In 2010, the World Health Organization estimated that 285 million people exhibit some form of vision impairment. Of these, almost 40 million people are functionally blind [1]. Yet, 80% of blindness could either be treated or avoided at the point of onset.
The vast majority of avoidably blind people reside in low-income countries, where the number of practicing ophthalmologists is critically low. Indeed, throughout the world, there is an inverse relationship between the prevalence of blindness and the number of eye care providers within reasonable reach. As an example, in Kenya there are 86 ophthalmologists to provide care to a population of over 40 million people. Given this order of magnitude in the disproportion between population size and number of care providers, it is clear that, in low-income countries, eye care can only be provided on a sustainable basis by screening the population for eye disease in the community and then referring only patients who would benefit from further diagnostics and treatment to the very scarce specialist care.
In high-income countries, such as the United Kingdom or the United States, the need to approach eye screening directly in the community is equally critical. Major medical conditions, such as diabetes, high blood pressure, or stroke, require constant attention to eye health. Patients with these conditions are required to undergo regular eye screening and monitoring. However, as life expectancy is increasing, the median age of the population rises, and older people exhibit a higher incidence of these conditions. For example, the World Health Organization estimates a doubling of diabetes deaths from 2005 to 2030. Health care provision services are facing increasing pressure, and shifting eye screening and monitoring from secondary to primary care, or even to the community is, therefore, key in ensuring the sustainability of large-scale health care provision. Ideally, patients should be able to access eye screening programs with sufficient ease to shift the very concept of eye care from the early treatment of eye conditions to the maintenance of good eye health.
For population screening to be possible, the technology must meet some core requirements. It needs to be operable by non–eye care specialists, such as family doctors, community nurses, pharmacists, or school teachers. It needs to be affordable. Importantly, it needs to be seen as friendly by the patients. Would we want to be screened with devices that have the same appeal as a dentist drill?
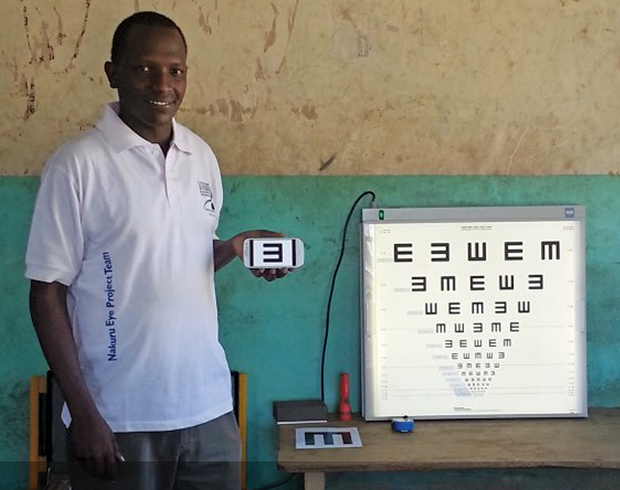
To this end, mobile phone technology appears ideal. Modern mobile phones are effectively a hybrid between a computer, an acquisition system, and a telecommunication device. They offer a good quality camera to capture images of the eye. They present a sophisticated visualization interface, useful both for simple tests, such as showing letters to read, and to display eye images for analysis (Figure 1). Their computing power is comparable to a personal computer, and this allows sophisticated image enhancement. Telecommunication is in their very nature, giving them intrinsic telemedicine capabilities. And, most importantly, they are found everywhere, ubiquitous both in low- and high-income countries. Looking again at the indicative example of Kenya, there are more people who can access mobile phones than those who have access to clean, running water. This availability, unprecedented for any other electronics-based technology, ensures that, in developing eye screening tools for mobile phones, we can assume widespread literacy, both among the operators and, importantly, among the patients, who perceive phones as familiar and friendly elements of their daily life (Figure 2).
Phone-Based Opthalmoscopy

In eye screening, the examination of the retina through the eye’s pupil (ophthalmoscopy) is a key requirement. Arguably, from an optical device point of view, it is also the most difficult to implement. At present, ophthalmoscopes rely on optical designs developed in the mid-1800s. They are difficult to use, and the level of specialist skills required severely limits their application by untrained personnel or by practitioners making infrequent use. A United Kingdom case study by Dalay, Umar, and Saeed (2013) reports how, due to the lack of familiarity of the doctors with the procedure, even in such a critical setting such as acute admissions to an accident and emergency unit, only 20% of patients who should be having their retina examined actually receive such examination.
Therefore, if we want to approach ophthalmoscopy for eye screening, a solution that can be used by personnel with minimal training is strongly and urgently needed. Yet, photographic images of the back of the eye are often simpler to obtain than performing direct observations, and they have been recorded for more than a century. The image quality offered by mobile phones is reaching levels comparable to good digital cameras. Photographic resolutions in excess of 10 megapixels and video recording of 4K quality are now available in mainstream commercial mobile phones. For screening, retinal photography definitely appears as the correct approach.
The implications of a mobile-based digital ophthalmoscope would be far-reaching. Of specific advantage to ophthalmoscopy, phones offer an intuitive interface for image acquisition, storage, visualization, and basic evaluation. They are sophisticated telecommunication devices, and images can be retransmitted for remote analysis by an expert operator or, prospectively, by automated image analysis software. Were an inexpensive and simple-to-use phone-based retinal imager to be made available, this would enable screening in the community of socially important pathologies such as glaucoma, diabetic retinopathy, agerelated macular degeneration, forms of hypertension, malaria, and many neurological diseases.
Not surprisingly, ophthalmoscopy attracts the highest effort in the development of mobile devices for eye care. A number of solutions are now starting to appear for mobile-phone-based ophthalmoscopy, both commercially and on the research scene, albeit still suffering from technology infancy issues [2]. Mainstream manufacturers have put on the market adapters that couple popular phone models to traditional ophthalmoscopes, upgrading them to telemedicine functionality, yet without overcoming the intrinsic difficulty of use of the original instruments. Ophthalmoscopy devices specifically dedicated to mobile phones have also recently become available, albeit at costs unattractive for screening, especially in low-income countries. Very recently, a simple solution has been made available, which is prospectively offered on an open source basis [3]. A 3D printed plastic arm holds a lens in front of a phone, in a configuration known as “indirect ophthalmoscopy.” While functional, it still requires a high level of skill to be used.
Providing Access to Eye Care: Peek
An interesting case study highlights a specific approach that may differentiate mobile-phone-based screening from more traditional technology. When Andrew Bastawrous, from the London School of Hygiene and Tropical Medicine, went to Kenya for a community study on eye care, he found himself in a logistic nightmare trying to transport the necessary bulky screening equipment around the villages. He then teamed up with the University of Strathclyde, in Glasgow, United Kingdom, and the Glasgow Centre for Ophthalmic Research of the National Health Service (NHS) Greater Glasgow and Clyde, United Kingdom, and they pooled their complementary expertise in international eye health, biomedical engineering, and ophthalmic research.
Today, the Portable Eye Examination Kit (Peek) [4] is being tested in field trials in Kenya, Mali, Malawi, Tanzania, Botswana, Madagascar, India, and the United Kingdom, and testing in more countries is planned in the future. Peek is a comprehensive and integrated smartphone-based tool kit that comprises the full set of core tests needed for eye screening, designed to be used by operators with minimal to no training. It is composed of a smartphone app and a low-cost adapter for retinal imaging, both optimized for ease of use, and it allows operators to test for the core vision problems—testing for visual acuity, color, and contrast sensitivity, image grading cataracts—and for photos of the back of the eye to be taken, saved, and sent to experts for diagnosis, follow-up, and arranging treatment.
However, unlike the many other approaches in mobile-based eye screening, Peek’s primary aim is not to enhance or replace existing diagnostics tools. Rather, Peek aims to link patients with eye care providers. Peek is specifically oriented and optimized toward eye screening in the community. With this, it helps to identify, directly in the community, by nonspecialist community workers, the people who need to be seen by an ophthalmologist, increasing access to high-quality eye care.
Outlook
The unprecedented opportunity offered by mobile technology to transform eye care is driving transformational innovation. We are witnessing a wealth of successful demonstrations of devices that interface to existing ophthalmology technology that augment smartphones with eye care functionalities, and that aim to redefine field and community screening. They will not only allow better diagnostics, treatment, and follow up of eye patients but, importantly, by enabling population screening, they will link potential patients to doctors and avoid the burden of unnecessary referrals.
These initial efforts will now need to face the opportunity and challenges presented by the dizzyingly fast evolution of the mobile phone market, not least the need to keep up with the constantly changing specifications of mobile handsets. Furthermore, standards and protocols for the use of mobile phones in health care, in general, and in eye care, in particular, are only beginning to exist and are still lacking a solid framework.
Even more substantially, delivering health care is effectively a succession of many stages interacting with each other, and the larger the size of the population involved, the higher the importance of an efficient and effective workflow. To date, of the many successful pilot studies in mobile health, only a small minority have managed to fit successfully into the workflows of actual health care provision and, hence, be adopted. Mobile-based eye screening now faces the need to dive deep into this challenge. If successful, it may well revolutionize the way we look at eye care.
References
- World Health Organization, “Visual impairment and blindness,” Fact Sheet No. 282, 2010.
- N. M. Bolster, M. E. Giardini, I. A. T. Livingstone, and A. Bastawrous, “How the smartphone is driving the eye-health imaging revolution,” Expert Rev. Ophthalmol., vol. 9, no. 6, pp. 475–485, Dec. 2014.
- OpthamalicDocs [Online].
- Peek Vision [Online].



