For $99, you can obtain a kit that includes two cotton swabs and instructions for properly collecting your own stool sample, along with oral and skin samples. Upon shipping those specimens to the Knight Lab in La Jolla, CA, you will join the ranks of “citizen scientist,” becoming a contributor to the world’s largest crowd-sourced microbiome research project. In return, should you have accepted this mission, you will receive a report that offers you a “snapshot” of the microbes found in your fecal matter, and compares it to that of the rest of the population.
This is the American Gut Project, which has set out to analyze over 10,000 stool samples drawn primarily from the U.S., U.K., and Australia. Among their findings released in 2017 is a strong link between mental health and gut bacteria. One of their tests compared the microbiome of those who report living with posttraumatic stress disorder (PTSD), schizophrenia, depression, or bipolar disorder with those of controls who did not report these disorders and had been matched for age, gender, and body mass index. They found that those who reported mental health issues had more bacteria in common with others who reported the same types of problems than they did with the bacteria of the control subjects. Their report also suggests that some types of bacteria may be more prevalent in people with depression.
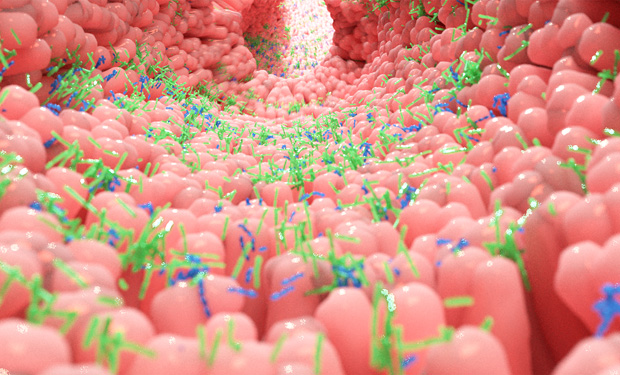
It’s been established for about a decade that microbes are a significant player in gut–brain communications. In animal studies (many of them in mice), the microbiome has been found to affect some emotional behaviors that are thought to mimic human neuropsychiatric disorders, including autism spectrum disorders, anxiety, depression, Alzheimer’s disease, Parkinson’s disease, schizophrenia, and epilepsy. The human studies in these areas are much fewer, but there is evidence for a relationship between the types of microbes living in the gut and brain structure and function. (For an earlier discussion of the link between gut bacteria and depression, see [1].)
Recently, a number of treatments have been emerging from research into the gut–brain axis that may be used in neurodisorder therapies, among them: fecal microbiota transplants (FMT), pre- and probiotics, dietary interventions, and psychobiotics (biotics that have mental health benefits). Some are currently in use, and others, such as FMT, may come into greater use once clinical trials more definitively establish their safety and efficacy. Dietary interventions and FMT in particular hold promise for successful disease treatment options in the near future.
Fecal Microbiota Transplants
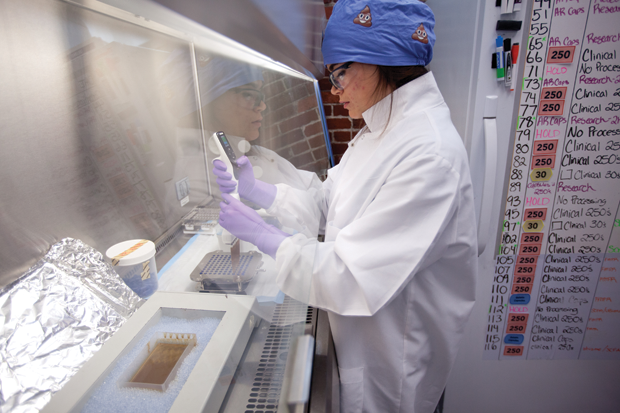
FMTs arguably have the longest history of any of these treatments that seek to transform the patient gut microbiome, yet this approach may prove to be the slowest to come into widespread use due to safety concerns, namely the risk of pathogen transmission from donor to recipient. FMT has been a part of Chinese medicine for hundreds of years, used to address gastrointestinal issues as well as other maladies. There’s also evidence of FMT in Bedouin culture, where camel feces have been used to treat gastrointestinal problems. “Historically, the major barriers to using FMT either as a therapeutic or a research tool are logistical in nature … material processing and safety,” says Dr. Pratik Panchal, Clinical Research Scientist at the nonprofit stool bank, OpenBiome. Donors of feces must be screened, and there need to be the proper facilities to prepare the donor material, screen the recipient, and conduct the actual transplantation (Figure 1).
FMT’s effects on emotion and mood were recently rediscovered during FMT therapy for ulcerative colitis, says Antonio Inserra, who’s part of a group of researchers proposing the “microbiotainflammasome” hypothesis of major depression. Patients reported improved gastrointestinal functions, and also experienced a mood lift and improvements to their emotional state. Discoveries like this suggest that psychiatry might adopt FMT in the future, but we are still some years away from that. “Currently,” notes Panchal, “the use of FMT as a treatment option is limited to patients with recurrent Clostridium difficile infection (CDI) who do not respond to standard antibiotics. Patients looking to use FMT for other indications, including mental health, must be participants in a clinical trial led by an investigator who holds an investigational new drug application with the FDA.”
A recent global survey of clinical trials involving FMT from 2010 to 2018 revealed that over half were focused on CDI and irritable bowel syndrome. However, since 2014, there has been a rapid expansion of FMT clinical trials involving other diseases, with up to ten different disease indications in 2018. Stool banks such as OpenBiome play a significant role in enabling these trials.

OpenBiome is the first public, nonprofit stool bank in the U.S. By centralizing the identification and screening of donors, safety controls, and material processing, it reduces the time for patients with recurrent CDI to receive treatment, and has also enabled broad access to FMT for physicians and clinical researchers investigating other disorders (Figures 2 and 3). Currently, OpenBiome is involved in clinical trials for three neuropsychiatric disorders: depression, multiple sclerosis, and anorexia nervosa.
“Associations do not necessarily mean causation,” Panchal says of the promising early clinical microbiome studies focusing on the link between mental health and the microbiome. They do not mean that FMT is “necessarily an appropriate or effective treatment,” he adds. “More research needs to be done, and patient safety has to be paramount.”

Some adverse side effects of FMT are fever, increased frequency of defecation, abdominal pain, bloating, nausea or vomiting, and flatulence. But there can be more serious effects if pathogens from the donor are transferred to the FMT recipient. This can occur regardless of the method of delivery, whether via colonoscopy, capsule, or enema. “If this transfer is done, it needs to be done with very well-screened donors and with very purified samples and screened samples, and under medical supervision,” emphasizes Dr. Rosa Krajmalnik-Brown, who’s been part of an autism study involving FMT.
FMT and Autism
This recent study, “Long-term benefit of Microbiota Transfer Therapy in Autism Symptoms and Gut Microbiota” [2], exemplifies the promise that the brain–gut microbiome fields holds, as well as some of the challenges in working in this area of research. In this recent open-label study, led by Krajmalnik-Brown, 18 children on the autism spectrum received ten weeks of daily FMT treatments. Over a period of two years, the study showed improvement for the child participants on the Childhood Autism Rating Scale, Social Responsiveness Scale, and the Aberrant Behavior Checklist. “Improvements were such that the children in our study dropped off the scale of being in the spectrum. And that’s fascinating. That’s something that’s not seen with other treatments,” says Krajmalnik-Brown, professor at the School of Sustainable Engineering and The Built Environment and the Swette Center for Environmental Biotechnology at Arizona State University (Figure 4).
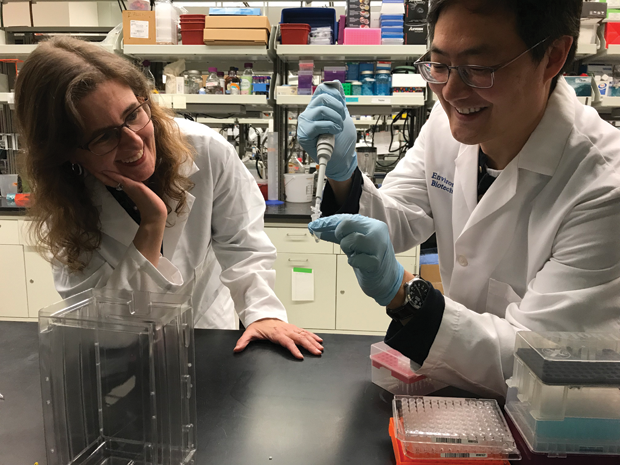
Because this was an open-label study, observers caution that there could be a placebo effect (particularly in this case, hopeful parents might see improvements where there aren’t any). However, Krajmalnik-Brown points out, they had an external evaluator do the assessments of the children’s behavior. And, she says, fellow researcher Dr. Dae-Wook Kang received “blinded samples [of the participants’ microbiome]. We didn’t know which child [a sample] belonged to. We didn’t know if these children had [autism-related symptom] improvements or not. And just by looking at [their] microbiome, you can see a scientific, blinded measurement that shows there’s a huge improvement in the microbiome.”
Autism’s heterogeneity (it can range from severe to light from person to person) and multifactorial mechanisms and risk factors presented one set of challenges to the study group. On the other hand, they also had to contend with the opaque aspect of working with gut microbes. Krajmalnik-Brown’s team didn’t know which microbes have a specific role for autism; they had a hypothesis about Prevotella and that diversity of microbes is desirable. So while they didn’t select fecal samples for transplantation based on the microorganisms that were there, the researchers did know that the samples contained hundreds of different types of microbes—a higher diversity than if they’d been treating the participants with a probiotic.
“One of the things that my lab is focusing on,” Krajmalnik-Brown says, “is trying to learn from the treatments. So, you transplant a sample that is very diverse, but it is very interesting to see which are the microbes that increase in proportion [during] treatment. Or which of the microbes we can correlate with improvements… One of our hypotheses is that metabolites produced by microbes are … actually destroyed by microbes that normally would get to the brain their concentrations are changing in the gut, and this might be one of the mechanisms by which the gut communicates with the brain,” she observes.
For Dr. Emeran Mayer, author of The Mind-Gut Connection, this study is less interesting for what it may show about the benefits of FMT, and more noteworthy for its novel treatment approach. The study combined regular FMT treatments with broad spectrum antibiotics at the start that knocked out the baseline microbiome. Then, FMT was transplanted and repeated over a period of time, on a weekly basis. “That, in my opinion, is a promising approach,” says Mayer, who directs the G. Oppenheimer Center for Neurobiology of Stress and Resilience and co-directs the CURE: Digestive Diseases Research Center at the University of California, Los Angeles. “It’s like bone marrow transplantation in lymphoma or leukemia, or ecosystem restoration in nature where you want to wipe out the bad ecosystem and then start it from scratch again.”
Interested but cautious observers of this autism study say they want to see if this line of research can demonstrate similar outcomes in future, double-blind, placebo-controlled trials. Krajmalnik-Brown hopes that future iterations of this research will enable them to identify a few key microbes that are important for this treatment, and grow those microbes in the lab so that they don’t have to rely on FMT. “In my opinion, it will probably be more than a microbe. It will be a community,” she adds. “But we can still grow a community in our reactor. So, either a community of microbes that can be grown in the lab in a cleaner way, or in fermenters—it doesn’t have to be in the lab.”
A Future Microbial “Fingerprint”
Could science identify a silver-bullet microbe that could change a whole disease course? This question comes up when evaluating the success of other brain–gut-microbiome treatments such as probiotics. Mayer says it’s simplistic to think this way, and that the gut–brain axis is a much more complex system. “Some people would say that the reason current [probiotic] studies are not more impressive is because you give the same probiotics to people with highly different microbial communities,” Mayer explains. “Once you would be able to ‘fingerprint’ individuals, then you could customize the probiotic and maybe get a 30% higher responder group. Even though this has not been demonstrated yet, it is a plausible hypothesis.”
Diet’s impacts on the gut—and the mind
Less novel, but more direct, dietary changes are an effective, widely available intervention for reshaping the composition of our gut microbiome. By extension, diet can treat mental illness resulting from heightened inflammatory signaling or pathological shifts in the gut microbiome, says Antonio Inserra. An example he offers: Consuming foods with high tryptophan content can boost the serotonergic system. As far as cognitive function, Mayer describes a study from Rush University Medical Center in which the influence of diet on cognitive decline was assessed in a large number of healthy individuals in their 70s and 80s. Those that consumed a modified Mediterranean-type diet (“MIND diet”) showed a much slower cognitive decline than those on the typical American diet [3]. This diet brings fiber and polyphenols and other phytochemicals (health-promoting molecules) into the gut, both of which increase the diversity of microbes, reduce the leakiness of the gut, and increase delivery of beneficial gut microbial metabolites to the brain.
“I would say that diet is the one [gut–brain axis treatment] that is now being evaluated in a rigorous way for several brain disorders, including depression, Alzheimer’s disease, and Parkinson’s disease,” says Mayer, “and in my opinion has the biggest potential, not as magic cure, but as a modulator of disease trajectories.” Mayer cautions, “New treatments that only target the gut microbes directly are not enough. You can’t ignore the non-microbial parts of the system such as genetics, psychosocial factors, and environmental exposures. Also, we don’t yet know to what degree different brain disorders are caused by the brain, the gut, or both.”
And yet, the bidirectional communication loop between the brain and the bowels, so to speak, is being corroborated again and again in studies. And while all of the treatments discussed here focus on treating the gut to heal the brain, the benefits and harm extend both ways. Mayer mentions one of his studies in conjunction with a group at the University of Buffalo that looked at the effect of cognitive behavioral therapy (CBT) in patients with irritable bowel syndrome. One of the findings is arguably no less astonishing than any of those mentioned so far, and yet it stands out: CBT significantly improved symptoms in close to 60% of patients. This improvement was associated with a change in brain structure and function, as well as in the composition and function of the gut microbiome. Outcomes like this confirm that there is communication traveling both directions between gut and brain. Consequently, says Mayer, “you can influence a dysregulation by targeting this brain–gut-microbiome axis at different levels. You could have the benefit to a brain-targeted therapy and you could have a benefit to do with probiotics or diet at the gut level, at the microbial level.” This bidirectional relationship is likely to complexify and expand the range and set of treatments available to patients in the coming years.
References
- M. Bates, “Gut feeling: Researchers are discovering a link between depression and gut bacteria,” IEEE Pulse, vol. 8, no. 6, pp. 15–18, Nov.–Dec. 2017.
- D.-W. Kang et al., “Long-term benefit of microbiota transfer therapy on autism symptoms and gut microbiota,” Sci. Rep., vol. 9, 2019, Art. no. 5821.
- M. C. Morris et al., “MIND diet shows cognitive decline with aging,” Alzheimers Dement., vol. 11, no. 9, pp. 1015–1022, Sep. 2015.