The current gold standard for diagnosis of mental health disorders is a clinical interview in which the patient and clinician discuss the patient’s symptoms and history. This process is subjective and can be adversely affected by the patient’s memory difficulties and ability to articulate what he or she is experiencing. There is also a concern that patients may over- or underreport their symptoms depending upon real or perceived consequences for a diagnosis. Treatment of mental health disorders is similarly burdened by challenges in selecting an appropriate treatment and objectively monitoring response to treatment over time. In this article, we describe an approach that enables the use of objective psychophysiological indicators such as heart rate and skin sweating to augment current clinical practice for the diagnosis and treatment of mental health disorders. The ultimate goal of this work is to improve patient outcomes by increasing the ability to accurately diagnose, efficiently treat, and effectively monitor the response to treatment over time.
Problem Space
Mental health disorders are a leading cause of disability in the United States and across the globe [1], [2]. Mental health disorders are diagnosed via a structured clinical interview in which patients relay information about their symptoms and level of psychological functioning to the clinician. To be diagnosed with a mental health disorder, such as major depressive disorder (MDD) or posttraumatic stress disorder (PTSD), patients must exhibit a certain number of symptoms within the diagnostic criteria for each disorder listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [3].
One of the inherent challenges in this process is that the clinician must rely upon what the patient reports and what is observed in the clinical interview. Patients may have difficulty describing their current symptoms and past symptoms for many reasons, including memory difficulties, the presence of coexisting medical or mental health conditions, and the fact that patients more accurately report symptoms that are current or recent. Additionally, there is a risk that patients may under- or overreport their symptoms depending upon real or perceived consequences for a mental health disorder diagnosis.
An additional challenge in accurately diagnosing a mental health disorder is that many mental health disorders are comorbid (i.e., patients may have anxiety in addition to depression) and many symptoms overlap across disorders. For example, PTSD and MDD often occur together. Not all patients will exhibit every symptom listed as diagnostic criteria in the DSM-5, and there is considerable variability across people in the manifestation of symptoms and symptom severity. To further complicate diagnostics, mental health disorders often coexist with other medical conditions such as diabetes, hypertension, and obesity, which also may have symptoms that overlap with or contribute to symptoms of mental health disorders.
It is clear that a more objective means of diagnosing mental health disorders is needed. Objective means include direct or indirect measurement of the biological systems that are not functioning normally in patients with mental health disorders. There are a number of technologies that have shown potential for distinguishing among those with and without mental health disorders, including functional magnetic resonance imaging (fMRI), positron emission tomography (PET), and psychophysiological measures such as skin conductance (SC), electrocardiogram (ECG), and facial electromyography. Although these approaches have demonstrated promise for distinguishing among those with and without mental health disorders, they currently are not integrated into clinical workflows.
For imaging technologies, one of the primary barriers to integration into a clinical setting is cost; technologies such as PET and fMRI are expensive to acquire and require expertise to use and interpret the findings. Psychophysiological measures are less expensive to acquire, but most systems require technical expertise to acquire, analyze, and interpret the data. None of these approaches is perfect; all have some percentage of false positives and false negatives that can result in diagnoses in those without a disorder and missing diagnoses in those who do have a disorder. Although no single technology is perfect, the use of several approaches and technologies will provide better discrimination than any approach used alone.
In addition to the challenges involved in correctly diagnosing mental health disorders, clinicians also are challenged with correctly matching treatments to individual patients. Not all patients will respond identically to a treatment. Some patients may respond best to a pharmaceutical treatment, whereas others may respond best to cognitive behavioral therapy, and some may respond best to a combination of these. Clinicians currently have no way of objectively identifying these groups of patients prior to starting a therapeutic regimen. A means for improving the clinical decision process for ascertaining which therapeutics patients will respond to prior to starting treatment is needed.
Our Approach
To address these challenges, we have developed an innovative approach that utilizes objective multimodal psychophysiological measures and nonidiographic stimuli. Psychophysiological measures such as SC (skin sweating), heart rate, blood pressure, and pupil diameter directly and indirectly measure the nervous system and other systems in the context of observed behaviors (e.g., how a person reacts to a stimulus). Nonidiographic stimuli are emotionally evocative and arousing but not specific to a person’s individual experience. At Draper, we have conducted two small-scale studies using this approach, one focused on PTSD and one focused on MDD.

Much of the work that has been done examining psychophysiological responses in those with and without PTSD has utilized stimuli specific to an individual’s trauma. This approach generally results in strong physiological responses and the ability to distinguish among those with and without PTSD. However, this approach requires time and effort to elicit information about the trauma and creation of the stimuli to be used during data collection. We chose to examine the utility of nonidiographic stimuli in our study to ascertain whether we could distinguish among those with and without trauma and PTSD with a goal of developing less specific stimuli that could be used more easily and efficiently in a point-of-care setting (Figure 1).
In our PTSD study, we examined differences among those with PTSD, those who had experienced trauma but did not have PTSD, and matched controls who had not experienced trauma and did not have PTSD. We recruited participants in the areas of Boston, Massachusetts, and Tampa, Florida. Of the 58 male veterans who participated, 19 were in the no trauma/no PTSD diagnosis group, 23 were in the trauma exposed/no PTSD diagnosis group, and 16 were in the PTSD diagnosis group. The participants completed a data collection protocol in which they were exposed to emotionally evocative virtual reality (VR) audiovisual stimuli while their physiological activity was recorded. We collected SC and ECG from which we derived interbeat interval (IBI), respiration, and pulse photoplethysmography (PPG).
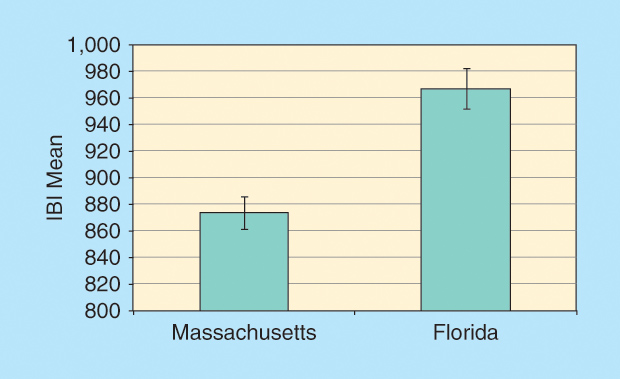
One of the most interesting findings in this study was a significant difference among our data collection sites in IBI. These data are depicted in Figure 2. The participants in Tampa had a longer average baseline IBI (lower heart rate) than the participants in Boston. This difference was not due to known differences in the participants, equipment, or methodologies and emphasizes the need to assess and properly account for geographic differences in future work. We envision a suite of algorithms tailored to geographic, individual, and disorder differences. One very important strategy in the diagnostic paradigm we envision is that an individual patient’s responses be compared with his or her own baseline in terms of monitoring treatment effectiveness.
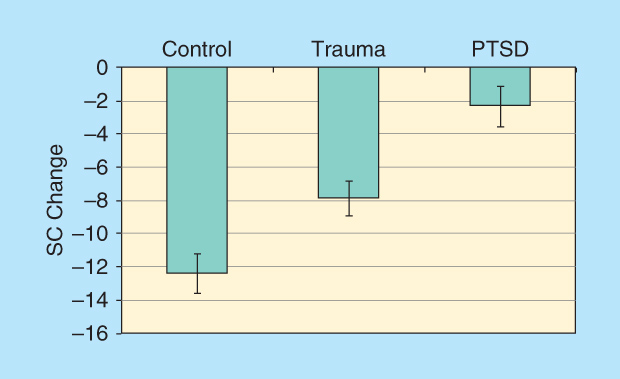
One of the primary findings in this PTSD study was a difference among the three groups in their SC reactivity in response to the VR stimuli. All participants watched two VR videos (a city patrol scenario and a Humvee driving scenario) in which stimuli of increasing intensity were presented. Half of the participants watched the patrol video first, and the other half watched the Humvee video first. We computed difference scores to assess change across the two videos. These difference scores were computed such that a negative value indicates a decrease in reactivity from video 1 to video 2. These data are presented graphically in Figure 3. One can see that those in the PTSD group showed similar arousal across the two videos as demonstrated by small change scores, whereas those in the control group showed less arousal during video 2 as compared to video 1. This finding indicates that those in the control group habituated across the two videos, whereas those in the PTSD group remained aroused and did not habituate. Habituation is a well-known phenomenon in which psychophysiological responses diminish over time in response to repeated stimulus presentation.
In our depression study, we recruited 25 participants with MDD and 25 control participants. Similar to our PTSD study, we exposed participants to emotionally evocative audiovisual stimuli while their physiological reactivity was recorded. In addition to SC, ECG, respiration, and PPG, we also used an eye tracker to record pupil diameter from each eye.
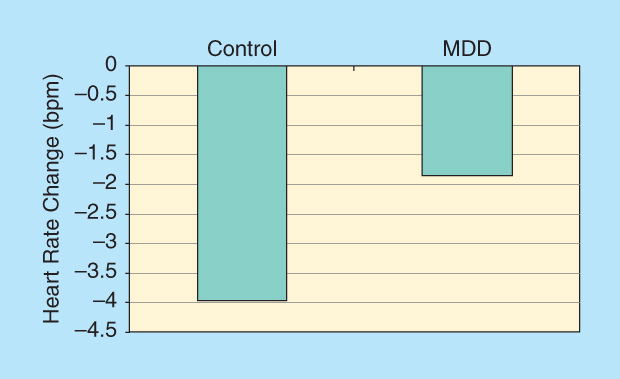
We examined change from baseline to that seen during viewing of emotionally evocative movies. Heart rate results are shown in Figure 4. This graphic demonstrates that heart rate decrease was significantly greater in control individuals as compared to those with MDD. These results indicate that those with MDD have a blunted reaction to specific types of stimuli and are not as physiologically responsive as those without MDD.
Path Forward
There is increasing interest from the National Institutes of Mental Health to develop innovative ways of understanding and diagnosing mental disorders informed by research on genetics, neuroscience, and behavior that could complement or even challenge traditional diagnostic categories. The approach we describe here is intended to leverage a century of neuroscience, psychological, and physiological research to redefine the way that mental health care is delivered. We envision a data collection and analysis system that can be used in point-of-care settings to assist clinicians in diagnosis, treatment selection, and treatment monitoring for a variety of mental health disorders. The results from our small proof-of-concept studies are promising and suggest the utility of this approach for assisting with diagnosis. A significant funding investment is needed to perform the work necessary to move this approach closer to deployment in point-of-care settings.
Further work is needed in larger, more heterogeneous samples to assess the robustness and generalizability of this approach. The participants in our samples were relatively free of comorbid disorders. Given that many mental health disorders are comorbid with one another, it will be important to assess this approach in samples where several disorders are comorbid. Additionally, as noted previously, it is important to assess and account for geographic differences. The participants in our samples also were relatively free of medications. Given that physiological activity can be affected by medications, it will be important to evaluate this approach in samples that vary in medication type and dosage.
Work also is needed to assess this approach in treatment studies to begin to understand how treatments can be better matched to individuals. We have done some preliminary work assessing differences in physiological reactivity pre- and post-treatment for PTSD [4], and the results are promising and suggest that these objective measures can be used to assess response to treatment.
Although this work is in its infancy, the promising results speak to the value of this approach and the need for additional work. The continued development of this approach and widespread deployment to point-of-care settings after proper testing and evaluation will help ensure that patients are efficiently diagnosed and treated, resulting in improved outcomes and quality of life for all.
References
- World Health Organization. (2015, July 1) The global burden of disease: 2000-2012 estimates. [Online].
- H. A. Whiteford, L. Degenhardt, J. Rehm, A. J. Baxter, A. J. Ferrari, H. E. Erskine, F. J. Charlson, R. E. Norman, A. D. Flaxman, N. Johns, R. Burstein, C. J. L. Murray, and T. Vos, “Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010,” Lancet, vol. 382, no. 9904, pp. 1575–1586, Nov. 2013.
- American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, D.C.: American Psychiatric Association, 2013.
- A. K. Webb, K. E. Kip, A. B. Jin, and E. J. Hickling, “Use of psychophysiological measures in the assessment of treatment response for PTSD,” Poster presented at the annual meeting of the International Society for Traumatic Stress Studies, Nov. 2015.



