Proteome editing could help treat diseases that antibodies and drug therapies cannot reach
At a time when a global vaccine program is being rolled out at unprecedented speed, the world is more aware than ever before of the wonders of medical science. There are, however, many diseases that remain beyond the reach of modern medicine and the potency of some of our most widely used therapies are waning.
Microbes evolve rapidly, adapting to their environments and, through mutations, maximize their chances of survival. The constant evolution of bacteria, viruses, fungi, and parasites can result in resistance to antimicrobial drugs. Methicillin-resistant Staphylococcus aureus (MRSA) is the most common antibiotic-resistant infection in humans, but it is far from the only one. In addition, there are many infectious diseases with which antibodies cannot cope, and many genetic diseases cannot yet be treated despite great strides forward in genome editing. Such conditions are, however, the fuel that drives innovation.
One of the pioneers of genome editing, David R. Liu, professor of chemistry and chemical biology at Harvard University (Figure 1), is among those opening up potential solutions to the problem of antibiotic resistance and making fundamental advances towards therapies for conditions that antibodies cannot treat.

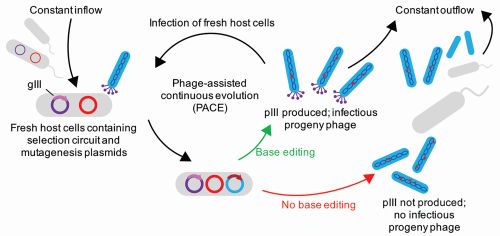
In his work on technologies for rewriting the human genome, Liu focused on turning on or switching off genes to rewrite errors in the genetic code. More recently, he has refined a technology he helped to develop back in 2011, phage-assisted continuous evolution (PACE), which takes a similar approach to the human proteome, the set of proteins that can be expressed by the genome, cell, or tissue. “Virtually every biological process is modulated by proteins, including every disease process,” Liu remarks. “So, the ability to manipulate the structure of a protein is important to the study and treatment of disease.”
The power of proteases
PACE automates the random mutation system that most researchers use to develop new proteins, more powerful DNA base editors, and enzymes that can deliver amino acids into living organisms (Figure 2). Until now, however, the technology had been unable to effectively evolve proteases.
Proteases are enzymes that increase the rate of proteolysis, or the breakdown of proteins into smaller polypeptides or single amino acids. They have rarely found their way into therapeutic applications, but with Liu’s latest iteration of PACE, it has become possible to create new proteases that can target a specific string of amino acids within a protein and cut—or cleave—the protein at that point. Every cell contains hundreds of proteases, which can destroy or mutate proteins. When a protease cuts off a specific part of a protein, it modifies its function. As examples, such cleaving could potentially turn off the Tau proteins responsible for creating the intraneuronal tangles that cause Alzheimer’s disease, or might turn off Ras proteins that, when persistently active, can cause many psychiatric disorders.
What Liu and his team have achieved with PACE is the ability to massively accelerate the evolution of a protease—effectively simulating millions of years of mutations—to the point where it can cleave a chosen protein rather than its current natural target. “Proteases are nature’s evolved solution for controlling the structure and function of proteins,” Liu notes.
“For decades, researchers have seen the potential of proteases as tailor-made biological therapies, but they have proven difficult to create in the laboratory with specific properties,” Liu says. “For therapeutic purposes, they need to be incredibly specific for their targets.”
Writing the next phage
PACE relies on the properties of bacteriophages—viruses that infect and replicate within bacteria, ultimately destroying them. Bacteriophages are found wherever bacteria exist and are believed to be the most abundant organisms on the planet. For more than a century, they have been used as treatments in their own right, largely as an alternative to antibiotics. Although phage therapy took a back seat when antibiotics became widely available, it is once again emerging as a potential means to tackle drug-resistant bacteria. It relies on matching bacteriophages to specific bacteria—effectively using viruses to kill off bacterial infections. Deadly to those bacteria, phages are harmless to the host organism.
For Liu, bacteriophages are the building blocks of the PACE platform, which uses them to rapidly evolve and reprogram variants of the Botulinum neurotoxin (BoNT) light-chain proteases to greatly improved substrate selectivity. Proteases with bespoke protein cleavage specificities are created through dozens of generations of evolution per day—with minimal human intervention—to selectively cleave a specific protein.
The first phage selected for evolution was BoNT/X—better known as botox. A promiscuous protease, it is unique among BoNT proteases, as it cleaves naturally to a number of vesicle-associated membrane proteins (VAMP1, 2, 3, 4 and 5, plus Ykt6). Until now, it has been hard to push the application of BoNT proteases beyond this small set of protein targets, but PACE has already evolved four BoNT protease variants that selectively cleave both native and non-native substrates, including VAMP7 and phosphatase and tensin homolog (PTEN). The enhanced PACE platform also enables proteases to be reprogrammed through both positive selection (what amino acids to cleave) and negative selection (not cutting specific amino acid bonds).
Therein lie potentially huge breakthroughs. The evolution of a protease that can cleave PTEN, a protein that restricts cell growth, is highly significant. PTEN is found in nearly all of the tissues in a human body and is known to act as a tumor suppressor due to its role in regulating cell division. The researchers were able to selectively shut down PTEN, which could encourage the regrowth of neurons, thus promoting better recovery after a severe injury.
“There has been no good way to evolve a protease to cleave a protein of our choosing, until now,” Liu explains. “Our system has that capability for the proteins that we have studied so far, the challenge being that proteases and proteins are so vast in number. There are many proteins of interest out there, and we don’t know if we can reproduce the success that we had with PTEN in 5%, 20%, 50% or more of them.”
The first steps on a long journey
The results Liu and his team achieved were beyond their expectations. All four evolved proteases cleave their new substrates with very high specificity. BoNT proteases evolved in this system also showed the ability to potently self-deliver into primary neurons in extremely small concentrations. Those results have opened up a myriad of potential applications for what is known as proteome editing.
As human therapeutics, proteases offer many advantages when compared to antibodies. Because they act as catalysts, each protease molecule can process many substrate molecules, not just one, which means much higher potency than antibodies. Furthermore, proteases can activate proteins rather than simply bind or inhibit them and can increase or decrease a protein’s lifespan.
“Antibodies can do far less than proteases,” Liu remarks. “Antibodies hug their targets to death, but you need one antibody molecule per target molecule, and the binding can be reversible. Also, they cannot activate a protein, unlike a protease. A protease is a catalyst to activate or manipulate the properties of a molecule. BoNT is so powerful at self-delivery that the required dose might be as small as a nanogram, and in such a low dose it would not be immunogenic.”
The main reason proteases have not been widely adopted as human therapeutics was the lack of a technology to create proteases that could cleave a specific protein target. With the latest version of PACE, Liu has developed precisely that technology. It could make editing the proteome possible, just as Liu’s other work has made it possible to edit the genome.
“It was an ambitious goal to develop a BoNT protease that could cleave a class of proteins it was not previously known to cleave,” he says. “The results were a real eye-opener. The specificity was a pleasant surprise. Now, we are pursuing targets in the lab that might result in therapeutic outcomes.”
Although he is not ready to commit to specific outcomes, Liu is currently working on selectively cleaving PTEN to enable it to deliver itself into neurons and perhaps stimulate neural regeneration. That could open up treatments for Alzheimer’s, Parkinson’s, and a host of other neurodegenerative diseases.
His search for specific therapeutic targets will initially target those areas in which no drug therapies currently exist or where antibodies are ineffective. For some diseases, antibodies are either not known or might not be useful. For instance, antibodies find it hard to get into cells, so intracellular bacterial infections—among them the bacteria that cause tuberculosis, malaria, and AIDS—are beyond their reach. Proteome editing could change that.
Liu’s work on genome and proteome editing may have dramatic therapeutic implications. One, however, is much more straightforward than the other. “Protein cleavage is simpler than genome editing,” Liu remarks. “If you have a protease that can recognize six or ten amino acids selectively, then that specificity gives you a high chance of cleaving a specific protein in the human body, which is easier than cleaving a specific site on the human genome, which has more than 20,000 genes that can make proteins.”
It is certainly too early to declare the end of a specific disease due to proteome editing, but at a time when the treatment of many diseases remains out of reach and antibiotics are becoming less of the panacea they once were, the prognosis for proteome editing is as good as it gets.