Above: CAVE2 at the Electronic Visualization Laboratory, University of Illinois at Chicago.
“Space. The final frontier.”
With this and other iconic phases, a legacy was born. 2016 marks the 50th anniversary of the original Star Trek television show, which painted a captivating vision of space exploration and potential technologies about 200-300 years in our future. Though the original Star Trek made its debut in 1966, in many ways, most of the technology it portrayed is still light years ahead. We will not likely witness a warp drive or an interplanetary “Federation” of governments in our lifetime.
Yet part of the appeal of Star Trek is the idea of technology integrated so seamlessly into the characters’ lives that it offered a tantalizing portrayal of what our future technology and health care could someday be, from regenerating tissue to transporting organic matter via energy beams. In fact, some of Star Trek’s technology has actually materialized in the last five decades: cell phones, for example, were inspired by the flip phone-like capabilities of communicators in the original series. And from asking Siri for directions to commanding our cars to call a phone number, we increasingly use more voice-enabled technologies that were first seen on Star Trek spaceships.
In addition, many of the medical technologies that first appeared fantastical are now emerging. From restoring vision to instantly diagnosing a patient, several technologies seem on the verge of providing life-altering solutions in our lifetime.
A Quick Diagnosis
Perhaps few things inspired more dread in Starfleet personnel then a command from Dr. McCoy or Dr. Beverly Crusher to go to Sickbay, a hybrid ER-hospital-rehab-morgue on the ships, chock full of seamless, integrated medical technology. The medical tricorder is the ultimate tool for Star Trek doctors. A handheld device, the tricorder could be waved over a patient to immediately determine a health condition and provide a diagnosis, even out in the field.
Imagine you are at home or work when a friend begins to have strange symptoms. It could be something benign like indigestion, or something more serious, like appendicitis or a heart attack. Especially when it comes to the very young, elderly, or chronically sick, being able to distinguish a life-threatening condition from a passing symptom would save lives, prevent stress, and reduce healthcare costs. It could also be vital in the many places around the world without easy access to medical doctors.
“There is a primary human need, for exploration or for survival, that drives science fiction ideas,” says Pelagia-Irene Gouma, professor and director of the Center for Nanomaterials and Sensor Development at SUNY at Stony Brook. “The medical tricorder answers to the human needs for protection, identity, and freedom—i.e., personalized health monitoring to ensure our welfare. This fiction is now becoming real.”
While there are a number of portable diagnostic tests and even smart phone apps in the market, these typically require manually entering symptoms or collecting samples like blood or urine to perform the analysis. But tools that could non-invasively scan for a health condition and recommend a treatment, similar to the tricorder, are currently in the works.
The XPRIZE Foundation, a Culver City, California-based group that attempts to push new technology developments through contests, launched the Qualcomm Tricorder XPRIZE in January 2012 to make the “medical tricorder” a reality. In conversations conceptualizing the prize, the organizers decided that Star Trek’s tricorder represented what this device should be and prototypes or designs entered in the competition had to be a noninvasive and user-friendly device that could diagnose 15 diseases including HIV, stroke, mononucleosis, heart disease, allergies, and type 2 diabetes by monitoring common health metrics and contextualizing the information for users. Judging for the prize will take place in 2017.
Interestingly, advances in breath analyzers may also provide a noninvasive, all-in-one medical diagnostic tool someday. The North Carolina-based NIOX’s VERO, for example, is an FDA-approved device that analyzes patient breath to detect airway inflammation particularly in cases of asthma. Other preliminary research efforts indicate that molecules in the breath can reveal if people have cancers or heart disease.
The challenge with analyzing breath for a wide range of disease is the overwhelming number of biomarkers (over 300 known chemicals in a single exhale) and the low concentrations of those chemicals. “The chemical complexity of the breath exhale gas mixture requires devices that can discriminate a single gas in order to have reliable diagnostics and this has not been achieved with the existing technologies,” says Gouma. Collecting information from a single exhale requires highly sensitive sensors and the limitations of current technologies involve exhaling many times over and over or exhaling at a controlled flow rate.
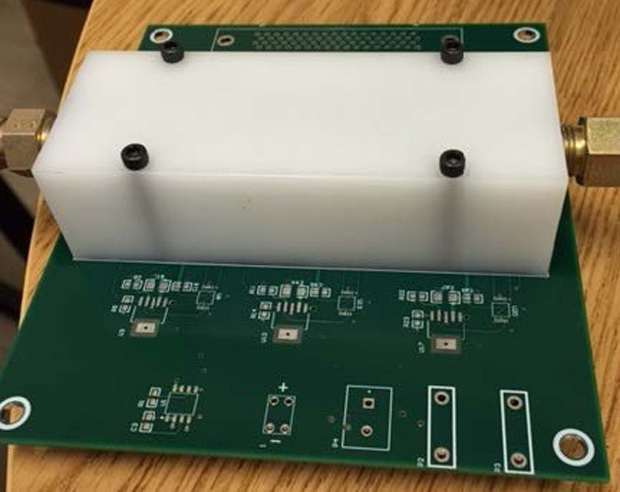
But developments in nanotechnology have allowed Gouma’s group to overcome some of these limitations and create a handheld, portable, single-breath diagnostic with selective chemical sensors that can detect and measure amounts of common biomarkers like nitric oxide, ammonia, acetone and others which can signal disease.
A Sense of Vision

One iconic symbol of Star Trek has been the VISOR (“Visual Instrument and Sensory Organ Replacement) of engineer Geordi La Forge. La Forge, a character said to be blind from birth, uses a visual prosthetic to see beyond the normal range of human vision across the electromagnetic spectrum, allowing him to peer into the infrared and ultraviolet. His special sight comes in handy on numerous episodes to detect problems and solve dilemmas.
Visual prosthetics—retinal implants combined with technology to provide a form of vision—have been on the rise, with a number of these in clinical trials or poised to hit the marketplace, but are a far cry from LaForge’s functioning visor. Many of these devices work by surgically implanting an array of electrodes on top of eye cells which then stimulate neurons in response to light. Aside from requiring invasive surgery, these devices are a small step forward, as they provide, at best, a distorted sense of vision with low resolution and also require a battery source.
Second Sight, which is based in Sylmar, California, has an FDA-approved Argus II Retinal Prosthetic System that restores some amount of visual perception in blindness by electrically stimulating the retina. It does not map directly onto the patient neurons—one downside of this is that a patient must move their whole head to focus on an object in their field of vision. The German-based company, Retina Implant AG company, uses an optical implant of approximately 1500 pixels that electrically stimulate the neurons and maintains the direction of gaze and vision.
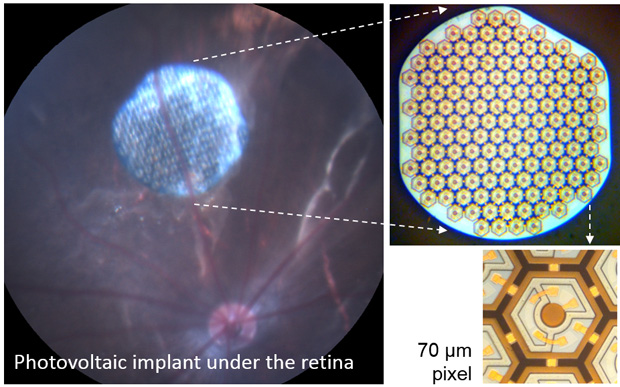
“Getting vision better than 20/200 is a major threshold that so far nobody has been able to cross,” says Daniel Palanker, a physicist and Stanford University professor who focuses on visual perception and optical augmentation. In response to that challenge, he developed a visual prosthetic called the Vision Restoration System (VRS) in partnership with the French-based Pixium Vision and plans to conduct clinical trials on the latest version—that aims to get to the resolution of facial identification—this year.
In Star Trek, there are many cases aside from visual prosthetics of inorganic technology and biology integrating into a working system. In a notorious example of cybernetics, technology fused with flesh in members of the villainous “Borg,” a colony of hybrid machine and biological beings that try to assimilate other characters into their brainwashed collective. Another character, the android Data, had biological components grafted onto his artificial systems. While there are a number of examples of inorganic material interfacing with organic (for example, advanced prosthetic arms or legs), incorporating inorganic material is still an obstacle in current research efforts.
“The biggest challenge for realizing the next generation of implantable bionic devices in general is to ensure that electrode technology intimately connects to the flexible, dynamic, microscopic world of the biology in ways that can survive for the lifetime of the recipient,” adds Nigel Lovell, a professor of biomedical engineering at the University of New South Wales in Australia (see also “Visions of a Bionic Eye”).
A Painless Injection
Many a child—and adult—rue the day they have to get a shot or vaccine. In Star Trek, characters are able to deliver medication or sedatives with a small hand-held device through the clothing with no needles (and no pain) via a concentrated, high-pressure blast. Aside from lessened pain, such a device could more easily and safely deliver medication or subdue thrashing patients.
Decades ago, needleless jet injectors were used to mass vaccinate against polio and other diseases but they were discontinued because they often broke the skin, were reported to be as painful as needles, transmitted infection, and were difficult to maintain. But new technologies have the potential to revitalize this approach.
In 2012, a group in MIT’s Department of Mechanical Engineering engineered a prototype that uses a magnet to shoot a liquid at a high velocity out of a miniscule nozzle at a range of controllable depths. Another device, a disposable-syringe jet injector (SDJI), developed by the non-profit, Seattle-based PATH organization, gets medication into the skin by shooting through a small hole at high pressure (imagine a tiny, powerful water pistol). In 2014, PharmaJet’s manufactured Stratis SDJI gained FDA-approved in the United Sates for a flu vaccine and is in the process of being approved by the World Health Organization, according to Darin Zehrung, who leads the Vaccine and Pharmaceutical Delivery Technologies portfolio at PATH.

“By operating without the use of needles, DSJIs hold promise for overcoming many of the persistent challenges and risks associated with needle-based injections and sharps waste,” says Zehrung. “DSJIs use a sterile, single-dose needle-free syringe and a pressurized liquid stream rather than a needle to penetrate through the skin and administer injections. Once an injection is delivered, the device’s syringe cannot be reused and must be discarded—removing the potential for cross-contamination.”
Such a device could be a boon to low-resource health systems, where the safe management and disposal of needles is a challenge, he adds.
A room of Virtual Reality
The holodeck, another well-used technology in Star Trek, lets people enter into any kind of simulated virtual reality situation they wish—you could have dinner with a revered historical figure, practice a virtual surgery, or spend the afternoon doing team-building exercises as pirates on the high seas.
In the real world, this technology, largely driven by the gaming and business industry, is gradually moving forward through the use of wall-to-wall high-depth monitors, projectors, motion sensors, as well as the integration of other technologies. For example, Microsoft has a proof-of-concept system called the IllumiRoom, which uses a Kinect and projector to augment the space around a TV, creating an illusion that blurs the boundary between virtual and real. At the moment, virtual or augmented reality headsets (such as Microsoftʻs HoloLens or the Oculus Rift) are further along than full Holodeck-like rooms, but headset designs are not yet lightweight and comfortable enough to be used for long periods of time.
Fully immersive, augmented environments could be useful for handling stress and learning to manage anxiety or other mental disorders as well as providing physical therapy rooms in more serene settings. In addition, researchers at University of Illinois at Chicago’s virtual room called Cave Automatic Virtual Environment or CAVE2 (which lets fans walk around the Starship Enterprise) suggest their work could also be used for medical training.
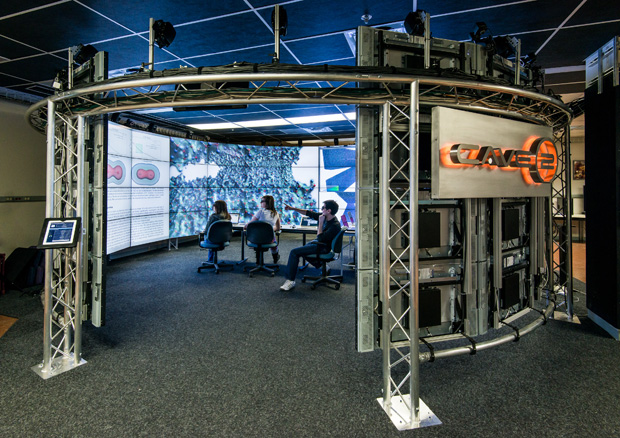
“As immersive and especially augmented reality technology improves in quality they have the potential to augment medical practice at all levels from primary care to surgery,” says CAVE2 designer Jason Leigh, now a computer science professor at the University of Hawaiʻi at Mānoa. Leigh, who adds he gets many of his ideas for projects watching Star Trek, says that such a system could superimpose medical imagery, such as three-dimensional MRI data, beside the patient that would issue warnings and suggestions to the doctor (like a GPS) in order to reduce errors.
His latest technology, the CyberCANOE (Cyber-enabled Collaboration Analysis Navigation and Observation Environment), will use cutting-edge LED displays to provide a seamless display, room-sized environment with richer and brighter colors, enabling him to simulate virtual realities even more realistically.

A World of New Technologies
A host of other technologies seen on Star Trek are currently in the early stages of development and may eventually have medical applications when—and if—fully manifested.
The universal translator in Star Trek was able to scan brain waves to interpret unknown languages into the user’s own language. In April 2014, Microsoft introduced Skype Translator, where a computerized voice and captions interprets spoken sentences in one language and translates them into another. Skype Translator Preview currently offers six voice languages and 50 messaging languages. Eventually, such a technology could prove useful in medical environments when caretakers and patients do not speak the same language.
Star Trek characters also had the benefit of replicators, devices that could materialize matter into any form requested, such as clothing or, more commonly, food and drink. In the last few decades, 3-D printers, which add layers of material to build three-dimensional objects, have become cheaper and more widespread. 3-D printers for food have also begun to take off, with everyone from NASA to gourmet chefs testing the waters. Someday we may enjoy instantaneous food deliveries and be able to order, for example, “Tea. Earl Gray. Hot.” as does Captain Picard.
The Star Trek fleet also used handheld touchscreens or “data slates” dubbed PADDs (Personal Access Display Devices). While the fictional rendition doesn’t look exactly like an iPad, characters used PADDS to play movies, make art, and record logs and audio, similar to how those in the medical fields use iPads and other tablets today to view and input data.
While we have realized or are making headway toward many Star Trek-like technologies likely once thought to be impossible to the show’s viewers, some features—teleportation, warp speed—still remain out of reach. Even so, the show’s impact on viewers’ imaginations has helped guide the development of many innovative medical technologies over the last decades, and it would appear we can look forward to more developments in the future.



