiety levels and improve therapeutic success, Rose said. “In GLOW!, you are in an evening glade surrounded by dancing fireflies. GLOW! uses a camera-based system so the patient interacts using their physical hands manifested in the virtual world” (Figure 9). He described it as a biofeedback experience that uses a heart-rate sensor to drive a simple meditative action: “Lower your heart rate and close your fingers to call the fireflies to you. The fireflies become liquid light in your hands, which inspires active play and physical motion. Lanterns appear and you can put the light into the lantern, then watch the glowing lanterns fly off into the sky.” Patients experience a reduction in pain and develop mindfulness skills to control their pain better, he added, and “doctors report that GLOW! is actually helping chronic pain patients stop using opioids.”


In addition, GLOW! emboldens the patient to move, something that typically is helpful for long-term recovery from a chronic condition, but that patients may avoid because they fear it might trigger pain, Rose said. “When people are immersed in VR, they are totally present and focused. This helps free them from the self-limiting fear of moving and enables them to relax and recover faster.”
Currently, Rose estimates that Firsthand’s VR software is helping patients in more than 40 chronic pain clinics and hospitals in North America and Europe, and Firsthand is building on clinical success to scale up its VR products and spread them to more clinics. “Many physicians today have heard of VR pain relief and know Firsthand’s role in developing this therapy. They are interested and receptive, but most still have never personally tried VR, and they come to us to learn more about how to bring it to their clinics. Interest is definitely growing, and we’re looking forward to hitting the tipping point where VR becomes ubiquitously accepted and integrated into pain medicine everywhere.”
Up and Coming
Firsthand is now also looking into more ergonomic headsets as well as VR systems that can work on ever-smaller computers, or that can be wirelessly streamed from the cloud. “In the future, biosensors and biometrics will become increasingly important and integrated into VR hardware systems, driven by artificial intelligence to dynamically modulate the VR environment so it is personalized to the individual patient,” Rose said.
Similarly, Samsung is collaborating with software developers to take into consideration biometrics, particularly capturing respiration measurements and using VR content to help the patient adjust their breathing to a level that enhances pain management, Rhew said. They are also studying whether newer sensors can track pain-related physiologic parameters, such as increases in blood pressure that are generally associated with heightening pain, and ultimately help clinicians and patients assess both when VR should be employed and how well it is working. “We need more of these non-narcotic tools and alternatives for individuals to be able to better manage their care and specifically their pain.”
VR doesn’t just have potential applications for pain. Hoffman and Rose have been involved in developing VR systems for exposure therapy designed to help people recover from post-traumatic stress disorder. Hoffman is also part of a group developing a system to engage people who have spinal cord injury and paralysis, and is collaborating with Barbara Atzori from the Department of Health Sciences at the University of Florence, Italy, and Wadee Alhalabi from the Departments of Computer Science at King Abdulaziz University and Effat University in Jeddah, Saudi Arabia, to use VR to ease pain during blood draws. In addition, Samsung and IrisVision, Pleasanton, CA, have developed a VR low-vision system to improve vision for patients with macular degeneration. Other research teams are designing systems that assist children who have autism spectrum disorder or attention deficit disorders, that provide surgical or other training, and that help in a variety of other health-related situations.
Hoffman remarked, “Everybody is scrambling to use virtual reality on different medical procedures in a wide range of patient populations. It’s really catching on.”
References
- V. C. Tashjian et al., “Virtual reality for management of pain in hospitalized patients: Results of a controlled trial,” JMIR Mental Health, vol. 4, no. 1, Mar. 2017, p. e9, 11 pages.
- T. McSherry et al., “Randomized, crossover study of immersive virtual reality to decrease opioid use during painful wound care procedures in adults,” J. Burn Care Res., vol. 39, no. 2, Feb. 2018, pp. 278–285.
- K. M. Malloy and L. S. Milling, “The effectiveness of virtual reality distraction for pain reduction: A systematic review,” Clin. Psychol. Rev., vol. 30, no. 8, Dec. 2010, pp. 1011–1018.
- Human Interface Technology Laboratory, University of Washington, Seattle, WA, USA. [Online]. Available: www.hitl.washington.edu
- H. G. Hoffman, J. N. Doctor, D. R. Patterson, G. J. Carrougher, and T. A. Furness, III, “Use of virtual reality for adjunctive treatment of adolescent burn pain during wound care: A case report,” Pain, vol. 85, no. 1–2, Mar. 2000, pp. 305–309.
- H. G. Hoffman, “Virtual-reality therapy,” Sci. Amer., vol. 291, no. 2, Aug. 2004, pp. 58–65.
- Human Photonics Lab, University of Washington Mechanical Engineering, Seattle, WA, USA. [Online].
- H. G. Hoffman et al., “Modulation of thermal pain-related brain activity with virtual reality: Evidence from fMRI,” NeuroReport, vol. 15, no. 8, Jun. 2004, pp. 1245–1248.
- H. G. Hoffman et al., “The analgesic effects of opioids and immersive virtual reality distraction: Evidence from subjective and functional brain imaging assessments,” Anesth. Analg., vol. 105, no. 6, Dec. 2007, pp. 1776–1783.



