In Italy, biomechanics research and the analysis of human and animal movement have had a very long history, beginning with the exceptional pioneering work of Leonardo da Vinci. In 1489, da Vinci began investigating human anatomy, including an examination of human tendons, muscles, and the skeletal system. He continued this line of inquiry later in life, identifying what he called “the four powers—movement, weight, force, and percussion”—and how he thought they worked in the human body. His approach, by the way, was very modern—analyzing nature through anatomy, developing models for interpretation, and transferring this knowledge to bio-inspired machines.
With a similar approach in recent decades, a great deal of research has been carried out in the field of movement analysis, functional evaluation of human performance, rehabilitation engineering, and biomechanics. This field combines knowledge, concepts, and methods from across many biomedical engineering disciplines (e.g., biomechanics, innovative technologies and materials, computational modeling, and robotics as well as neuroscience, physiology and clinical applications) with the aim of developing new devices and methods for the measurement and analysis of complex sensorimotor performance. The ultimate goal is the enhancement of performance and the diagnosis, treatment, and rehabilitation of motor disorders and disabilities related to various pathologies. In this article, we provide an overview of related research activities in Italy.
Methods and Technologies for Movement Analysis
Since the 1970s, the Politecnico di Milano (Polytechnic University of Milan) has had a long tradition in the research field of movement analysis, particularly at the Centro di Bioingegneria (jointly sponsored with the Don Gnocchi Foundation), which is aimed at developing innovative technologies and computational modeling in cooperation with medical doctors to meet the emerging needs in clinical practice. The center is where an analog–digital hybrid computer was developed that processes signals from a piezoelectric force plate, obtaining in real time a single image of the vector diagrams of gait (also butterfly diagrams or Pedotti’s diagrams). This diagram, now obtainable by a normal personal computer and widely used in gait analysis labs, opened the pathway to the development of more advanced systems for motion capture.
![FIGURE 1 - Multifactor analysis of gait: (a) three-dimensional (3-D) IR motion capture [10], (b) a force plate providing butterfly diagrams [11], (c) a multimodal 3-D representation, and (d) a wireless surface electromyography (SEMG)](https://www.embs.org/wp-content/uploads/2015/07/fig16.jpg)
The very large-scale integration (VLSI) technology allowed Ferrigno and Pedotti to design and implement the first prototype of the elaboratore di immagini televisive (ELITE) system, obtaining a high level of accuracy and reliability in the determination of marker position (Figure 1). The system was patented and transferred to a start-up, which has become one of the leaders in this sector worldwide.
SEMG has also been developed for basic measurements obtained under static conditions (e.g., nerve conduction studies and analysis of motor unit recruitment and fatigue) in terms of hardware and software for data processing mainly at the Politecnico di Turin, Italy.
Complexity and Motor Learning
Common in the animal kingdom as well as in our daily activities, movement is not usually associated with the concept of computational complexity and intelligence. In reality, even an apparently simple motor performance involves a complex coordination of neuromuscular activities required to reach a multiparametric optimization, including precision, equilibrium, speed, environment interaction, and energy minimization. To achieve such goals, our brain processes information about the internal state of the body (proprioceptive feedback) and the external world (visual, tactile, vestibular, and auditory feedback) according to programs (motor strategies) that are acquired genetically or by learning.
![FIGURE 2 - Studies on neuromotor strategies and motor learning: (a) the results from high-level classical dancers [13] and (b) experiments in microgravity.](https://www.embs.org/wp-content/uploads/2015/07/fig26.jpg)
Computational modeling combined with quantitative analysis of movement, brain functional imaging, and genomics could answer new questions about the role of learning versus genetic predisposition in skilled motor performances. For this purpose, selected motor tasks involving multijoint coordination, which belong to the repertoire of ordinary movements, have been investigated to compare different motor strategies adopted by a population of naïve subjects with a population of high-level performers (i.e., classical dancers and Olympic gymnasts). Similar studies have also been performed on astronauts during long-term missions on the Mir Space Station and the International Space Station (ISS), where a specially developed ELITE system is still present, demonstrating that learning processes make it possible to build up new motor programs with important consequences for designing new prostheses and rehabilitation techniques (Figure 2).
Computational Modeling of Organ Motion and Body Segments
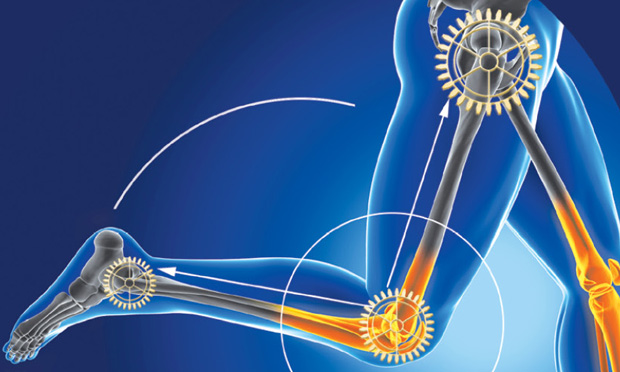
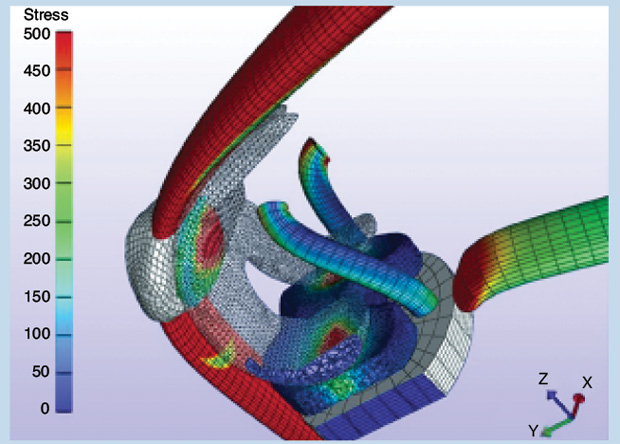
Mathematical models and numerical simulations of organ motion and the body segments under sensorimotor control have been developed for different conditions and performances in healthy subjects and patients with motor disabilities such as muscular dystrophies, cerebral palsy, Parkinson’s disease [3], orthopedic problems, Down syndrome, and stroke. Posture, equilibrium, gait, and motor control are currently being studied in these patients throughout a multifactorial approach, including not only biomechanics (e.g., statics, kinematics, dynamics, and kinetics) but also functional signaling and imaging [e.g., electromyography, electroencephalography, near-infrared spectroscopy, and functional magnetic resonance imaging (fMRI)]. Recent developments in this field are, therefore, oriented toward a strict combination of functional assessment and imaging techniques to define a more detailed modeling of both body segments and soft tissues. An example of this trend is a dynamic model of the musculoskeletal system, in which the geometry of bones, joints, and muscle attachments was derived from magnetic resonance imaging (MRI) [4] (Figure 3). These kinds of models are useful for computer planning in functional surgery and customization of endoprosthesis.
It is, however, accepted that the research in biomechanics has enlarged its prospects, including motion not only from organs and body segments but also from the molecular levels to understand the behavior at the organ or tissue levels.
Theoretical and experimental studies of the mechanics of proteins, the molecular mechanisms, and mechanotransduction in living cells are the basis of molecular and cellular biomechanics. Indeed, forces and stresses transmitted via individual proteins to the cytoskeleton can cause structural changes for initiating and controlling cell signaling pathways. The response of cells to mechanical signals influences tissue development and behavior. The mechanical characterization of tissues helps in determining the main features to describe, understand, and predict their behavior. Experimental studies have been conducted on tendons, ligaments, cartilage, bones, plantar soft tissues, cardiac valves, vessels, cornea, teeth, and vertebrae. These studies are often accompanied or followed by computer models aimed to describe the biomechanical behavior and predict the interaction of the degenerated or diseased tissue with a medical device implanted to restore tissue functionality.
![FIGURE 4 - (a) A planar X-ray image of the thoracolumbar spine of a scoliotic patient, (b) a finite-element model based on the radiographic image in which pedicle screws (in blue) are implanted to simulate the surgical correction of the spinal deformity, and (c) the experimental setup to test the strength of the pedicle screws and fixation rods used in the deformity correction surgery. (More information can be found in [14] and [15].)](https://www.embs.org/wp-content/uploads/2015/07/fig45.jpg)
Figure 4 shows a biomechanical study partially carried out at the Laboratory of Biological Structure Mechanics of the Politecnico di Milano established in 2000 by Prof. Riccardo Pietrabissa, Prof. Roberto Contro, and Prof. Roberto Fumero. The study addressed adolescent idiopathic scoliosis, in which planar radiographic information in combination with a patient-specific computer model was used to select the optimal surgical treatment to achieve a good and safe correction of the spinal deformity. The modeling approach can be coupled with experimental testing (e.g., with cadaveric specimens or standardized surrogates) to ensure that the biomechanical predictions of the model are reliable.
Bones have attracted a lot of attention since the beginning of biomechanics studies, and the Università di Bologna, together with The Rizzoli Orthopedic Institute (Istituto Ortopedico Rizzoli) with Prof. Luca Cristofolini and Prof. Marco Viceconti, has invested much effort in understanding the bone shape–function relationship. In vitro tests accompanied by anatomical considerations show how the proximal femur is optimized to resist the cyclic loads during daily activities (Figure 5); these studies highlight how the robust optimization of the femur resists a force applied in a range of directions during daily life and, at the same time, is able to absorb a large amount of energy associated with an impact in a completely different direction during a sideways fall. The diaphysis of the tibia is shaped to uniformly distribute stresses during locomotion. Similarly, the shape and microstructural arrangement of the body of the thoracolumbar vertebrae is optimized to resist axial loads.
![FIGURE 5 - An in vitro test on a human femur. A paraphysiological loading scenario was simulated to induce spontaneous fractures. (More information can be found in [16].)](https://www.embs.org/wp-content/uploads/2015/07/fig53.jpg)
Other examples of innovative research in the field of biomechanics at a tissue level can be found in the cardiovascular field, such as the hemodynamics generated in cardiovascular surgery or in the presence of endovascular prostheses and devices. For examples of research in this area, we refer the reader to the contributions in this issue of IEEE Pulse related to the clinical interpretation of mathematical models, “A Model of Health“ by Alberto Redaelli (on page 27) and “A Model Approach” by Claudio Cobelli and Mauro Ursino (on page 33).
The design and evaluation of medical devices are strictly related to the research activity in biomechanics. Indeed, the characterization at the level of the material and the mechanical evaluation of stresses and strain in the device have an importance for the life and behavior of the device itself. When studying or designing a device, such as a spinal fixator, an orthodontic brace, or an endovascular stent, the relationship between the structure, the material, and the surrounding tissue plays an important role. Materials can have ductile properties like stainless steel, cobalt-chrome, and titanium alloys or superelastic properties such as shape memory alloys like nickel-titanium alloys or Nitinol. It is well known that a stent, for example, can properly expand with a polymeric balloon if made of a ductile material and a particular design, but it can also self-expand with a superelastic material with a design that is completely different from stents used with an angioplasty balloon. The materials properties determine the fatigue life of the device when implanted in an environment exerting cycling loads such as in the stents used to treat lower-limb pathologies (Figure 6).
![FIGURE 6 - An evaluation of the risk of stent rupture in cases of peripheral vascular angioplasty. This study used data from in vitro experiments on real stents and precomputed numerical simulations of diverse clinical cases personalized based on the patient conditions and suggest possible risks of stent rupture. Models such as these are, therefore, of great utility for physicians before a surgical operation as well as for engineers working in the biomedical industry. (For more information, see [17] and [18].)](https://www.embs.org/wp-content/uploads/2015/07/fig62.jpg)
Robot-Based NEurorehabilitation
The bioengineering community in Italy is very active in the emerging areas of rehabilitation robotics and bionic prosthetics, with leading research groups based at the BioRobotics Institute of the Scuola Superiore Sant’Anna in Pisa, the Campus Bio-Medico Università di Roma, the Italian Institute of Technology in Genova, the Politecnico di Milan, and with other active groups in Bologna, Padua, and more. Italy also features a very high number of clinical centers when compared to other European countries, currently using rehabilitation robots for their routine services and/or clinical trials. This was one of the key success factors of the 2010 IEEE Robotics and Automation Society/EMBS BioRob conference, which was organized in Rome (with one of the coauthors of this article, Eugenio Guglielmelli, serving as the general chair) with more than 500 attendees from more than 40 countries.
Rehabilitation robots are systems that provide therapy for persons seeking to recover their physical, social, communication, or cognitive function and/or that assist persons who have a chronic disability to accomplish activities of daily living [5]. Rehabilitation robotics has experienced a significant growth in recent decades, with an increasing number of systems becoming commercially available and double-digit market growth estimated in the short to medium term. Apart from the performance, quality, and appropriateness of the robotic systems being developed, there are two main drivers concurring in such a success: increasing acceptance by clinical caregivers and a growing demand for effective rehabilitative therapies induced by the aging population in most developed countries.
Rehabilitation therapy robots offer the advantage of delivering high-intensity and task-oriented training using interactive scenarios that help the active involvement of patients. Moreover, rehabilitation robots provide a measure of patient performance that, in turn, enables the adoption of quantitative kinematic and dynamic metrics, such as those developed in a long-lasting joint research effort involving the Newman Lab [N. Hogan and H.I. Krebs at the Department of Mechanical Engineering, Massachusetts Institute of Technology (MIT)] and the Campus Bio-Medico Università di Roma (UCBM) in Italy [6] or the collaboration between the Scuola Superiore Sant’Anna and Fondazione Maugeri in Veruno [7].
Several Italian research teams are currently working on important research topics such as the following:
- Integration of therapy robots with neuroimaging and neuromodulation systems to unveil how rehabilitation therapy induces brain reorganization, such as in chronic stroke patients. For example, a passive fMRI-compatible manipulandum, architecturally similar to the MIT-MANUS and resulting from the MIT/UCBM research collaboration, was recently developed and tested.
- Adaptive bio-cooperative patient–robot interaction schemes for therapy robots, where both psychophysiological and biomechanical information are used for updating robot interaction control. Multimodal assessment of patient performance can be obtained by monitoring the patient’s strength, endurance, and emotional state, possibly anticipating patient motion intentions and modeling internal states. The first examples of bio-cooperative controllers have been developed in the framework of the European projects FP7-ECHORD/MAAT (multimodal interfaces to improve therapeutic outcomes in robot-assisted rehabilitation).
- Soft robotics systems: Wearable robotic suites made of soft structural elements, sensors, and, typically, pneumatic actuators, which are directly linked to the human body for assisting locomotion. Consequently, the performance of the robotic system can be properly evaluated only when coupled to the human component.
Assistive Devices and Artificial Limbs
The fields of prosthetics, orthotics, and functional neural stimulation (FNS) are also closely allied with rehabilitation robotics. Prof. Ferrigno and Dr. Pedrocchi from the Politecnico di Milan recently led the European Union (EU) project Multimodal Neuroprosthesis for Daily Upper Limb Support (MUNDUS), which aimed at developing FNS with robotics to develop more effective assistive devices for people with neurological disorders. Starting from the results achieved during MUNDUS, a follow-up project REaching and grasping Training based on Robotic Hybrid Assistance for Neurological Patients: End Users Real Life Evaluation (RETRAINER), led by Dr. Maria Bulgheroni (from Abacus srl), was recently funded to bring these devices to clinical exploitation and market availability.
Prostheses are artificial hands, arms, legs, and feet that are worn by the user to replace amputated limbs. Surveys [19] on using such artificial hands reveal that 30–50% of amputees do not use their prosthetic hand regularly, basically due to its low functionality, poor cosmetic appearance, lack of sensory feedback, and low controllability.
For this reason, one of the authors of this article (S. Micera)started working a few years ago on intraneural electrodes to be inserted longitudinally (LIFE) or transversally (TIME) thanks to the collaboration with Ken Yoshida (who at that time was at Aalborg University). This approach is clinically promising in the short to medium term because it combines acceptable invasiveness with good selectivity. In particular, LIFEs and TIMEs are flexible polymer structures that are inserted in the nerve and, thus, are better suited for the longitudinal stretch motion of the nerve during limb movement.
To verify these potentials, in 2009, the first clinical trial on a human amputee of LIFEs, developed by Klaus Hoffmann’s team [at the Fraunhofer Institute for Biomedical Engineering (IBMT), St. Ingbert, Germany], was carried out at UCBM [18], demonstrating the feasibility of the restoration of bidirectional neural communication with a multifingered robotic prosthesis [8].
In 2013, TIMEs developed by Thomas Stieglitz (at Freiburg University, Germany) were implanted in a transradial amputee by a team led by S. Micera (with his teams at the École Polytechnique Fédérale de Lausanne and the Scuola Superiore Sant’Anna) and Paolo M. Rossini (Università Cattolica di Roma/Gemelli Hospital) and involving researchers working in many other Italian and European institutions, including another author of this article (E. Guglielmelli). During a four-week experiment, we showed for the first time that amplitude modulation of intraneural peripheral stimulation can provide sensory information about grasping force, object shape, and stiffness to an amputee during the real-time control of a dexterous hand prosthesis [9]. The restoration of the ability to judge the spatial coarseness of a textured surface would represent the next extremely important step toward the reestablishment of the sensory skills of the natural hand.
This goal was achieved by measuring the tension in artificial tendons that control finger movement and turning this measurement into an electrical current, but this electrical signal was too coarse to be understood by the nervous system. Using computer algorithms, the scientists transformed the electrical signal into an impulse that sensory nerves could interpret. The sense of touch was achieved by sending the digitally refined signal through wires into four electrodes that were surgically implanted into what remains of the user’s upper-arm nerves. The experimental setup is shown in Figure 7.
![FIGURE 7 - The experimental setup for validating a bionic prosthesis on a human amputee [9].](https://www.embs.org/wp-content/uploads/2015/07/fig71.jpg)
The clinical study provides the first step toward a bionic hand, although a sensory-enhanced prosthetic is years away from being commercially available. The bionic hand of science fiction movies is even further away. The next step involves making the electrode implants possible for years, miniaturizing the sensory feedback electronics for a portable prosthetic and fine-tuning the sensory technology for better touch resolution and temperature detection. Such goals are being investigated in several European and Italian research projects, such as the NEurocontrolled BIdirectional Artificial upper limb and hand prosthesiS (NEBIAS). EU project coordinated by S. Micera and the research project on innovation of prosthetics (PPR2) recently launched by the Centro Protesi Istituto Nazionale per le Assicurazioni contro gli Infortuni sul Lavoro (INAIL) (Vigorso di Budrio, Bologna, Italy). This leading prosthetic center, which assists more than 12,000 amputees per year, is working to develop translational applications of recent research results in this area as well as to support new breakthrough research achievements.
Important efforts are also ongoing in the field of lower-limb prostheses, including the EU project CYBERLEGS led by Dr. Nicola Vitiello (and involving Silvestro Micera) at the Scuola Superiore Sant’Anna.
References
- G. Baroni, A. Pedrocchi, G. Ferrigno, J. Massion, and A. Pedotti, “Static and dynamic postural control in long-term microgravity: Evidence of a dual adaptation,” J. Appl. Physiol., vol. 90, no. 1, pp. 205–215, 2001.
- A. Aliverti and A. Pedotti, Eds., Mechanics of Breathing: New Insights from New Technologies. Italia: Springer-Verlag, 2014.
- M. Ferrarin, M. Rizzone, B. Bergamasco, M. Lanotte, M. Recalcati, A. Pedotti, and L. Lopiano, “Effects of bilateral subthalamic stimulation on gait kinematics and kinetics in Parkinson’s disease,” Exp. Brain Res., vol. 160, no. 4, pp. 517–527, 2005.
- C. Frigo, E. E. Pavan, and R. Brunner, “A dynamic model of quadriceps and hamstrings function,” Gait Posture, vol. 31, no. 1, pp. 100–103, Jan. 2010.
- B. Siciliano, O. Khatib, M. Van der Loos, D. Reinkensmeyer, and E. Guglielmelli, Eds., “Rehabilitation and health care robotics,” Handbook of Robotics, 2nd ed. Germany: Springer-Verlag, ch. 64 (in press).
- L. Zollo, L. Rossini, M. Bravi, G. Magrone, S. Sterzi, and E. Guglielmelli, “Quantitative evaluation of upper-limb motor control in robot-aided rehabilitation,” Med Biol. Eng. Comput., vol. 49, pp. 1131–1144, Oct. 2011.
- A. Panarese, R. Colombo, I. Sterpi, F. Pisano, and S. Micera, “Tracking motor improvement at the subtask level during robot-aided neurorehabilitation of stroke patients,” Neurorehabil. Neural Repair, vol. 26, no. 7, pp. 822–833, 2012.
- P. M. Rossini, S. Micera, A. Benvenuto, J. Carpaneto, G. Cavallo, L. Citi, C. Cipriani, L. Denaro, V. Denaro, G. Di Pino, F. Ferreri, E. Guglielmelli, K. P. Hoffmann, S. Raspopovic, J. Rigosa, L. Rossini, M. Tombini and P. Dario, “Double nerve intraneural interface implant on a human amputee for robotic hand control,” Clin. Neurophysiol., vol. 121, no. 5, pp. 777–783, 2010.
- S. Raspopovic, M. Capogrosso, F. M. Petrini, M. Bonizzato, J. Rigosa, G. Di Pino, J. Carpaneto, M. Controzzi, T. Boretius, E. Fernandez, G. Granata, C. M. Oddo, L. Citi, A. L. Ciancio, C. Cipriani, M. C. Carrozza, W. Jensen, E. Guglielmelli, T. Stieglitz, P. M. Rossini, and S. Micera, “Restoring natural sensory feedback in real-time bidirectional hand prostheses,” Sci. Transl. Med., vol. 6, no. 222, pp. 222ra19, Feb. 2014.
- G. Ferrigno and A. Pedotti, “ELITE: A digital dedicated hardware system for movement analysis via real-time TV signal processing,” IEEE Trans. Biomed. Eng., vol. 32, no. 11, pp. 943–950, Nov. 1985.
- A. Pedotti, “Simple equipment used in clinical practice for evaluation of locomotion”, IEEE Trans. Biomed. Eng., vol. 24, no. 5, pp. 456–461, Sept. 1977.
- C. Frigo and P. Crenna, “Multichannel SEMG in clinical gait analysis: A review and state-of-the-art,” Clin Biomech., vol. 24, no. 3, pp. 236–245, Mar. 2009.
- L. Mouchnino, R. Aurenty, J. Massion and A. Pedotti, “Coordination between equilibrium and head-trunk orientation during leg movement: A new strategy build up by training,” J. Neurophysiol., vol. 67, no. 6, pp 1587–1598, June 1992.
- H. Schmidt, F. Galbusera, A. Rohlmann, and A. Shirazi-Adl, “What have we learned from finite element model studies of lumbar intervertebral discs in the past four decades?” J. Biomech., vol. 46, pp. 2342–2355, 2013.
- T. Villa, L. La Barbera, and F. Galbusera, “Comparative analysis of international standards for the fatigue testing of posterior spinal fixation systems,” Spine J., vol. 14, no. 12, pp. 695–704, 2014.
- L. Cristofolini, M. Juszczyk, S. Martelli, F. Taddei, and M. Viceconti, “In vitro replication of spontaneous fractures of the proximal human femur,” J. Biomech., vol. 40, no. 13, pp. 2837–2845, 2007.
- Real time simulation for safer vascular stenting. (2015, May 19). [Online].
- E. Dordoni, A. Meoli, W. Wu, G. Dubini, F. Migliavacca, G. Pennati, and L. Petrini, “Fatigue behavior of Nitinol peripheral stents: The role of plaque shape studied with computational structural analyses,” Med. Eng. Phys., vol. 36, no. 7, pp. 842–849, July 2014.
- Atkins, 1996.