Before the novel coronavirus (COVID-19) started sweeping across the United States, it began on the coasts. The first known case was reported in a county just outside of Seattle, WA, with other cases quickly cropping up in California and in the greater New York City region. As the virus lingered on the periphery of the country, doctors and physicians working in inland, rural communities worried about what might happen if the virus hit their homes.
Fourteen percent of Americans live in rural areas, and rural health care centers face a multitude of challenges [1]. Rural America is home to many groups of ethnic minorities, who are at increased risk of getting more severe COVID-19. Compounding that are higher rates of cigarette smoking, high blood pressure, and obesity—all of which are more prevalent in rural populations. Getting tested for COVID-19 may also be challenging since rural centers are usually not well stocked with supplies. Such communities might lack the medical experts needed to deal with a new virus and the complex medical challenges it presents. Finally, rural Americans may be hours away from an emergency room, if they need to get ventilated or seek out more intensive care. In many ways, COVID-19 has laid bare the inequities of rural health in the United States.
However, despite the challenges that rural communities face from a health care perspective, they can also be incredibly nimble and flexible to adapt to a crisis if they have the resources to do so, says Carrie Henning-Smith, deputy director of University of Minnesota’s Rural Health Research Center. Across the USA, and in response to the coronavirus pandemic, many communities have strengthened their own capacities to deal with health crises by taking advantage of resources available to them. Nonprofits, campaigns, county health departments, and universities have also stepped in to help. Such efforts serve to aid rural health systems in the time of COVID-19—and possibly lead to long term change in rural health.
Tapping into the Medical Reserve Corps
In the wake of the September 11 attacks, the U.S. government established the Medical Reserve Corps (MRC), a national network of volunteers organized within local chapters who would improve the health and safety of their communities. MRCs drew on the expertise and experience of their members to help with community preparedness during natural disasters or health crises. To date, there are about 850 MRCs across the country and a total of 175,000 volunteers [2].
In mid-March, Jim Bristow, a former cardiologist and former director of the Department of Energy’s Joint Genome Institute, wanted Vashon Island in Washington to be prepared in case the virus moved into their community. Bristow’s wife came down with what seemed like coronavirus, but there was no testing available on the island to ensure that was the case. Residents on Vashon are about an hour away from the closest emergency room in Seattle, and can only get there by ferry. Bristow quickly got in touch with John Osborn, who leads the island’s MRC, to see what they can do. Together, they came up with a volunteer-based model to get residents of Vashon tested. Because many of the volunteers on the Vashon MRC are in the at-risk age category o contracting severe coronavirus, Bristow and Osborn opted for a drive through test site that allowed their residents to self-administer the test (Figure 1).

The clinical standard of a nasopharyngeal swab is invasive, and requires personnel to don extensive personal protective equipment (PPE), which was in short supply at the time Vashon started building their testing capacity. To bypass this requirement for extensive PPE, Vashon opted to conduct nasal swabs, which can be self-administered. Residents who go to the drive-through site first get their identity checked (Figure 2). A separate volunteer wearing goggles and a mask will hand them a q-tip so they can pull over and self-administer a nasal swab (Figure 3). (Recent studies show that the nasal swab is about as accurate as the nasopharyngeal swab [3].)

The lack of extensive PPE allows the model to be replicated in other places with well-trained volunteers, says Zach Miller, an infectious disease doctor and resident of Vashon who helped with the island’s coronavirus response. Bristow and Osborn have since brought their model to a number of tribes and communities in the Pacific Northwest. They have also publicized their model so that other communities can replicate it, on Vashon Be Prepared.

Elsewhere in the country, MRCs are being put to good use. Others are conducting temperature checks and extending care to homeless shelters in Columbus, OH. In New Mexico, the local MRC has also been helping set up medical facilities in the hard-hit Navajo Nation. With a shortage of medical facilities, the MRC, along with other university partners, have repurposed a high school gym into a temporary hospital [4].
Universities see rural communities as opportunities for education and partnerships
Back in 2003, Sanjeev Arora at the University of New Mexico launched a project to help rural health care providers take care of patients with hepatitis C. “People were dying from liver failure and liver problems because they couldn’t access specialists,” Arora says. With medical specialists centralized in major cities, they were in essence out of reach from the lower-income patients who don’t have the financial means to travel. Arora thought the way forward was to get specialized knowledge into the hands of rural providers.
Since then, Arora has launched Project Extension for Community Healthcare Outcomes (ECHO), an initiative that funnels specialized knowledge to health care workers in rural communities. They leverage videoconferencing via platforms like Zoom to share best practices with doctors across the country. At first, the specialists shared best practices over videoconference to health practitioners across the state of New Mexico. About a year and a half into the project, everyone with hepatitis C was getting access to treatment in the state of New Mexico. Project ECHO has since expanded nation-wide, and started training other universities with medical expertise to implement videoconferencing with rural hospitals in their respective states. More than 400 academic medical centers now are a part of Project ECHO’s model. Project ECHO also works internationally.
This year, ECHO has used its platform to dispense medical expertise on COVID-19. “Rural doctors all over the world don’t have access to the right knowledge at the right place at the right time,” Arora says. “Knowledge is constantly changing with public health practices like PPE or testing strategies, how to isolate or quarantine, how to manage treating patients at home, or how to manage patients in a hospital.” To date, he has trained more than 5000 health care professionals on handling COVID-19 in their communities. Every week, providers will log online to “ECHO clinics.” Around four or five medical specialists will also log on and provide expertise on managing and treating the coronavirus. These clinics, which run approximately one to two hours, aren’t traditional telemedicine where a specialist helps a patient. Rather, the specialists educate health care providers to enable collaborative learning. “We want to teach people to fish, not just give them the fish,” Arora says.
ECHO doesn’t directly bring resources or medical supplies into rural communities, but its model empowers communities to be better educated so they can make their own decisions. “What it does create is a greater awareness of how people can collaborate to make the best use of the resources,” explains Arora. This type of model can help rural communities even beyond the pandemic.
Elsewhere, universities have also begun partnering with rural communities in a more hands-on approach. This spring, the University of California at San Francisco (UCSF) launched an effort to provide testing to Bolinas, a small town in Marin County (Figure 4).

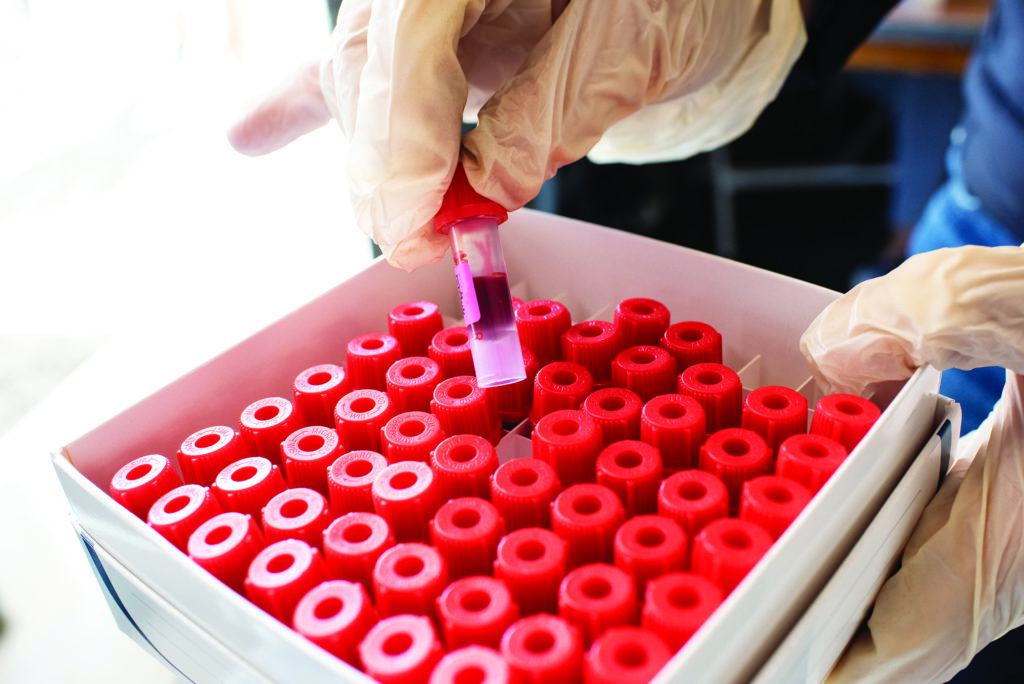
The goal was to understand transmission of COVID-19 in a rural community, and to get a sense of how to conduct widespread testing, explains Aenor Sawyer, a UCSF doctor and Bolinas resident [5]. This collaboration enabled the 1200 or so people in Bolinas to have access to both the test that would detect the virus if someone were symptomatic, and the antibody test to see if they had been infected (Figure 5), both at no cost to the residents (total project costs amounted to approximately US$340,00 beyond university expenses).

UCSF provided the medical supplies, as well as the ability to run the necessary laboratory tests (Figure 6). As of May 2020, this widespread testing showed that the community had no active infections, which might be largely due to residents adhering to the shelter in place orders, good hygiene, and social distancing practices. The complete testing of the community has not been replicated, however, because it’s not financially feasible, says Sawyer. UCSF’s involvement in Bolinas provides an example of how a university could partner with a rural community to conduct widespread testing, explains Bryan Greenhouse, an infectious disease researcher on this project at UCSF. The university partner is critical, explains Sawyer, although it’s less important for the medical center to be adjacent to the community they are serving. “Not everyone lives within an hour of a world-class medical center,” she says. “But this pandemic has shown us that we can have highly productive partnerships remotely.”
Team members have advised other rural communities in California and along the East Coast in implementing similar partnerships. For this to succeed in other communities, Sawyer says that there has to be broad buy in from residents who can help contribute volunteer hours, a partnership with the local and county agencies, an academic medical center partner, and a platform to communicate with others. And because rural communities have wide economic disparities, there must be a number of ways for people to access testing—whether it’s drivethrough testing, dropping tests off at people’s doorsteps, or going into their homes to administer tests.
Looking forward, rural communities know that while fighting and detecting active infections is important, there’s a long game. Because of COVID-19’s lingering effects, “we’re creating millions of long term chronic disease,” says Sawyer. “We need an organized approach to this pandemic starting at the highest level of our country, or we’re going to continue to see preventable cases of COVID-19.”
Osborn, of Vashon Island, also sees a looming mental health crisis associated with COVID-19. “There is a growing uneasiness about what is coming this fall and winter with COVID—exacerbated suicides, substance abuse morbidity and mortality, and domestic violence. Highest rates of suicide are often found in rural areas, notably the West,” he says. “With COVID sickness and death, social distancing, job loss, and economic collapse we are facing an ‘all hands on deck’ threat to our nation’s mental health.” And not only are rural communities lacking in medical supplies and testing, they are also scant in mental health resources and therapy. (For more on this, see “COVID-19 Is Straining Mental Health” in the July/August issue of IEEE Pulse.)
In late july, Osborn wrote a letter to Sen. Patty Murray of the Senate Committee on Health, Education, Labor & Pensions to fund MRCs to help build community resilience for the pandemic and beyond. The MRCs can not only be a vital force in containing COVID-19 cases, but also in strengthening access to mental health resources looking forward. But even as rural communities continue to tap into the resources of MRCs or universities, they still require support from one itinerant partner in both the short and long term: the federal government.
References
[1] Centers for Disease Control and Prevention, “Rural ncommunities.” Accessed: Aug. 23, 2020. [Online]. Available: https://www.cdc.gov/coronavirus/2019-ncov/ need-extra precautions/other-at-risk-populations/ruralcommunities. html
[2] Medical Reserve Corps, “About the Medical Reserve Corps.” Accessed: Aug. 23, 2020. [Online]. Available: https://mrc.hhs.gov/pageviewfldr/About
[3] H. Péré et al., “Nasal swab sampling for SARS-CoV-2: A convenient alternative in times of nasopharyngeal swab shortage,” J. Clin. Microbiol., vol. 58, no. 6, p. e00721-20, May 26, 2020, doi: 10.1128/JCM.00721-20.
[4] ASPR Blog, “Medical Reserve Corps volunteers’ hands felt at every level of the response to COVID-19.” Accessed: Aug. 23, 2020. [Online]. Available: https://www.phe.gov/ASPRBlog/Lists/ Posts/Post.aspx?List=f59454e5%2Da08d%2D4a13%2D9abe%2D0d31ef99f1af&ID=37 &Web=e1195e40%2Dc916%2D4c28%2Daa5a%2Dde2eda4302e4
[5] UCSF, “Bolinas COVID-19 testing effort detects no active infections.” Accessed: Aug. 23 2020. [Online]. Available: https://www.ucsf.edu/news/2020/05/417326/bolinascovid-19-testing-effort-detects-no-active-infections
Wudan Yan is an independent journalist and contributing writer to IEEE Pulse. She is based in Seattle, WA, USA.



