The Engineers in Scrubs (EiS) training program at the University of British Columbia, affiliated with the Faculty of Applied Science’s Biomedical Engineering Graduate (BMEG) Program, is not a typical graduate school course. Nor does it follow a traditional master’s course rubric that culminates with a tidy end-of-year project. Rather, the course is designed to push students to prototype innovative medical devices, encourage health care collaborations, and create an unprecedented interface between technology and health care to further medicine.
EiS was the brainchild of BMEG Director Dr. Antony Hodgson, who envisioned a program that merged medical engineering and health science, drawing from his past education at Harvard University and the Massachusetts Institute of Technology. Since the creation of the program in 2011, it has brought together diverse and talented engineers to identify unmet needs in clinical health care. The engineers accepted into EiS come from a wide range of disciplines but most have little clinical experience, which predisposes them to questioning decades-old procedures that one might take for granted. This naïveté is an advantage when touring medical facilities, where students often pepper the staff with questions such as: why patients are x-rayed multiple times or why don’t they use new computer- assisted technology to decrease operating room (OR) times? Inevitably, students are continually shocked when staff members answer, “We haven’t thought to look at it like that. Why don’t you fix it?” Tours such as these are just one part of the students’ introduction into the clinical setting and serve to highlight how biomedical engineers have applied their uniquely valuable outlook to aid in areas like cancer detection and cardiac surgery over the years.
Once EiS students grasp the potential value of their contribution to the clinical setting, clinicians are invited to pitch problems they currently face in their daily practice. It is here, in these MedTech Cafes, where engineering knowledge begins to merge with medical technology. It is up to the trainees to navigate the needs of the many disciplines, including radiology, orthopedic trauma, neurosurgery, and plastic surgery, and to gauge a project’s clinical importance and global impact. The pitched projects range from advanced ligament repair tools to alternative power drills in low-resource settings. After a set of problems are identified and the projects are chosen, teams are formed, and a tight feedback loop is established between clinicians and training programs, like the Uganda Sustainable Trauma Orthopaedic Program (USTOP). This creates an agile development process that will quickly bring novel solutions into the hospital setting.
At this point in the curriculum, it becomes clear to the students that EiS has tapped into something special. Students are given a chance to solve real-world engineering challenges from renowned clinicians, and clinicians have an engineering team dedicated to their needs. The clock starts now, and using the Stanford Biodesign Innovation Process [1] as a guide, students have four months of intense prototyping and iterating to prove their solution will be adopted.
From Blueprints to Three-Dimensional Printers
The Stanford Biodesign Innovation Process is fundamental to the education of an EiS trainee. This process is used extensively to identify the underlying need within each clinician’s problem statements and provides a solid framework for prototype development. The process is very human centered, implying that the teams develop their device with the user, the patient, and even the payee in mind. This human-centered approach also encourages “seeking inspiration from new places” [2], thereby allowing engineers to leverage their diverse backgrounds into the clinical setting to springboard the invention process. The Biodesign approach is invaluable and has proven its merit as it has been applied to many different projects with promising results. The Biodesign process also incorporates Toyota’s lean production method, an approach meant to eliminate wastefulness in the innovation process, ensuring fast device iterations, which, consequently, in EiS helps to keep clinicians engaged.
As an example of the design process, we can look at the Screw Cutter Project (see Figure 1), to see a team focused on trauma in Uganda, where road accidents kill four times as many people as in Canada [3]. The goal was to address inadequate surgical screw inventory in low-resource hospitals—an unassuming project that could potentially have a huge global impact. There are 5 million global traumatic fatalities yearly, and 90% of these occur in developing nations. With this number rising steadily, the health care systems of low-resource nations are the least prepared for the increasing demand for quality surgical care. To provide effective treatment for traumatic injuries, proper surgical consumables are required and the team aimed to develop a method to extend existing screw resources. By working with USTOP members, the screw inventory project was conceived in the EiS program to help clinicians provide a higher standard of surgical care when working with nonprofits—the forefront of care in the developing world.
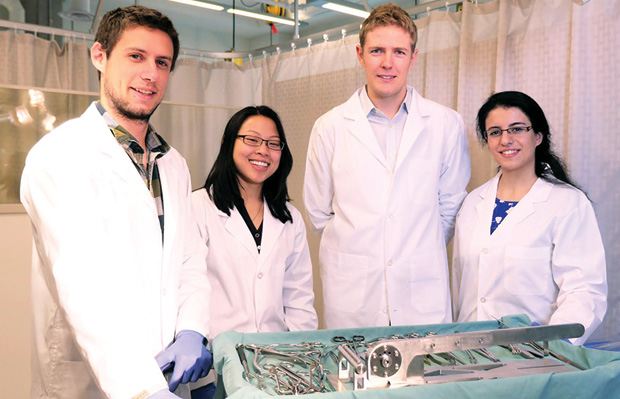
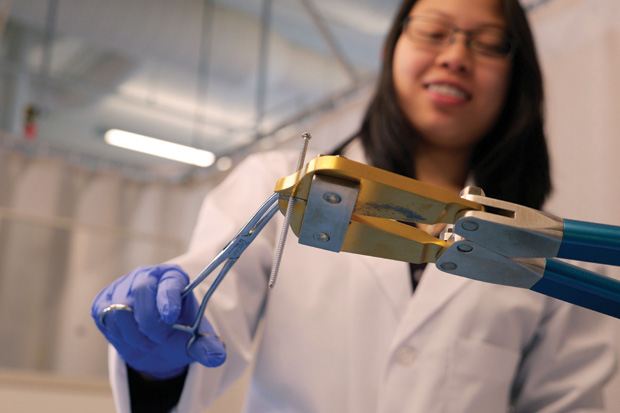
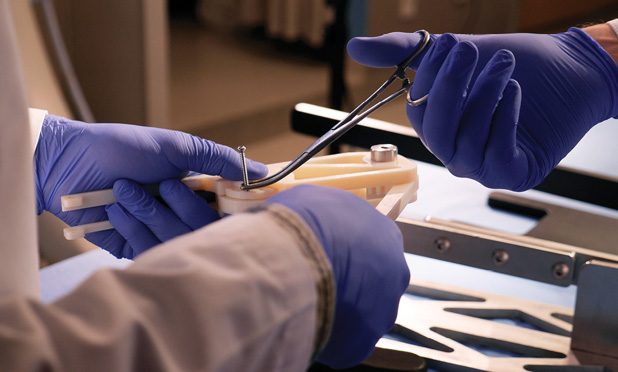
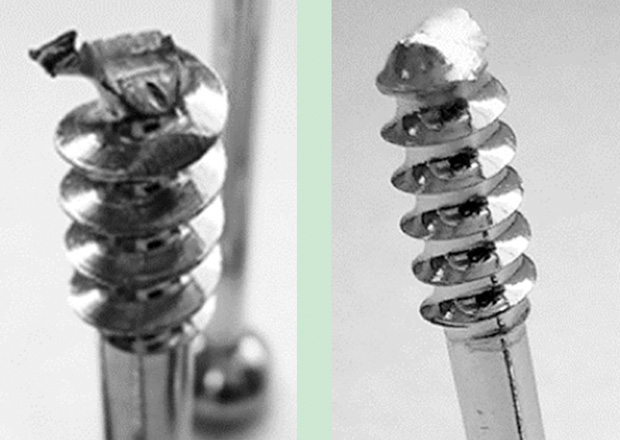
For several months, the Screw Cutter Project team (Figure 2) met weekly to discuss prototype design with the course instructor, Dr. David Wilson, as well as additional faculty. While the project moved quickly, the need to learn about current solutions being used was a major hurtle. The team discovered that screw inventory in Uganda was primarily donated by sources in developed countries; however, supply chains lacked a feedback loop that would allow proper inventory management. This resulted in a surplus of surgical screws that were not optimal for patients but, due to constraints, were used anyway. Using inappropriately sized screws to complete a surgery can cause serious postsurgical complications if it disrupts the tissues surrounding the fracture. Similarly, screws that are too short fail to engage cortical bone and cause improper fixation. Currently, the method used to produce appropriately sized surgical screws in the OR is a bolt cutter (Figure 3), similar to one you would find at a local hardware store, that chops screws to length. This method is known to damage screw threads and leave sharp ends that can damage nerves, soft tissue, and blood vessels (see Figures 4 and 5).
Working with clinical investigators, the team realized that the project was no longer a screw inventory problem, but the problem revolved around the screw-cutting device. This would require a new device that would warrant minimal training for health care professionals and that could easily integrate into their existing workflows. The proposed novel screw cutter, however, was unsettling to the clinical investigators since cutting surgically safe screws in the OR was virtually unheard of. However, the idea, while clinically unproven, has a rich history in other industries, and there are even commercial products available.
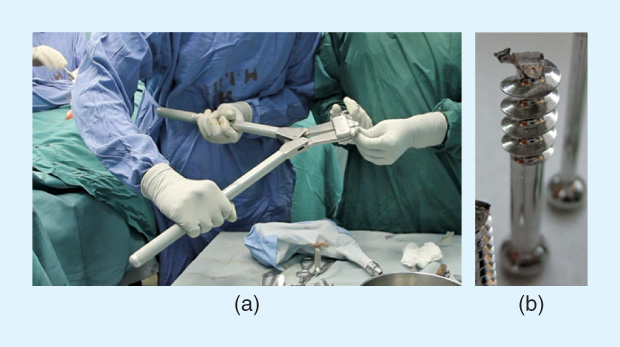
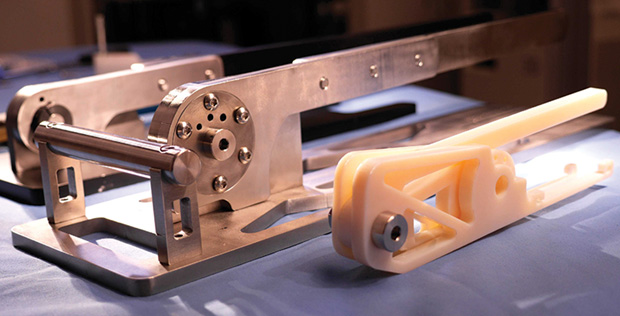
Subsequently, the students, with the clout of EiS, contacted a leader in surgical screws, Synthes Inc., and began experimenting. Using established techniques, they cut test screws using a combination of electric and manual shears and saws. In a preliminary presentation, it was shown that shearing provided the highest quality of cutting that didn’t sacrifice screw threads. The project progressed to using three-dimensional (3-D) printing, for an initial “look and feel” prototype to present to USTOP surgeons. This led to many sessions, tweaking the device’s ergonomic design to improve its applicability in the OR.
The team’s initial device was simple, and it used iterative prototyping that incorporated the feedback of mechanical engineers, as well as local and foreign surgeons, to advance the design. With the initial design approved by EiS and clinical collaborators, a full-scale prototype was constructed that had the capability to cut cortical, cancellous, and locking screws (see Figure 6). The prototype produced a flat cut at the tip of the screw and was accurate to the millimeter. However, in a feedback session with surgeons, they expressed the need for screws that were tapered, allowing easier screw insertion into the bone. Because of our program’s flexibility, students have the freedom to spend days interviewing stakeholders, or in this case, working in the British Columbia Cancer Agency machine shop. With assistance from a talented genomic scientist, Dr. Robin Coope, we developed a novel way to cut a tapered screw, which is currently being patented.

Not Just a School Project
The Screw Cutter Project is still ongoing; its first prototype was transported to Uganda in April 2014 as part of a usability study, which has provided invaluable feedback and validated the project’s need (see Figure 7). The device received high praise from local Ugandan surgeons and nurses, who used descriptions such as “genius” and “very applicable to our situation.” From their feedback, it was clear that the device had a strong potential for use in their ORs. A recurring feedback item from the study was that the device was not portable enough. This comment was reinforced by the important contextual fact that the device had to be carried over one kilometer from the sterilization center to the medical wards—something incomprehensible in North American health care. Based on this feedback, version 2 of the prototype was manufactured to be lighter and more simplified, which will aid in mass manufacturing. Using the most recent version, the team concluded a three-week usability study in May 2015 within Ugandan ORs and already has younger residents clamoring for it. The waiting list is growing because doctors understand the screw cutter device will enable them to perform higher-quality surgical procedures in situations where they lack proper screw inventories. One volunteer, a Canadian surgeon from McMaster University, even said, “Without your screw cutter, we wouldn’t have done the cases we did as well.”

It is not uncommon in EiS for groups to fully complete a working surgical prototype by the end of semester, but it is never expected. The purpose of the course is to learn the biodesign methodology and understand the process. The “minimal class-time” approach of the program allows students to research their project, learn new skills, and gain a better understanding of their place in medical technology culture. This program not only provides students with a deep appreciation for the needs and uses of technology in health care, but it also enables them to identify intuitive tools to aid clinicians. However, the EiS Program is not without its pitfalls. A project’s success is highly dependent on clinician interactions and the scope of the project. Smaller projects with a laser-like scope, such as the Screw Cutter Project and the Arbutus Medical’s Drill Cover Project, have found more success in terms of a completed product. Most students would agree that regardless of their final product, the networking opportunities provided within the clinical setting leaves plenty of room for future innovation with these disciplines. In conclusion, it is clear that institutions should continue championing the EiS program as it serves as a fantastic launch pad for fascinated young innovators who have some bold ideas of changing health care locally and worldwide.
Acknowledgments
The author acknowledges Andrew Meyer, Shalaleh Rismani, Vivian Chung, Nathan O’Hara, Dr. Piotr Blachut, Dr. Peter O’Brien, Dr. David Wilson, Dr. Machiel Van der Loos, and Dr. Robin Coope.
References
- P. G. Yock, S. Zenios, J. Makower, T. J. Brinton, T. M. Krummel, U. N. Kumar, C. Kurihara, F. T. J. Watkins, and L. Denend, Biodesign. Cambridge, U.K.: Cambridge Univ. Press, 2015.
- IDEO. (2009). [Online].
- C. Provost. (2011, May 11). The world’s most dangerous roads— Get the data. The Guardian. [Online].