As the current pandemic continues to affect populations around the globe, the search for a viable vaccine for coronavirus-2019 (COVID-19) continues. However, rather than constantly scrambling to generate a vaccine after an outbreak happens, some researchers are working on what they see as a better approach: developing a broad-acting “pan-coronavirus” vaccine that provides protection from any coronavirus, present or future.
Research groups at Duke’s Human Vaccine Institute (DHVI) and at Entos Pharmaceuticals, Inc. of Edmonton, AB, Canada, are two of the teams setting their sights on a pan-coronavirus vaccine. In both cases, the researchers are capitalizing on those conserved (i.e., shared) features of all coronaviruses so that the body’s immune system immediately recognizes the current severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (as well as any member of the coronavirus family) as a pathogen, and mounts a strong defense.
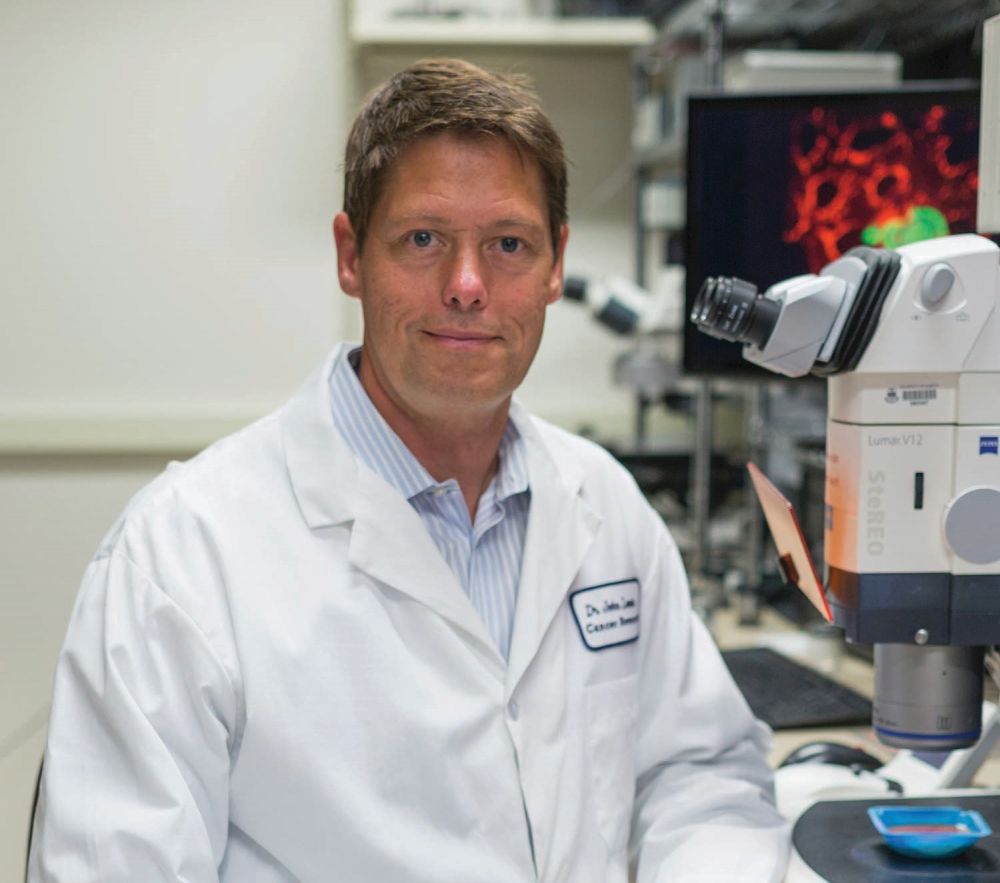
“If you think of the coronavirus family as a tree, and SARS-CoV-2 and the other coronaviruses as branches off that tree, almost all of the virus projects under way now are going after the one branch. We’re hoping with this pan-coronavirus vaccine to go after the central trunk,” said Thomas Denny (Figure 1), chief executive of DHVI in Durham, NC [1].
Duke approach
At Duke, the researchers started their work on a pan-coronavirus vaccine by gathering genetic sequences from as many types of coronavirus as possible, Denny said. They searched the scientific literature for genetic details that have already been deciphered from known coronaviruses, including SARS-CoV-1, which was responsible for the 2002–2003 SARS epidemic, and Middle East Respiratory Syndrome coronavirus (MERS-CoV), which has spread from the Arabian Peninsula since it was first reported in 2012. They are also sequencing seasonal coronaviruses, such as the common cold, and SARS-COV-2 from a range of people to determine whether it has variation or is stable.

“Once you get all that material together and double-check it to make sure you’re not getting errors in what you’re bringing in, then you can turn loose the high-speed computers to try to find these highly conserved regions,” Denny said.
The Duke group is working with investigators at Los Alamos National Laboratories in New Mexico and at the University of North Carolina-Chapel Hill. The Los Alamos group has already identified highly conserved regions, designed recombinant immunogens based on the amino acids coded by those regions, and is preparing to test the synthesized immunogens in animal models to ensure that the immune system launches a sufficient antibody response (Figure 2). At UNC-Chapel Hill, the research team of Ralph Baric, Ph.D., of the departments of microbiology and immunology, and epidemiology, is surveying potential coronaviruses that might emerge in the next outbreaks. “It is critically important to have a pan-coronavirus vaccine ‘on the shelf’ for the next vaccine to avoid societal shut-down when a new outbreak occurs,” noted Barton Haynes, director of DHVI and overall leader of the pan-coronavirus project.

Candidate immunogens with good immune-response tests will move forward to tests in nonhuman primate models with the ultimate goal of phase 1 human clinical trials.
Unusually, Duke’s vaccine institute has its own Good Manufacturing Practice (GMP) Production Facility to manufacture phase 1 material, and will also soon be adding fill-finish (product formulation and packaging) capability. The GMP facility will grow candidate immunogens in a cell line to determine their practicality for vaccine development. “A lot of times what happens is scientists put in years of work to develop a drug or a product like this that looks wonderful, but when they hand it off to a product-development team to try to make it so it can go into a trial, the product-development team comes back and says they can’t manufacture it: perhaps the cell line doesn’t express the immunogen in sufficiently high quantities, or the cell line expresses the immunogen with glycosylation patterns that don’t make it a good immunogen for humans,” Denny said. “Our model at Duke is to embed our product-development team alongside of our discovery team, so that as we get down the line on a slate of potential candidate immunogens, our product-development team has already had enough involvement that they can say, yes, that’s manufacturable.” He added, “That’s the niche that we are bringing to this work.”
The Human Vaccine Institute has several large, concurrent projects in the works [2], including a messenger ribonucleic acid (mRNA) vaccine and mRNA-delivered antibody therapies to fight SARS-CoV-2, and a pan-influenza vaccine, and has been successful in isolating cross-reactive coronavirus antibodies that are being used as templates for vaccine design. “We’re here to prove a concept, show safety, immunogenicity and hopefully efficacy,” Denny said, “and then we will hand it off to the companies that can make this at a massive scale.”
Entos approach
Entos opted to take a different route and is developing a vaccine that can deliver the directions—via deoxyribonucleic acid (DNA)—for encoding selected coronavirus proteins, or epitopes, that are highly conserved within the coronavirus family. These epitopes serve as antigens, which in turn, prompt the body to begin producing coronavirus-fighting antibodies and confer long-term immunity.
As with other DNA-delivery projects, one of the most challenging tasks is getting intact DNA to the cells, but Entos had an ace in the hole. It had already developed its innovative Fusogenix platform [3], a proteo-lipid nanoparticle vehicle that is able to transport a wide variety of nucleic acids, including gene therapies and plasmid DNA, directly to the cytosol of target cells, according to John D. Lewis, Ph.D., founder and chief executive officer of Entos, and researcher at the University of Alberta in Edmonton, AB, Canada (Figure 3). “With this platform, we can scale-ably manufacture nanoparticles, and these nanoparticles can effectively deliver DNA without any associated toxicity,” he said. In addition, Entos’s nanoparticles have a large enough cargo capacity to hold DNA directions for making multiple antigens, even full-length proteins.
To choose conserved epitopes capable of providing a robust immune response across coronaviruses, Entos has employed a rapid prototyping process to evaluate antigens developed in-house as well as those provided by collaborators such as informatics and immunology biotechnology company Epivax of Providence, RI (Figure 4). This process has yielded two dozen promising epitope combinations, with lead candidates being the full-length spike protein (S-protein), the full-length nucleocapsid protein (N-protein), and a combination of the two [4]. Tests in animal models have shown that DNA vaccine formulations of the S-protein and of the N-protein are each effective after a single dose.
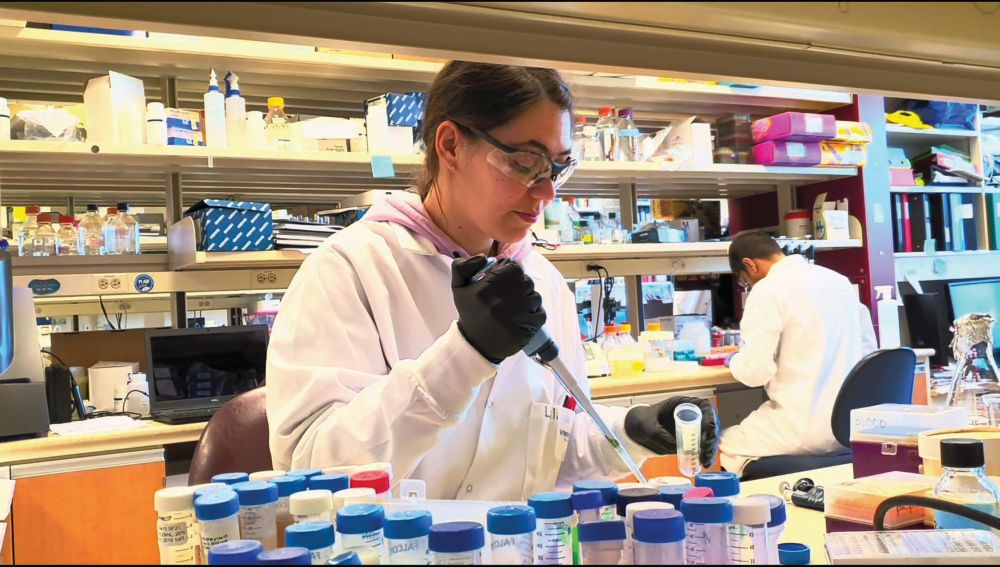
Lewis is especially excited about the potential of the N-protein option. The S-protein has received considerable attention from research groups developing a vaccine specifically against SARS-CoV-2, he said, but it is not as well-conserved across the coronavirus family as is the N-protein. Lewis remarked, “So from a pan-coronavirus-vaccine standpoint, N-protein was compelling because we knew it could produce strong T-cell (immune) responses. In fact, if you look at the original SARS-CoV-1 patients, even now they still have T-cells floating around that recognize the SARS N-protein, which means that it could be the basis of both a long-term T-cell immunity, as well as potentially cross-immunity with other coronaviruses.”
Through the fall, Entos will be conducting tests of the vaccines’ effectiveness against a variety of coronaviruses in animal models. In addition, they have already completed the preclinical work on the S- and N-proteins, and is beginning adaptive phase 1/phase 2 design clinical trials. “For the phase 1 or safety part, we are recruiting 74 patients, and as soon as the safety signal looks good in those patients, we’ll move into the phase 2 portion that will include up to 600 patients,” Lewis said. He hopes to have that wrapped up by the end of the year and start phase 3 trials as early as the end of this year.
The progress on the pan-coronavirus vaccine, as well as the vaccines and other approaches under way to specifically designed to fight SARS-CoV-1, are part of a greater picture, Lewis noted. “It’s really been an unprecedented collaborative and data-sharing effort by the scientific community to be able to make rapid progress.” Looking to the future, he added, “I’m looking forward to this becoming much more the norm.”
References
- Duke Human Vaccine Institute, “Influenza.” Accessed: Aug. 1, 2020. [Online]. Available: https://dhvi.duke.edu/diseases-research/priority-pathogens/influenza
- G. D. Sempowski, K. O. Saunders, P. Acharya, K. J. Wiehe, and B. F. Haynes, “Pandemic preparedness: Developing vaccines and therapeutic antibodies for COVID-19,” Cell, vol. 181, Jun. 25, 2020. Accessed: Aug. 1, 2020. [Online]. Available: https://doi.org/10.1016/j.cell.2020.05.041
- Entos Pharmaceuticals, “The challenge: Effective drug delivery.” Accessed: Aug. 1, 2020. [Online]. Available: https://www.entospharma.com/fusogenix
- Entos Pharmaceuticals, “Entos announces selection of lead DNA vaccine candidates for COVID-19 and a $4.2M award to move forward with phase I/II human trials.” Accessed: Aug. 1, 2020. [Online]. Available: https://www.entospharma.com/news/entos-announces-selection-of-lead-dna-vaccine-candidates-for-covid-19-and-a-4-2m-award-to-move-forward-with-phase-i-ii-human-trials