The year is 2024. At a small regional hospital, an automated call has just come in, triggered by a patient’s personal fitness-monitoring device, which has detected several sudden and drastic anomalies—a sharp spike in pulse rate followed by an extreme slowdown, and slow and shallow breathing. Data from her smartphone reveal she just experienced a very sudden deceleration of key vital signs. The artificial-intelligence triage system monitoring the incoming data puts the pieces together and concludes the patient has been in a car accident and may be seriously hurt and possibly unconscious. An ambulance is called, and the first responders are given the accident location and the patient’s vital signs before even arriving at the scene.
On the way to the hospital, the medical technicians use onboard diagnostic imaging systems to examine the patient and transmit data and images instantly to the emergency room, where a surgeon is already scrubbing up while perusing the patient’s full medical history as well as the incoming data on a heads-up virtual-reality display—a more sophisticated successor to the Google Glass and Oculus Rift devices of the previous decade.
Once inside the emergency room, the surgeon is assisted by an autonomous robotic device with flexible arms and nimble fingers to perform basic tasks. A microscopic camera attached to the surgeon’s virtual-reality goggles displays precision views of tiny blood vessels as he carefully stitches them together. Noninvasive monitors keep track of a far more complete suite of physiological parameters than even invasive systems typically tracked a decade earlier.
Similar no-contact monitors evaluate the patient continuously during her stay, even as she walks through the corridors, providing the medical staff with an instant warning of any changes in her condition that might require medication or other intervention.
Several days later, the patient is discharged, wearing a comprehensive noninvasive monitoring system that sends data continuously back to the hospital to track her vital signs as she goes through a lengthy recuperation. And she’s delighted to know that she was sent home days earlier than she would have been in earlier years, thanks to the security provided by that constant monitoring.
It sounds like science fiction, and right now it is. But all of the elements that make up this futuristic vision of an intelligent, high-tech hospital are already in existence or close to it, at least in prototype form. And some say there is every reason to believe that the pace of technological advances in hospital equipment—and outside-the-hospital follow-up equipment—will only keep accelerating.
For example, new, more portable diagnostic systems and noninvasive patient monitoring, whether inside a hospital room or at home going about daily activities, have the potential to produce a drastic change in the experience of both in-hospital treatment, and in systems that can often obviate those hospitalizations or at least shorten their duration. Such systems have the potential to save billions of dollars in medical expenses and eliminate unnecessary and risky procedures, potentially saving lives and improving health outcomes.

“Ultimately, the goal is that we’d like to be in a situation where every interaction with the health care environment becomes an opportunity to learn more about how to take care of that patient better and an opportunity to see what works and what doesn’t, so that we can continuously and incrementally improve the care of the patients, improving their health as well as improving the health care system,” says Doug Fridsma, chief scientist in the Office of the National Coordinator for Health Information Technology.
Dr. Fridsma, who holds M.D. and doctorate degrees in biomedical informatics, explains, “We’ve taken an approach guided by the way the Internet has grown over time. Rather than trying to architect a singular system that’s going to be able to provide all of the functionality that we would like to see, we really look at this as a process of creating the right standards and building blocks that then can be used to create new functionality that perhaps we didn’t even think about.” Once those data become integrated, accessible, and standardized to allow for meaningful comparisons, he continues, “Wouldn’t it be great if somebody figures out a way to use these standards to come up with something that we never imagined, that’s going to transform the way health care is delivered and the way in which we can engage patients?”
We may be at the cusp of some significant transformations in those systems, some analysts say. Dr. Darren Dworkin, senior vice president of Enterprise Information Systems and chief information officer at Cedars-Sinai Medical Center in Los Angeles, California, declares that looking ahead a few years, “medical equipment that exists in the hospital today will be more intelligent and guided, as we go through this explosion in technology. I see rapid growth in imaging technologies. And less-invasive surgeries will be feasible as imaging technology continues to advance.”
“There’s a whole bunch of market forces and technology forces that are colliding at the same time and place,” says Tim Reha, a digital strategist and technologist who created a series of interactive Digital Health Summit events earlier this year, in conjunction with the International Consumer Electronics Show. These forces, he says, are all helping to bring about significant advances that will affect how both patients and physicians experience a hospital visit.
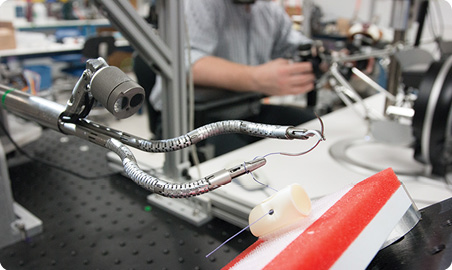
For example, in future operating rooms, “We’re at the advent of soft robotics, not the rigid robots we’ve been used to, but precision machines that are soft like we are, that can take on a form factor that we don’t have, such as miniaturized microrobotics that can go in and do things that we just can’t. They can use haptic feedback and all kinds of sensors that can guide the procedure. And then you always have to build in the telepresence,” so that experts can be virtually brought in to share their particular skills. Before long, Reha remarks, some surgical-assistive robots could be “something like an octopus, with microrobotics that can do interesting things,” using multiple kinds of precision tools on its multiple appendages.
“We’re kind of at an inflection point,” he says, “where we’re going from wrist bracelets and things like that, that give you some idea of your data, to more passive things, almost like smart homes that can, for example, monitor the urine in your toilet, and your refrigerator doors opening, and your smart pillows—all your interconnected devices working together like a mesh.” And all those data could be collected in your own privacy-protected database, where intelligent systems could begin to detect patterns and warning signs. And long before they get disseminated to typical homes, such interconnected systems will provide a degree of in-hospital monitoring for average patients that is comparable to what today’s patients get in an intensive care unit, he says.

“We can imagine that health care providers will have access to super-powerful tools,” Reha continues, “miniaturized versions of what they have now in the hospitals, so they can bring them to the point of care. And data will flow from that point of care to the hospital and to other experts through telepresence, connected through their mobile devices—tablets or robotics—to a care path that is streamlined and set up so that when you get out of the car, when you get put in the ambulance after the car accident, that pathway is set up to speed up your care, when every second counts against you.”
Joe Kiani is founder and chief executive officer (CEO) of a company called Masimo, which makes one of the most comprehensive noninvasive continuous monitoring systems available today. The lightweight and wireless system, called Radius 7, can continuously monitor several parameters, including oxygen saturation, pulse rate, respiration rate, and hemoglobin, and can send that information to a computer program that can alert the physician to any anomalies that might indicate pulmonary, cardiac, or internal bleeding problems.
“The patient can get up from bed and still be continually monitored, noninvasively,” describes Kiani. “It allows patients to be mobile, yet give accurate readings of their condition,” and do so continuously for as long as needed. It uses a simple optical sensor to detect pulse and blood oxygenation through the skin and another patch that picks up tiny vibrations that can be analyzed to reliably detect the respiration rate—something that Kiani says proved to be surprisingly challenging to detect without invasive sensors.

Such systems could have a dramatic impact if widely deployed in hospitals, he adds. “The majority of patients in hospitals are not monitored today. There are 200,000 hospital beds in the United States, and most of them are checked only once an hour. If you stop breathing, it often goes undetected. It’s one of the leading causes of preventable deaths in hospitals—in third place after cardiac diseases and cancer.” The widespread availability of constant monitoring could prevent many of those deaths, Kiani declares.
But in addition, this system will allow massive new collections of long-term monitoring data, which can be mined to reveal patterns that might otherwise not be noticed, he says—“maybe hours before, maybe more, before something happens. That’s not being done today.”
Other noninvasive monitoring systems are becoming available or are under development at many companies. Some of these require no patient contact at all, functioning entirely through precision video imaging, for example. A great variety of options are already becoming available now, and such systems are still in their infancy (see “Profiles in Hospital Innovation”).
[accordion title=”Profiles in Hospital Innovation”]
Intuitive Surgical Inc.
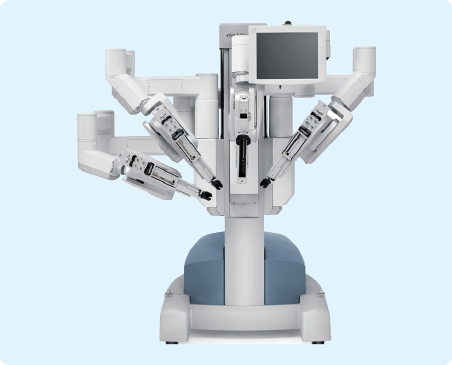
Already a market leader in surgical robots, California-based Intuitive Surgical this year introduced a new version of its widely used da Vinci surgical robot. The new Xi Surgical System was used for the first time this year at a hospital in Austin, Texas, and the company says among its innovations are a greater range of motion and the ability to upgrade the system through both software and hardware. The company’s initial technology came from research at the Stanford Research Institute, initiated by the U.S. Army for potential battlefield surgery, and in 2000, it was the first system to get U.S. Food and Drug Administration (FDA) approval for a robotic surgical device.
Titan Medical Inc.
This Toronto-based company was cofounded by a surgeon, Dr. Reiza Rayman, who holds a doctorate in telesurgery in addition to an M.D. degree and in 1999 was part of a team that performed the world’s first robotic heart bypass surgery. Now, this fledgling company aims to bring robotic surgery, which is already estimated to be a US$4 billion annual business, to much wider use. The company says its new robotic device, the SPORT Surgical System, expected to see its first use in Europe next year and soon thereafter in the United States, will be more compact and mobile than existing systems, allowing it to function in smaller operating rooms and to move easily on its mobile base from one operating room to another. Rayman was quoted recently saying that “Surgeons can use the technology to augment vision and to augment natural manual dexterity,” and he adds that recovery time for patients after robotic surgery has been greatly reduced compared to conventional surgery.
Masimo

Joe Kiani, an Iranian-born electrical engineer and entrepreneur, founded Masimo back in 1989 as what he describes as a “garage start-up,” and it has now grown to a 2,500-person company and a leader in noninvasive patient monitoring, whose technologies are used to monitor 100 million patients worldwide. The company has over 575 patents, and this year introduced its most comprehensive monitoring system, the Radius 7. Kiani also leads a nonprofit organization, the Patient Safety Monitoring Foundation, which is promoting a pledge among all companies in the field to share anonymized patient data to allow for data “mining” that could reveal correlations that might be impossible to discover otherwise and could lead to patient-specific treatment recommendations, Kiani says. More than 30 companies have already joined this effort.
Sensiotec Inc.

Taking noninvasive patient monitoring a step further, Sensiotec has introduced the world’s first no-contact monitoring system, which received FDA approval this year. Using a radar-based system, its Virtual Medical Assistant can (Figure S4) provide cardiorespiratory data as well as monitor movement and location, with no wires or attachments. The company was founded by Robert Arkin, a lawyer who previously founded several other electronic and medical companies, in 2008, and the company’s chief medical officer, Neal Templeton, is a former president of the American College of Radiology. The Virtual Medical Assistant is designed to allow for early detection and warning of any signs of clinical deterioration in hospitalized patients.
[/accordion]

In addition to diagnostic systems and surgical tools, a critical area for technical improvement is in the availability and usability of medical records and data, which are also at the early stages of a radical expansion of capabilities. For example, Bettina Experton, who holds M.D. and master’s degrees in public health, has been the CEO for 20 years of a company called Humetrix, which focuses on creating improved information systems for hospitals, patients, and emergency personnel to get instant access to complete medical records, in a form that makes them easily comprehensible to patients and makes it easy to home in on the relevant information.
Experton explains that a recent federal initiative called Blue Button has gone a long way toward ensuring that medical records from many sources, starting with the Veterans Administration, will be available in a uniform format that is making accessing and collating records much more feasible, and that system has already made some inroads into the nation’s health care system.
The digitization of records has been happening rapidly, but what has been missing is ways of integrating them. “In 2009, only 10% of hospitals were using digital records,” Experton explains, with 90% still limited to old-fashioned paper record-keeping systems. “Today, that proportion has been reversed, with 90% of hospitals now using digital records.” That’s an impressively rapid deployment of the new technology—at least within the confines of the hospitals. However, she says, “they don’t communicate with the wider community” of the health care system.
“When patients are discharged, if they enter a rehab facility or a sustained care or nursing facility, typically the electronic records don’t communicate” with the systems used in those facilities, so information may get lost along the way. “That’s where a lot of errors occur,” she says. But new systems, some of them already available today, such as the IBlueButton software that Humetrix provides, allow the patient to carry those records along personally, in an easy to access form that other health care providers can immediately download to their own iPads or other devices, just by scanning an optical code generated by the software (and a passcode to ensure confidentiality).
“A physician’s diagnosis and treatment depends on having a patient’s complete and accurate medical history,” asserts Experton. And although the federal rules now ensure that all records relating to Medicare treatment as well as from Veteran’s Administration facilities must adhere to the new standards, that still leaves a vast amount of older records, and even current records, that may not yet conform and will require tedious conversion processes to incorporate into a coordinated system.
Fridsma, who practiced medicine at Mayo Clinic Scottsdale before joining the federal Office of the National Coordinator for Health Information Technology (ONC) explains that “I think we’re in this period of transition, and I think it’s going to set the stage for a number of changes. For example, one of the things that’s different is that only one person can look at a paper record at a time, unless you make a copy, but with electronic records, it’s possible for that information to be shared much more broadly, not only with a primary care doctor but also with some specialists and with networks of providers that can then provide much more information at a patient’s fingertips than they ever had before.”
But of course there are a lot of challenges that will have to overcome to do that. “One challenge will be to set up the right set of standards that will support interoperability and the right business drivers to make sure that people share information,” he says.“And then we’ll have very high-quality data that we can use to make inferences, and learn from, and actually provide better care.”
As an example of the way better data can lead to better health care outcomes, Kiani points out that the ability of his company’s device to continuously monitor hemoglobin could save many lives as well as significant unnecessary expenses. A recent study at Massachusetts General Hospital showed that availability of continuous hemoglobin monitoring led to a 90% reduction in the number of patients who ended up getting blood transfusions.
That’s a significant finding, Kiani says, because “This can stave of unnecessary blood transfusions,” which have their own health risks. In addition, he says, by eliminating the unneeded procedures, “That alone will save billions of dollars.”
More broadly, the whole health care system could end up becoming much more efficient, from end to end. As Reha puts it, “because of the microchip, the network, the portability, the battery power, a mesh of broadband, connected devices, now what we’re seeing is that what happens in the consumer areas permeates all businesses. People are used to that really smooth experience from Apple, from Google, with a lot of things running in the background where the technology is kind of invisible, and interfaces like Siri, that I think we’re going to see things change really rapidly in health care technology as well.”
In Reha’s vision, “The intelligent hospital is something that’s now in the palm of your hand. It’s the background, it’s your robotic house. Really smart, transparent health monitoring that just surrounds you. It could see inflection patterns in your voice on your cell phone, if your voice changes because you’re sick,” and trigger a call to check and see if all is well.
Before long, such systems could not only improve the way care is given in hospitals but go a long way toward helping people decide whether that hospital visit is necessary in the first place. “In the future,” describes Kiani, “if you wake up at 3 a.m. with chest pains, instead of trying to decide whether you need to call 911, you’ll be able to just connect the home health monitor, and it immediately connects to the central facility, where a doctor can see your face, see your color, and see the data from the monitor.” Instead of having to make a personal decision that could potentially be a life-or-death choice—and doing so while half asleep and possibly impaired by your medical condition—the remotely linked doctor can be the one to make the determination: the doctor “will either tell you to come in Monday, or he’ll say that he has already dispatched an ambulance to come pick you up,” Kiani says.
The hospital of the future, in short, will work much more quickly and efficiently to provide better and faster care. From emergency room visits to surgery to hospital stays to outpatient care, the coming hospital will seamlessly integrate high-tech systems to improve patient outcomes. Doctors, nurses, pharmacists and other clinicians will be able to easily confer and communicate. That future may not be here yet, but it will be soon.



