Using state-of-the-art technology, athletes at the Paralympic Games achieve great feats of physical prowess, but for most people using assistive and rehabilitative technologies (ART), even simple tasks can present huge challenges. Many do not make full use of the technology available to them because it is unreliable, uncomfortable, and nonintuitive, so researchers are pushing the envelope to create practical solutions that function like real limbs.

Standard solutions use a socket attached to the end of the limb into which a prosthesis fits. Some users can learn to flex certain muscles to operate a hand, but, for others, the muscle ends are too damaged. Electrodes and wires on the skin can restrict natural movement, and the signals they transmit to the prosthesis are often unclear. Much research in the United Kingdom is focused on designing more responsive limbs and linking prostheses to the nervous system.
“Some 80% of prosthetic limb wearers will discard it in two years,” says Leonor Stjepic (Figure 1, right), chief executive of the Restoration of Appearance and Function Trust (RAFT). “Amputees report discomfort, the fact that prosthetics can be hard to get on and off, and a lack of functionality. Even the most sophisticated prosthetics cannot give the functionality of a person’s own limb and require a lot of learning gestures. We want to develop an intuitive technology.”
A New Hope
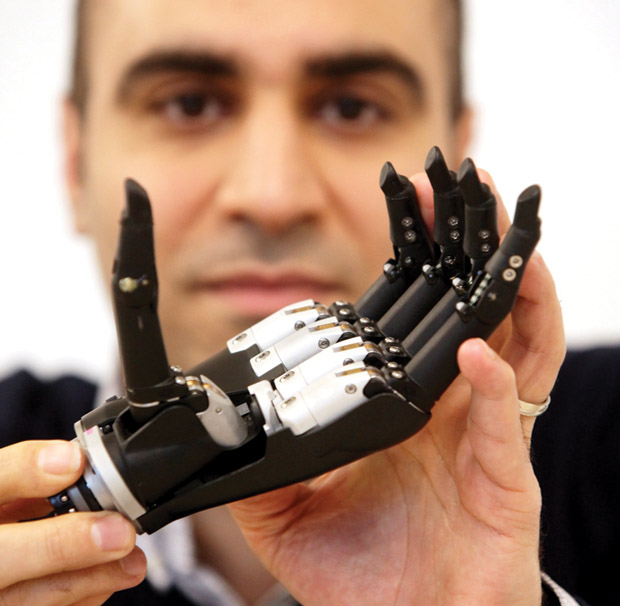
One exciting project is being led by Dr. Ravi Vaidyanathan, senior lecturer in biomechatronics with the Department of Mechanical Engineering at Imperial College London, and research postgraduate Samuel Wilson, who have developed a prototype sensor system that detects mechanical signals from the vibration of flexing muscles. In contrast to customary electromyography (EMG), which detects electrical signals through a socket connected to the stump, mechanomyography (MMG) uses microphones and a motion sensor system to detect muscle and arm movements.
“The idea of sensing mechanical sounds has been around for a long time,” Vaidyanathan explains. “Before EMG, clinicians would use stethoscopes to listen to muscles. A challenge for automatic use has been capturing the signals using accelerometers and microphones while removing interference. Another trigger was when my colleague Dr. Sandra Shefelbine was working on motion tracking with accelerometers and picked up interfering signals that could have been muscle vibrations.” Moreover, as Vaidyanathan points out, “EMG typically uses a wet electrode with conductive gel, so sweat can be a problem impacting electrical signal consistency, and EMG sensors normally cannot be reused. Dry electrode EMG technology has potential, but few systems have yet worked well outside the clinic. MMG is much simpler. There is no electrical connection, no electrodes, and no conductive gel, and sensors are reusable indefinitely. With our sensor, we want to capture motion and muscle activity together.”
So far, there have been no clinical trials, and there is a long way to go before any commercial application emerges. A prosthetic hand has been field-tested by Alex Lewis, who, in late 2013, developed Strep A toxic shock syndrome, septicaemia, and necrotising fasciitis, which resulted in a quadruple amputation, extensive skin grafts, and facial reconstruction. Myoelectric, microprocessor, and muscle-intuitive prosthetics are essential to his daily life, so he was eager to participate in the tests of the new bionic hand, which allowed him to perform both a light, three-fingered pinch and a power grip.
“The new state-of-the-art bionic hand is a big change from the myoelectric unit I have from the NHS, which is bulky and labor-intensive, has a short battery life, causes fatigue, and requires a lot of muscle training” says Lewis. “Amputees need functionality from devices they can wear all hours of the day. We need to replicate more movements for the hand, but it could be life-changing. At around £100 for Ravi’s system compared to £8,000 for some alternatives, the cost reduction could be revolutionary for the 130,000 amputees in the United Kingdom, the 4.5 million in the U.S., and the countless more in Africa and elsewhere.”
There is a long road ahead for Lewis and Vaidyanathan, but the so-called “Star Wars hand” holds great promise. “In the short term, we are looking at a human/machine interface for it. It has so many potential applications,” Vaidyanathan remarks. “Right now, we are raising money to do further trials, and we will work more with Alex. We also want to try MMG on legs because of the problems EMG has with sweat.”
Awakening Sensation
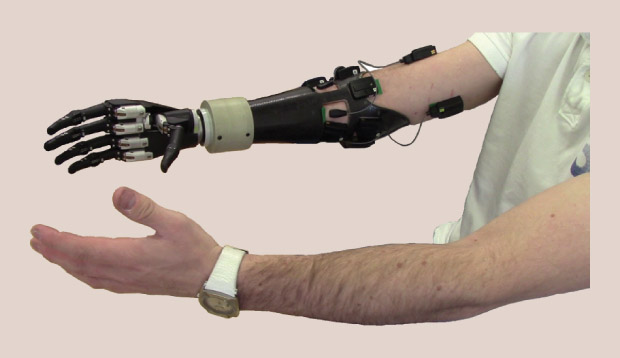
In the Biomedical Engineering Department at Newcastle University, Dr. Kianoush Nazarpour and his team are focusing on how to produce a prosthetic hand that can sense pressure and temperature (Figure 2). The project is backed by £1.4 million from the U.K.’s Engineering and Physical Sciences Research Council, which brought together 28 experts for a week in a remote hotel, where they worked with no mobile phones and no Internet to define key research projects.
According to Nazarpour, “Three projects emerged, including the bionic limb project, in which we are looking at what we need from the next generation of limbs. The electronic interface between the body and the prosthetic limbs has not changed for 80 years, though there has been a lot of mechanical development. Existing technology is superreliable but limited. Now, we need an interface with the body at a neural level with semiconductors that sit on nerves and communicate with the brain.”
Supervised from Newcastle University, the project involves specialists from the universities of Leeds, Essex, Keele, and Southampton, as well as Imperial College London, in a truly collaborative effort that typifies the U.K.’s approach.
“Our short-term goal is to make tiny electrodes 50-μm thick,” Vaidyanathan continues. “It is a challenge to implant them in human nerves, so we are looking for a protocol to implant them for stimulation and to keep them in the body for a long time because the body rejects microchips. I’m working on the grammar of the language that is needed to talk to the brain. There is a long way to go on the neural side—the more we look, the more questions we find.”
Still, Vaidyanathan remains hopeful. “In the long term, we are looking at prosthetics that are as good or better than the original limb. It is a very distant prospect, but it will be a prosthetic that is part of the body. You will be able to move the limb without looking at it” (Figure 3).
RAFT’s Bionic Limb project is also examining neural interfaces. The 18-month project, which will lead to clinical trials, is developing a solution that will eliminate surface wires and create intuitive, practical, and affordable prosthetics using electrodes implanted in the muscles that feed signals to the prosthetic through a bone anchor.
We have gone for a practical, long-term solution that is less like science fiction than some solutions,” says RAFT CEO Stjepic. “We are looking at how to capture electronic signals from muscles and nerves— the brain still sends these signals—and how to send them to a prosthetic hand. We can do that, but we need to create a feedback loop that returns signals to the brain. At first, we are looking at sensing shape rather than temperature, for instance, because the ability to naturally feel for small, everyday things without looking would make a big difference to people’s quality of life.”
Organization and financing are paramount. As Stjepic adds, “We are working on the electronic elements with University College London because they are leaders in the field of prosthetic limbs. The big challenge is to get the people to invest money in clinical trials and technology transfer. The United Kingdom is streets ahead in terms of innovation, ideas, and research; however, unlike the U.S., it is not as good at the investment stage.”
In the Vanguard of Innovation
These projects and many others put the United Kingdom firmly at the cutting edge of the development curve for ART. “The United Kingdom is certainly a player in rehabilitation technology, engineering, and robotics on the international stage,” says Imperial College’s Vaidyanathan. “These are very important areas of research over here.”
Nazarpour agrees: “The U.K. is the best place to do bionics research. We have 100 years of history here in neuroscience. No lab has everything—especially in the U.K., where the dimensions are smaller than in the U.S.—but we have many of the world’s top universities, and we ensure that collaboration is sustained. The U.K. is number one in terms of technology.”

Research ranges from next-generation prosthetics to solutions that support nonamputees with critical physical functions. A good example is the Wearable Soft Robotics for Independent Living project, which is led by Prof. Jonathan Rossiter at the University of Bristol (Figure 4, right) and which could support long-term assisted living in ways that conventional rigid robotics cannot. Researchers at seven U.K. universities are developing potentially ubiquitous, low-cost, and highly adaptable soft robotic clothing. This intelligent clothing—or “second skin”—could, for instance, give people additional bionic strength to move between sitting and standing positions.
Starting from the fundamental chemistry, Rossiter’s team will build nanostructures, then 1-cm thick layers, and, finally, a full device with control systems and power. A full demonstration model could be ready in three years. Like Vaidyanathan’s bionic hand, this technology could deliver enormous cost savings.
“Current robotics are rigid, hard, and mechanical,” Rossiter explains. “They are not sympathetic to movement—they move in spite of you rather than with you—and they are not necessarily compatible with skin and muscles. We want to make something that works with the body and moves in a more biological way. For example, we could strap on muscles to replace those under the skin. They must be wearable, washable, comfortable, and work with the biomechanics of the body. The technology must not only be big enough to replace the body’s muscle but fabricable and resilient over millions of operations.” The challenges are ongoing: “It may take five years or more to adapt existing technologies,” he adds.

Alongside such high-tech solutions, there is another strand of research that looks at the most fundamental aspects of using prosthetic limbs. The University of Strathclyde’s Department of Biomedical Engineering, for example, is using laser scanning or a hydro-scanning tank to let water capture the shape of amputees’ stumps to achieve an accurate fit for sockets.
“We are all inspired by Paralympians and elite athletes, but the majority of people with amputation are older and usually lose limbs through cardiovascular disease,” says Sarah Deans, a teaching fellow of prosthetics and orthotics at Strathclyde (Figure 5, right). “One of the biggest problems is that they need a socket that fits and is comfortable to wear all day. A lot of work is being done with carbon fiber to make lighter prostheses and with neurointerfaces to improve functionality, but the socket is the most important thing. We need to go back to basics.”
Whatever area of development one looks at in rehabilitative technology, one thing is certain—the United Kingdom is leading the way on innovation. The desire among researchers now is to see that creativity married with a level of funding rarely seen outside the Unites States.



