In mid-March 2020, as the novel coronavirus started making its way through the United States, Fiona Lowenstein (they/their) became ill. At that point, there was not yet any public health guidance on social distancing and wearing masks, and certainly no routine or readily accessible testing for COVID-19. Lowenstein was still interacting with others in person, and even led a yoga class. But when they became sick and were hospitalized, they were tested for SARS-CoV2 and received a positive diagnosis.
Lowenstein, a journalist and founder of the queer-femme wellness collective, Body Politic, immediately took to social media to raise awareness of the virus. Soon, their Instagram was flooded with messages from other survivors. Lowenstein texted frequently with Body Politic’s cofounder, Sabrina Bleich, who also tested positive, in order to keep track of each other’s symptoms. “We were experiencing symptoms that the Centers for Disease Control was not listing at that point,” said Lowenstein. Soon, Lowenstein recognized that there was already a platform where COVID-19 survivors could connect: Body Politic. “I realized I could not keep communicating with each of these people individually,” Lowenstein said. “It was exhausting. We had the infrastructure [with Body Politic] to launch,” and through that platform, “these strangers could be helping each other.”
Since the spring, a number of online communities—Body Politic, Survivor Corp, Long COVID Support Group, LongCovidSOS, among others—have taken root as COVID-19 survivors try and make sense of the bizarre symptoms that they are experiencing. Statistically speaking, since only about 1.5% of individuals who get the novel coronavirus will die, millions of individuals (self-described as “long haulers”) will survive and may suffer from post-COVID syndrome. While some symptoms are somewhat more common, including increased heart rate, the swelling of extremities such as toes, or chronic fatigue, much else remains unknown, and the list of possible complications grow by the day. In addition, people who were mostly asymptomatic may be experiencing different long-term effects from those who had to be hospitalized. Ultimately, these digital communities are on the frontlines of patients documenting new symptoms and are able to provide valuable data on what the full range of symptoms can be for someone recovering from COVID-19.
“We see things because we are getting real patient accounts in real time,” says Diana Berrent, the founder of Survivor Corp, a Facebook group for COVID-19 survivors. “By the time one doctor sees enough cases, they’d have to do a study”—which takes time in reporting findings. “But we can say: we’re seeing trends here, and this is alarming.”
Creating community
When Body Politic pivoted to becoming a community for long haulers, Lowenstein created a Slack group. Every COVID survivor who wants to join fills out a short survey before they are admitted to the private group. Within the Slack group, there are dozens of channels. There are channels based on symptoms specific to a part of the body, channels for people who have been sick for more than 30, 60, or 90 days. “All the channels are based on user requests,” says Lowenstein, “so they morph over time.”
Users in the group would frequently post, asking if they were alone in the symptoms they were experiencing. Many of the symptoms early on, Lowenstein said, weren’t yet being recorded by the Centers for Disease Control (CDC). Shortly after the initiation of the Slack group, Lowenstein received a message from Gina Assaf, a designer and researcher in the group, who wanted to start surveying group members’ symptoms.
Assaf’s initiative started as a channel in the Slack group, and has since evolved into what’s called Patient Led Research for COVID-19, a self-organized group of COVID survivors who are collecting data on long haulers. In May, she and her colleagues published a report about long-COVID symptoms over the course of two months after infection, based on 640 surveys from patients. At the two-month point after acute infection of SARS-CoV2, the majority of respondents said they had not yet recovered. Many reported that while they had recovered from a fever, they were suffering from fatigue, had trouble sleeping or concentrating, and lost their appetite.
Patient Led Research is now working on a longer, more intensive report to survey what long COVID looks like seven months out, according to Hannah Davis, a researcher with the group. “There are some symptoms that are pretty persistent, but there are others that show up for three of four days and then never show up again,” she says. “Those of us who have been sick for six or seven months absolutely have dealt with a hundred symptoms over the course of the past seven months.” This seven-month survey would take more than an hour to complete, Davis says. The group is aiming to survey about 4000 COVID survivors worldwide.
Tracking symptoms
Most long-COVID patients are not using anything technologically advanced to track their symptoms, but more frequently opting for a diary or a spreadsheet. They then transfer their logs to answer surveys like the one initiated by Patient Led Research. While there aren’t currently many phone apps currently available specifically for long haulers, some are in development. Ultimately, the best symptom tracking apps will take into consideration the needs of the patients and might actually help them—for instance, if a patient logs three symptoms that might require medical attention, an app might tell them that they need to visit a doctor.
“COVID survivors are the experts on the disease,” says Natalie Lambert, of Indiana University’s School of Medicine. “We need to make apps from input for a lot of survivors so they know it works for them.”
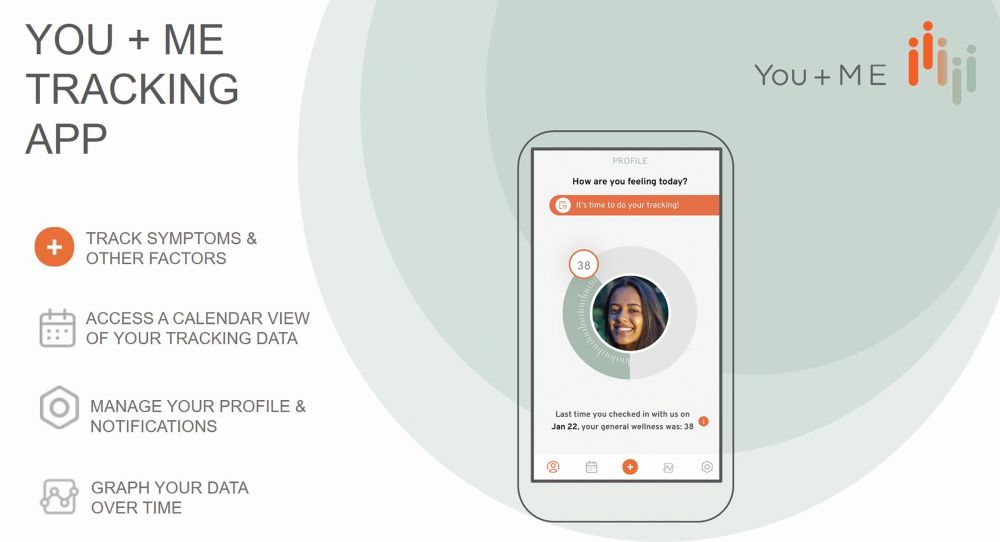
One phone app, called YOU+ME (Figure 1), is developed by Solve M.E., a nonprofit disease organization that supports research for myalgic encephalomyelitis (ME). ME, otherwise known as chronic fatigue syndrome (CFS), is a complex chronic disease with no diagnostic test nor Food and Drug Administration (FDA)-approved treatment.
Similar to COVID survivors, ME/CFS patients have a range of symptoms, explains Allison Ramiller, Solve M.E.’s director of research programs. “The disease can vary a lot between people, but also vary quite a lot over time,” she explains. “Capturing a moving picture of the illness and getting that longitudinal data is an incredibly valuable piece of information.” In the spring of 2019, Ramiller and her colleagues recognized that the app also could be repurposed for tracking COVID survivors’ symptoms.
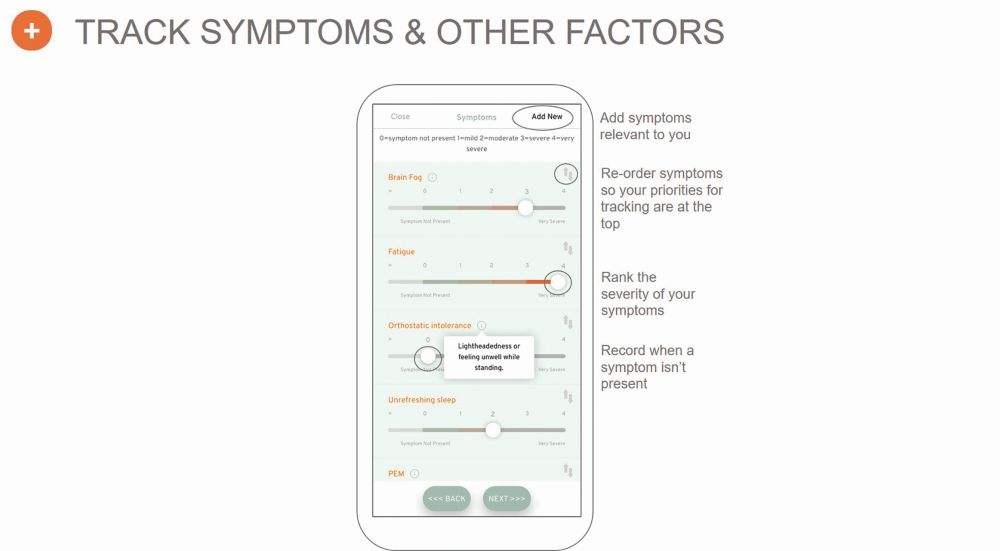
Once registered on the app, users can set their own custom notification schedule to be reminded daily or weekly to fill out a short survey on their symptoms (Figure 2). “We don’t require that people do it daily or require that they’re reminded daily, because [we acknowledge] that people have limited energy and ability to engage in an activity that could deplete their energy reserve,” Ramiller says.
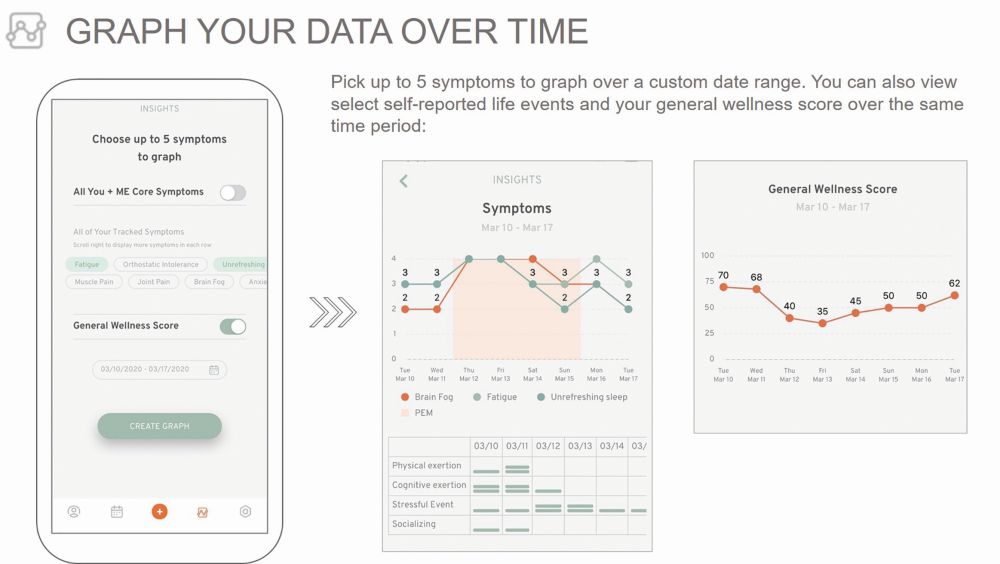
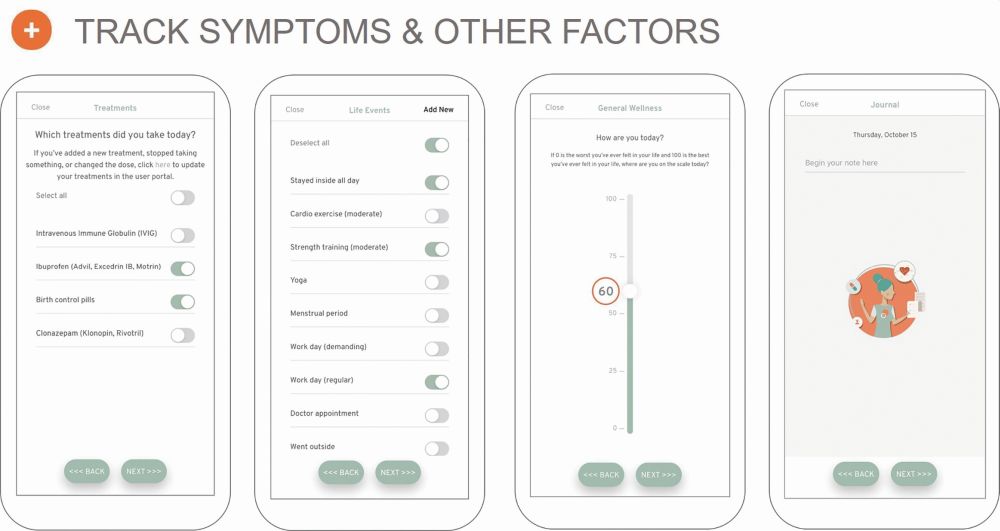
The symptoms captured on the app come from those reported by survivors on Body Politic or Survivor Corp, and those groups’ respective surveys (Figure 3). On the app, users can answer questions that takes anywhere from 3 to 10 minutes, says Ramiller. They are asked to rate the severity of their symptoms, and add their own symptoms if they are not currently listed as an option. Users can also list life events that might have been relevant to their day—for instance, whether or not they went outside, or socialized with friends or family (Figure 4). Users can also “journal” within the app using the voice-to-text function, to dictate how they are feeling in a given day beyond just reporting their symptoms.
The users’ data is secured and YOU+ME is currently building out a portal for research opportunities. Scientists who apply for access can view deidentified data, for instance, to build cohorts for future research. Users who consent to using the app also consent to be contacted, so a researcher could conceivably look at women who are under 45 who experienced a very specific symptom for future research, explains Ramiller. “Our intention is to make the data as accessible and useful for research as possible and not have it be siloed,” says Ramiller. “We want it to be maximally beneficial for as many projects as possible and want to encourage more citizen science projects—you don’t have to have an academic affiliation to access the data.”
Currently, the app is in beta testing, and is soliciting feedback from a couple hundred COVID survivors.
Regardless how symptoms get tracked, the medical community and the public would benefit from a better understanding of what it means to survive COVID-19. “The most pressing objective right now is that there needs to be an understanding that long haulers are ultimately a very diverse group,” says Lowenstein. Some long-haulers may test positive for the virus; others may not have access to testing; some get antibodies while others never sero-convert. “Even the idea that some are young and otherwise healthy—that’s not the case with all of them,” Lowenstein adds. There’s a wide spectrum among the individuals who get hospitalized, or the ones who are largely asymptomatic. Continued research and patient reports in online communities will help write the long-COVID playbook.
Others also hope that the attention on COVID survivors as folks living with a chronic illness will bring to light the importance of studying other chronic diseases. “I see this as a new type of new health revolution,” says Lambert. Not only are researchers focusing on the patient experience, but Lambert hopes that the research on long-COVID also helps people who suffer from other chronic diseases. “A lot of illnesses get put in the chronic bucket, but there aren’t a lot of answers.” The way that long-COVID is studied may pave a way forward for studying other chronic diseases using big data, thanks to these online communities.



