In developing countries like India, noncommunicable diseases such as diabetes have already replaced communicable diseases as the major cause of death. According to the recent Indian Council of Medical Research’s India Diabetes study, an estimated 62.4 million people in India have diabetes [1]. With increasing urbanization and industrialization, we can only expect this number to grow. Moreover, all diabetes efforts in India are currently focused in urban areas, while 70% of India’s population lives in rural locations. The lack of awareness due to illiteracy, lack of trained professionals (doctors and paramedical staff trained in diabetes), limited access to health care due to problems with transport and infrastructure, and unaffordability due to poverty are some of the major obstacles to delivering diabetes health care to rural regions. Screening for diabetes is hardly ever done in rural regions, resulting in a much larger burden of undiagnosed diabetes and potentially leading to higher rates of diabetes-related complications due to delayed diagnosis and/or improper treatment.
The current statistics demonstrate that urgent interventions are mandatory to curb the epidemic of diabetes and its complications at the grassroots level. This gap in providing diabetes care can be filled by the use of telemedicine. Telemedicine is defined as a tool that uses telecommunication to support health care in remote zones, and its main purpose is to facilitate a beneficial interaction between the patient and the health care provider to achieve improved treatment and lower treatment costs. It helps reduce the burden for health care personnel so that only those patients with more advanced disease requiring tertiary-level treatment need to be brought to the specialist hospitals in cities for management. In India, the telemedicine concept was introduced in the year 2000 in Andhra Pradesh by Apollo Aragonda Hospital. In 2006, we initiated telemedicine at the Madras Diabetes Research Foundation through the Chunampet Rural Diabetes Prevention Project (CRDPP) in the field of diabetes to provide mass screening and diabetes health care and prevention to a rural south Indian population in the southeastern state of Tamil Nadu through a combination of telemedicine and personalized care [2].
The Chunampet Rural Diabetes Prevention Project Model
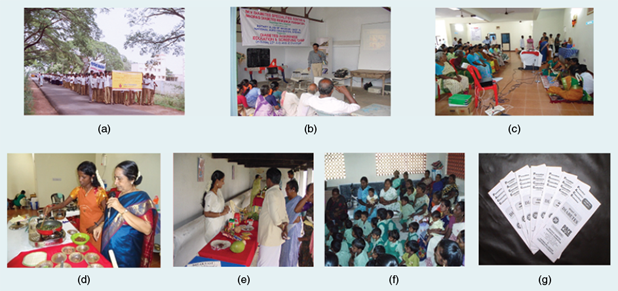
CRDPP was undertaken in collaboration with the World Diabetes Foundation in Denmark and the Indian Space Research Organization in Bangalore, India. Using a telemedicine mobile van loaded with appropriate equipment, trained technicians, and satellite technology, we screened for diabetes and delivered diabetes care to remote villages in southern India. The project planned to offer services at the following levels: to screen for and reduce the risk factors for diabetes (primordial prevention through mass-scale diabetes awareness programs), to prevent diabetes in those identified with prediabetes (primary prevention through lifestyle modification advice), to prevent the complications of diabetes in those already diagnosed with diabetes by controlling the disease (secondary prevention through screening for complications and glycemic control), and, finally, to offer treatment to those who already had some complications to prevent the progression to the end stage of these complications (tertiary prevention). The CRDPP was undertaken in a cluster of 42 villages in and around Chunampet in the Chithamur block of the Kancheepuram district of the state of Tamil Nadu in southern India, which has a total population of 43,158 (Figure 1).

A door-to-door diabetes screening was carried out in 23,380 of the total 27,014 people in the adult population (aged 20 years or more) living in the 42 villages using a fasting capillary blood glucose (CBG) test done by a handheld glucose meter. A structured questionnaire was administered; anthropometric measurements including weight, height, and waist circumference were obtained using standardized techniques; and blood pressure was recorded. Of those screened, 808 were self-reported diabetic patients, and 609 individuals who had a fasting CBG ≥126 mg/dl were then subjected to a 75-gm oral glucose tolerance test (OGTT) (using venous blood) to confirm the diagnosis, of which 330 individuals were diagnosed with diabetes. Thus, of the screened individuals, 1,138 (4.9%) had diabetes and 3,410 (14.6%) had prediabetes.
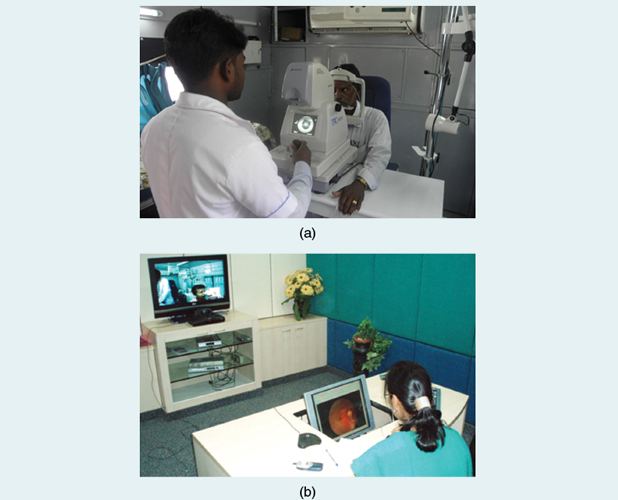
The 1,100 diabetic individuals (confirmed to have diabetes by the OGTT and all self-reported diabetic subjects), underwent screening for diabetes-related complications, including eye disease/retinopathy (retinal photography and slit lamp), nerve problems/peripheral vascular disease (Doppler), foot problems/neuropathy (biothesiometry), heart problems/coronary artery disease (electrocardiogram), and kidney disease (microalbuminria), in a fully equipped mobile telemedicine van with very small apperture terminal (VSAT) satellite connectivity by trained technicians and an optometrist. Unlike in urban areas, where qualified or trained paramedical staff are usually available, in rural regions, it is extremely difficult to find qualified people. Hence, village health workers (VHWs) and unemployed youth who had a basic high school qualification were recruited. In this way, we were able to employ local young men and women and foster community support for the program. We recruited 15 VHWs and gave them intensive training on all aspects of the study for a period of 15 days and further retraining at six-month intervals at our tertiary care center (Dr. Mohan’s Diabetes Specialities Centre at Gopalapuram in Chennai). The mobile van also had other facilities for blood sampling, videoconferencing equipment with a television screen, air conditioning, a generator for uninterrupted power supply, computers, a laser printer, and basic furniture. The glycemic control of self-reported diabetes subjects was assessed by measuring Hemoglobin A1c (HbA1c) levels. The entire screening in the van was offered free of charge to all individuals (Figure 2).

Seven-field stereo color retinal photographs were taken in the van and sent by satellite network to our center in Chennai. The ophthalmologists graded the photographs using the Modified Early Treatment Diabetic Retinopathy Study Grading System. Using video conferencing, the consultants interacted with patients, explained the present condition, and formulated the treatment and follow-up plans. The consultants also used the opportunity to educate patients about diabetes. Similarly, photographs of severe foot lesions were also transmitted to the center for further opinion on follow-up. We found that only about 2% of patients needed referral to Chennai for laser photocoagulation or hospitalization for foot complications [2]. All surgeries were offered free of charge or at subsidized rates, and, in addition, free transport to Chennai was provided (Figure 3).
Individuals with diabetes and early complications identified through screening were then offered follow-up care at the Sai Rural Diabetes Specialities Centre, our rural diabetes center established at Illedu near Chunampet in the Kancheepuram district. Those who could not afford to pay were given free treatment, while others were treated at heavily subsidized rates. This center is staffed by physicians and paramedical staff who were all recruited locally but trained at the main hospital in Chennai. At the one-year follow-up of the glycemic control of the diabetic subjects, it was observed that the mean HbA1c levels decreased from 9.3 ± 2.6% to 8.5 ± 2.4% (Figure 4).

Factors Contributing to Success
The CRDPP telemedicine model, which has proven to be sound, effective, cost-effective, and practical, has been highly successful and was well received by the local community. Its success was due, in part, to the support of and collaboration between multiple stakeholders, including the philanthropist who donated the land; the building that we constructed; the World Diabetes Foundation, Denmark, which provided a fully equipped van and initial salary support for four years; and the Indian Space Research Organization, which provided the satellite support for the telemedicine facilities. The project staff as well as its local partner organizations at Chunampet, including the National Agro Foundation (a nongovernmental organization), developed an excellent partnership with the members of the community, which ensured their continued support of these activities. The screening was mostly done by people without formal education who were given hands-on training.
Measuring Impact
The most tangible benefit of the program has been its help in detecting and managing diabetes and its complications in remote rural areas where medical facilities are nonexistent. It has provided individualized health information and employment opportunities to many of the local youth—thus providing a source of livelihood to the villagers, increased awareness of diabetes through education, enhanced decision making in clinical management, and easy access to diabetes care. The Sai Rural Diabetes Specialities Centre, along with an effective referral system, has dramatically reduced the number of patients needing to travel to specialized centers in urban areas, thus improving compliance rates. This has directly translated into the improved control of diabetes in the whole community with a reduction of HbA1c by nearly 1% within a year in the entire cohort of people with diabetes in the 42 villages using low-cost generic drugs. The CRDPP model is found to be specifically useful as the patients do not need to travel substantial distances to visit a specialist for proper diagnosis and treatment. From a health provider perspective, this program is attractive as it does not require the full-time services of highly qualified specialists (Figure 5).
The CRDPP has been recognized as a model for screening and delivering diabetes care to rural regions in developing countries [3]. This successful rural diabetes screening and care model can now be replicated and made available in other parts of our country where specialized diabetes care facilities may not be available.
References
- R. M. Anjana, R. Pradeepa, M. Deepa, M. Datta, V. Sudha, R. Unnikrishnan, A. Bhansali, S. R. Joshi, P. P. Joshi, C.S. Yajnik, V. K. Dhandhania, L. M. Nath, A. K. Das, P. V. Rao, S. V. Madhu, S. K. Shukla, T. Kaur, M. Priya, E. Nirmal, S. J. Parvathi, S. Subhashini, R. Subashini, M. K. Ali, and V. Mohan, “Prevalence of diabetes and prediabetes (impaired fasting glucose or/and impaired glucose tolerance) in rural and urban India: Phase 1 results of the Indian Council of Medical Research-INdiaDIABetes (INDIAB) study,” Diabetologia, vol. 54, pp. 3022–3027, 2011.
- V. Mohan, M. Deepa, R. Pradeepa, V. Prathiba, M. Datta, S. Ravikumar, H. Rakesh, Y. Sucharita, P. Webster, S. Allender, A. Kapur, and R. M. Anjana, “Chunampet. Prevention of diabetes in rural India with a telemedicine intervention,” J. Diabetes Sci. Technol., vol. 6, pp. 1355–1364, 2012.
- V. Patel, S. Chatterji, D. Chisholm, S. Ebrahim, G. Gopalakrishna, C. Mathers, V. Mohan, D. Prabhakaran, R. D. Ravindran, and K. S. Reddy, “India: Towards universal health coverage 3—Chronic diseases and injuries in India,” Lancet, vol. 377, pp. 413–428, 2011.



