Access to health care has long been considered to be a human right. It was formally declared in 1946 when the heads of states wrote the constitution of the World Health Organization (WHO). But more than 70 years after the fact, the global community still has yet to achieve it.
More than 20 years after the writing of the WHO constitution, world leaders signed the Declaration of Alma-Ata in 1978. This declaration was intended to spearhead an international call for primary health care as the first step of achieving universal health coverage. Access to primary health care means that every person can receive comprehensive care—from annual physical checkups to routine screening for disease, rehabilitation, and treatment—close to where they live and work. The signatories of the declaration believed that the governments of countries are responsible for providing access to these health services for all. And at the end of the day, expending the resources to ensure increased health care coverage is ultimately a boon for public health: studies have shown that routine access to primary health care is an effective and efficient way to address the main causes and risks of poor health and prevent emerging challenges, such as epidemics and antibiotic resistance through regular screening and surveillance.
Although the goals of the Declaration of Alma-Ata have yet to be attained, some governments have made strides in expanding access with moderate success. By 1990, the rate of child mortality decreased by more than 50%. And although people are living longer, half the world’s population today still lacks full coverage for essential health services, including care for noncommunicable and communicable diseases, maternal and child health, mental health, and reproductive health.
In October 2018, world leaders met in Astana, Kazakhstan, to discuss at length the promise that technology provides for expanding primary health care coverage. Henrietta Fore, UNICEF’s Executive Director, highlighted the importance of technology in achieving health care for all. Although innovation is certainly needed to develop new drugs, it’s “also about applying existing technology in new ways to bring vital services closer to hard-to-reach populations,” Fore says. The hope is that through digital technologies on our smartphones and other means, different tools can help deliver medical services and supplies that are essential to maintaining people’s health and well-being, and be one way to expand primary health care to those who need it most.
“Healthcare technology is critical,” says Austen Peter Davis, a Senior Adviser for the Norwegian Agency for Development Cooperation. “It’s potentially a game changer. It can assist in meeting primary healthcare goals to understanding public health challenges, or to power individuals to participate in their own health.”
A New Use for Text Messaging
While mobile phones—particularly smartphones—tend to compete for our attention, the devices that we use can also be adapted for different health care needs. Already, private institutions, nonprofits, and international agencies are taking advantage of the accessibility and increased use of mobile phones.
One technology that has been used for over a decade is a tool developed by UNICEF in 2008, called RapidSMS. On this platform, which can be used by anyone with a mobile phone and doesn’t require the capabilities of a smartphone, users can send text messages on any mobile device to a designated short-code, which would initiate a series of text messages so that the user can provide more information. The back-end of RapidSMS is opensource and can be adapted for a variety of needs.
If the user—such as a community health care worker in a rural village—wanted to provide medical information, the data collected by the centralized system could be relayed to hospitals weekly. In Malawi and Zambia, RapidSMS was utilized to expedite the delivery of HIV test results for infants directly to health clinics. Typically, mothers would learn about their child’s HIV status after one to two months, but RapidSMS helped reduce the time that results were sent back, which meant children received treatment earlier rather than later. Health workers in Malawi also use RapidSMS to monitor malnutrition in children under five years old using messages containing coded information about age, weight, and height.
UNICEF is now using a different iteration of RapidSMS called RapidPro to address a variety of needs. To date, RapidPro is used in approximately 60 countries worldwide and is specifically used for health purposes in about half of those countries, according to Sean Blaschke, a development business analyst with UNICEF in Kenya. Like its predecessor, RapidPro is also open-source and is SMS-based. In Nigeria, health care workers at regional clinics use RapidPro to communicate with the state on whether or not they have enough vaccines in stock and their storage conditions, as a means to maintain a sufficient supply.
The mobile phone as a diagnostic
Beyond SMS-based technologies, others are developing mobile apps employing machine learning and artificial intelligence that essentially make smartphones into diagnostic tools. And as smartphones become more affordable and ubiquitous, they can perhaps replace traditional tools used in delivering health services.
One such application, called Feebris, is starting to show promise in diagnosing respiratory conditions, such as pneumonia, asthma, or chronic obstructive pulmonary disease. The idea first occurred to biomedical engineer Elina Naydenova when she was working as an intern with the WHO’s medical device group in 2014 (Figure 1, right). At the time, she was studying childhood pneumonia, a condition that kills a million children under the age of five every year worldwide. It’s a complex condition to diagnose: even in a developed country with medical experts, a number of medical tests and experts are needed. But early diagnosis can help save more than 40% of the lives lost, Naydenova says.
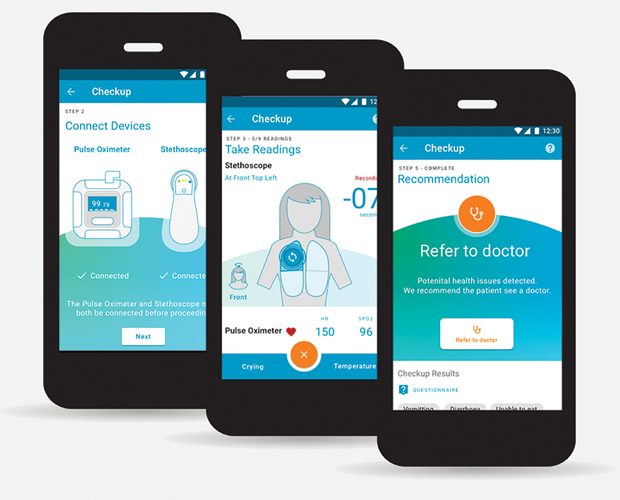
She wanted to take that complexity and precision of diagnosis to low-income countries with Feebris, which uses machine learning to diagnose respiratory disorders. So far, it has been tested in the urban slums of Mumbai on approximately 1,300 children among ten community health workers. She is looking to expand the program to be tested on 10,000 children in the coming months as part of a new child health program in India (Figure 2).

Feebris takes signals from digital stethoscopes and pulse oximeters that measure blood oxygen levels and pulse to come up with an overall diagnosis. Once these measurements are taken and uploaded to the mobile app, the algorithm essentially replicates what a pulmonologist would do: listen for sounds like crackles and wheezes in a patient’s breathing. These new measurements from patients are compared to data collected from hospitals already paired with a diagnosis. Once a diagnosis is made, a child can then be referred to a local community hospital, if needed, for treatment (Figure 3). So far in Mumbai’s slums, this technology is around 85% accurate compared to diagnoses made in the clinic. Naydenova and her colleagues at Feebris are also trying to see if the technology is accurate in diagnosing respiratory conditions in the elderly.
Others are also creating diagnostic tools using machine learning and artificial intelligence for different conditions. For example, catching skin cancer at its early stages often means it’s easier and cheaper to be treated. To this end, Amsterdam-based Skin Vision has developed a mobile app that allows patients to perform regular self-checks on themselves for skin cancer. After taking a photo of a perhaps troublesome skin spot or mole, the photo is compared with a database of skin lesions that correlate to low, medium, or high risk, and within thirty seconds, the app will tell the user whether or not they should seek additional medical care.
New Toys
Researchers and engineers are also working to develop multimodal devices that combine different sensors to bring medical care outside the clinic.
Naydenova, for instance, is using a wearable that has an electrocardiogram, pulse oximeter, thermometer, and other sensors integrated into one device to feed information to Feebris. Having one sensor to measure a range of health functions also works better for children, she says. “The more devices we have, the more distracted they get. If you couple this [tool] with the algorithms we’re developing, we can get a whole profile of the pulmonology, respiratory, or cardiac profile of a patient’s health,” she says. “The next five years will see a huge emergence of opportunities when hardware becomes more affordable and prolific.”
Researchers at Radboud University Medical Center in the Netherlands are also developing a smart multimodal device shaped like a hospital pager called Checkme to measure vital signs—such as body temperature, heart rate, and blood pressure—which could be used as a tool for daily patient monitoring in or out of a hospital. These measurements are then uploaded to a patient’s chart using Bluetooth via an app that communicates with the device [1].
Repurposing Drones
Like other countries in sub-Saharan Africa, Malawi is among one of the hardest hit by the HIV/AIDS epidemic. Because half of children who are born with HIV die before their first birthday, early diagnosis is key in preventing such deaths. But specialized centers in Malawi that can perform these early screening tests are often located days away from many villages. According to Judith Sherman, the Chief of HIV/AIDS in Malawi, there are only about nine laboratories for a country of more than 18 million people. It could take three weeks to get a test result back before a child could start treatment. So in 2014, UNICEF wanted to improve the timeliness of returning such test results to the parent, and thought to use drones to transport diagnostic samples to and from patients to hospitals and the lab.
In 2016, UNICEF worked with the government and different ministries of Malawi to set up a study to assess whether or not it was feasible to have drone corridors set up in-country. Fortunately, these initial pilot tests worked, and importantly, “it built up confidence in using drones within Malawi,” says Sherman.
No drones are currently being used yet, but Sherman hopes they will be operational in early 2019. They hope to first target communities that are in need, based on historical data trends.
Challenges
Despite the abundance of different apps, devices, and technologies that are being adapted or developed to expand or better primary health care, one of the biggest challenges is having to integrate it into a country’s existing health care system.
UNICEF knows this painstaking task well, as it has worked with health ministries and other governmental agencies to implement its technologies. The success of RapidPro, for example, is due to the fact that UNICEF has collaborated with countries’ governments and non-governmental agencies. One of the biggest challenges of Rapid- Pro, says Blaschke, is having a system to manage the influx of large amounts of data. And because RapidPro is based on SMS messaging, UNICEF needs to work with mobile phone operators in each country to make sure each network is streamlined for RapidPro so it can be accessed by anyone with a mobile phone.
The number of technologies in development won’t necessarily mean that each will be widely used. First, it would have to be tested on a large scale. However, “there’s not a clear way to break into the bureaucracy of healthcare systems to get something tested rapidly,” says Riina Sikkut, the Minister of Health and Labor of Estonia. “The real barrier is between technology [development] and acquisition in healthcare.”
And moreover, too many available applications and technologies might run the risk of health care becoming disintegrated. “There is no research [so far] to assess the reach, adoption, implementation, maintenance and fidelity of these interventions,” says Teng Liaw, a Primary Health Care Researcher at the School of Public Health and Community Medicine in Sydney, Australia.
In spite of these challenges, software developers, governments, and other agencies should at least strive for further innovation: in some areas of the world, new technologies have already shown great promise in reducing costs and simplifying primary care.
Reference
- M. Weenk et al., “A smart all-in-one device to measure vital signs in admitted patients.” PLoS ONE, vol. 13, no. 2, p. e0190138. 2018.



