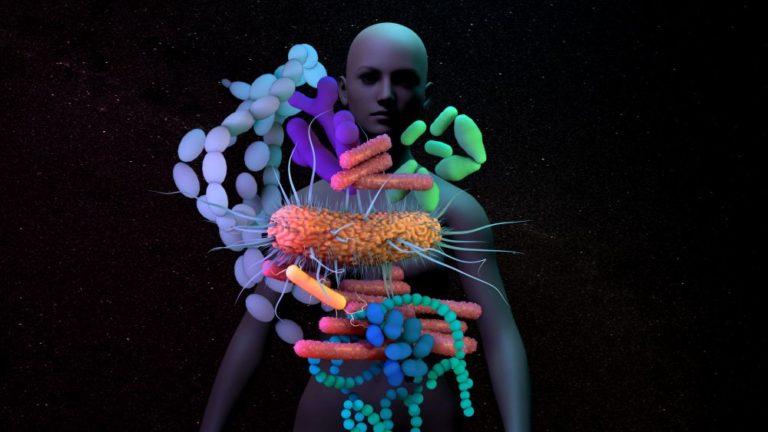
Only ten years ago, the idea that bacteria in your gut could affect your brain and behavior was seen as a fringe theory. But today, it is well-established that the trillions of microbes in the gastrointestinal tract—collectively known as the gut microbiome—profoundly influence the brain. Now, researchers are working to harness the power of the gut microbiome to develop new treatments for brain disorders.
Gut–brain connection
Our gut microbiome plays an important role in overall wellbeing by helping us make and absorb nutrients, supporting our immune system, and producing chemicals essential for brain function. The gastrointestinal system, its resident microbes, and the brain communicate via the gut-brain axis, a complex network of neurons, hormones, and proteins that allow the brain to send messages to the gut and vice versa.
Dysregulation of the gut-brain axis (from things like stress, illness, or poor diet) is not only associated with digestion problems, but also increasingly linked to brain disorders. Over the last decade, thousands of papers have implicated the gut microbiome in disorders including Alzheimer’s disease, autism spectrum disorder (ASD), multiple sclerosis, depression and anxiety, and Parkinson’s disease (PD).
This explosion of interest has propelled the gut-brain axis into mainstream brain science, making longtime proponents of its importance feel less like evangelists, says John Cryan of University College Cork (Figure 1). “I spent a long time trying to convince neuroscientists to think about things below the neck, to think about how the gut could talk to the brain and how this could be relevant for psychiatry,” he says. “Now, almost every traditional neuroscience, psychiatry, and neurology meeting has a microbiome session.”

Much of the evidence for the role of the gut microbiome in modulating brain function has come from animal studies. Experiments with germ-free mice have shown that the brain is affected in the absence of microbes, while administering specific microbes to rats can result in behaviors associated with anxiety or depression [1]. Other animal studies have used antibiotics, probiotics, or fecal microbial transplants to provide further evidence that gut microbes regulate the brain and influence behavior [2].
The results from these animal studies are supported by preliminary work in humans. Epidemiological studies have found that differences in the gut microbiota coincide with various mental illnesses, including depression, anxiety, and schizophrenia. For instance, people with schizophrenia often have an impoverished gut microbiota and blood markers indicative of gastrointestinal inflammation. Patients with depression and anxiety also seem to have less overall diversity in their gut microbiomes than people without mental health problems [3].
From mouse models to patients
Some promising work translating findings from animal subjects to human patients has come from Sarkis Mazmanian’s group at the California Institute of Technology (Figure 2). About 12 years ago, Mazmanian was researching how gut bacteria shape the gastrointestinal immune system. A colleague, Paul Patterson, developed a mouse model of ASD called the maternal immune activation model. Epidemiological studies suggested that infections in a mother during pregnancy increase the risk of ASD in her child. Patterson’s model showed that one could induce autism-like behaviors in mice by giving their mothers infections during pregnancy.
When Mazmanian examined the intestines of these mice, he found evidence of dysfunction and inflammation. Interestingly, studies report that children with ASD often have gastrointestinal issues, as well as exhibiting characteristic changes in their gut microbiomes. Mazmanian’s group went on to demonstrate that in the maternal immune activation model of ASD, mice with behavioral deficits also had changes in their gut microbiota and intestinal permeability, similar to the features reported in humans with ASD [4].

Further work with this mouse model elucidated how an infection in pregnancy can trigger a cascade of activity that ultimately contributes to ASD symptoms. In the mother mouse’s gut, an infection can stimulate specific immune cells to produce a small molecule called IL-17. This molecule travels into the brains of developing pups, binding to brain receptors. Mazmanian showed that IL-17 alters the development of particular brain cells in the fetus, leading to anxiety-like behaviors in adults [5]. His lab has already developed a small molecule that binds IL-17 as it is produced in the gut. It improved behavior in the mouse model and reduced anxiety in a small clinical trial with humans. A larger, randomized, controlled trial is now underway.
Mazmanian also turned his attention to PD, a neurodegenerative condition in which gastrointestinal issues commonly co-occur. In fact, most PD patients are diagnosed with clinical constipation years, if not decades, before their motor symptoms emerge [4]. In PD, a neuronal protein called α-synuclein aggregates inside neurons. While the normal function of this protein is to aid in dopamine transmission, when it clumps up, it leads to the death of the cell. Using a mouse model of PD, Mazmanian investigated whether the gut microbiome contributes to the symptoms and pathology of PD.
“We did experiments that involved antibiotic treatments, fecal transplants, and germ-free mice,” says Mazmanian. “In every experiment, those features of human PD that we can model in mice—the motor symptoms, neurodegeneration, and α-synuclein aggregation—were significantly affected by the microbiome.” These experiments led Mazmanian’s team to a target: a protein called curli that is made by a strain of E. coli in the gut. In mice, curli can form aggregates that prompt other proteins, including α-synuclein, to misfold, first in the gut and later in the brain [5]. And levels of curli are elevated in human PD patients.
With this bacterial target in their sights, Mazmanian and his team went to work on designing a therapy aimed at curli itself, rather than the clumps of α-synuclein in the brain. “We developed a drug that inhibits the production of curli and administered it to these mice,” says Mazmanian. “And they recovered. Their motor symptoms went away and their brain pathology improved.”
Since misfolded proteins are also characteristic of neurodegenerative conditions such as Alzheimer’s disease and amyotrophic lateral sclerosis (motor neuron disease), the concept behind the curli-inhibiting drug could translate to these diseases. Mazmanian’s team is planning a clinical trial in PD patients later this year and completing the first experiments to see if similar bacterial proteins are implicated—and could potentially be targeted—in Alzheimer’s disease.
Microbiome-based therapies
Although researchers are still probing the mechanistic details underlying microbe involvement in brain disorders, the prospect of new therapies for some of these intractable diseases is generating excitement. Delivering therapies into the brain has been a long-standing challenge, but manipulating the microbiome is relatively easy.
“The lowest hanging fruit for intervention is diet,” says Emeran Mayer of the University of California, Los Angeles (Figure 3). “In the next five years, people might come up with bioengineered microbes or assemblies of microbes that can overcome colonization resistance and produce specific molecules, but immediately, one can change the diet.”
Mayer says the existing evidence consistently supports increasing the intake and variety of plant fibers and reducing or eliminating ultra-processed foods. A diet like the traditional Mediterranean diet, which is rich in plants, unsaturated fats, and vegetable oils and low in refined sugars and red and processed meat, has been shown to increase gut microbe diversity and reduce physiological changes such as chronic inflammation [3]. “It does not seem to matter what is lacking in the microbiome; this diet is optimal for gut health,” says Mayer. “In the future, this could be more targeted. But right now, we know that if you carpet bomb the system with healthy food, your gut microbiome will benefit.”

Another emerging therapy to alter the microbiome is the fecal microbial transplant, where microbes from a healthy gut are transplanted into another person to repopulate their microbiome with diverse microorganisms.
Jane Foster of McMaster University says there is promising evidence that fecal microbial transplants can benefit people suffering from more than just gastrointestinal disorders (Figure 4). “In one study, researchers identified differences in the microbiome between responders and nonresponders to a particular cancer immunotherapy treatment,” she says. “Then they went a step further by taking the microbiome from the responders and transplanting it into the nonresponders, and the nonresponders’ outcomes improved.”
Foster also points to evidence of success with fecal microbial transplants in children with ASD. She says that while not everyone responds to the therapy, those that do respond have symptom improvement persisting at least two years.
A growing number of researchers are looking to so-called “psychobiotics” for the treatment of various neurological and psychiatric disorders. The term, coined by John Cryan and Ted Dinan, refers to microbiome-targeted interventions including probiotics (beneficial bacteria) and prebiotics (material that promotes the growth of such bacteria) [6].
At Axial Biotherapeutics, a company co-founded by Mazmanian, researchers are working to identify live biologics, such as specific commensal strains of therapeutic bacteria, as well as more traditional small molecules, to translate findings in mice to patients with ASD and PD. “The drugs being developed by Axial are gut-retentive and do not enter into circulation,” says Mazmanian. “We know that we can deliver molecules to the gut and drug microbial pathways, and by manipulating those, we can ameliorate neurodegeneration and behaviors linked to autism.”

“In just a decade, we have taken this concept that microbes shape behavior, originally in mice, and been able to design rational drugs for humans. There is a long way to go and no guarantee of clinical success, but the initial results are quite encouraging.”
Hope or hype?
While it is becoming clear that gut microbes impact psychiatric and neurological illnesses, we are still very much in the early days of these investigations. Questions remain about whether microbial changes are the cause or a complication of such disorders, as well as the mechanisms by which gut microbes exert their effects. Further studies in humans are required to substantiate the clinical use of potential treatments like psychobiotics and fecal microbial transplants.
Mayer, cautious not to over-interpret results from animal studies, says he still has a healthy skepticism about treating brain disorders via the microbiome. “I think we are at a stage where we can say a diet that is optimal for the diversity and richness of the microbial ecosystem probably benefits all these diseases,” he says. “Later, there may come a time when we are able to personalize it and recommend specific diet modifications for particular diseases.”
One challenge that remains is how to define a healthy microbiome when differences between cultures and even individuals can be great. Gut dysbiosis is just one of my contributors to psychiatric and neurological illnesses, meaning that microbiome-targeted treatments may help only a subset of such patients.
“We have not yet come to the point of identifying who will benefit from probiotics and other treatments,” says Foster. She, like Mayer, predicts that microbiome-targeted treatments will need to become more personalized and precise to have the greatest benefit.
Cryan sees the field moving in this direction. “People are beginning to understand that you can’t just take a probiotic from a health food store and expect it to do something,” he says. “That’s like walking into a pharmacy and picking a random drug to take because ‘medicine is good for you.’”
Despite the remaining questions and challenges, the promise of microbiome-based treatments for currently intractable brain disorders is an exciting prospect. Research in this area has exploded over the last decade; now, many researchers are predicting a boom of microbiome-based therapies in the next five to ten years. Time, and rigorous clinical investigations, will tell if the potential lives up to the hype.
References
- T. Meštroviс´, “Gut-brain axis and neuropsychological disorders,” News-Medical.Net, Feb. 26, 2019. [Online]. Available: https://www.news-medical.net/health/Gut-brain-axis-and-neuropsychological-disorders.aspx
- Y. K. Kim and C. Shin, “The microbiota-gut-brain axis in neuropsychiatric disorders: Pathophysiological mechanisms and novel treatments,” Curr. Neuropharmacol., vol. 16, no. 5, pp. 559–573, Jun. 2018, doi: 10.2174/1570159X15666170915141036.
- D. Robson, “How your belly could heal your brain,” BBC, Feb. 21, 2019. [Online]. Available: https://www.bbc.com/future/article/20190218-how-the-bacteria-inside-you-could-affect-your-mental-health
- E. Pennisi, “Meet the ‘psychobiome’: the gut bacteria that may alter how you think, feel, and act,” Science, May 7, 2020. [Online]. Available: https://www.sciencemag.org/news/2020/05/meet-psychobiome-gut-bacteria-may-alter-how-you-think-feel-and-act
- C. Willyard, “How gut microbes could drive brain disorders,” Nature, vol. 590, no. 7844, pp. 22–25, Feb. 2021, doi: 10.1038/d41586-021-00260-3.
- J. F. Cryan et al., “The microbiota-gut-brain axis,” Physiolog. Rev., vol. 99, no. 4, pp. 1877–2013, Oct. 2019, doi: 10.1152/physrev.00018.2018.