Progress in creating malaria vaccines has been slow, but a new take on an old method of using live parasites promises the potential for herd immunity.
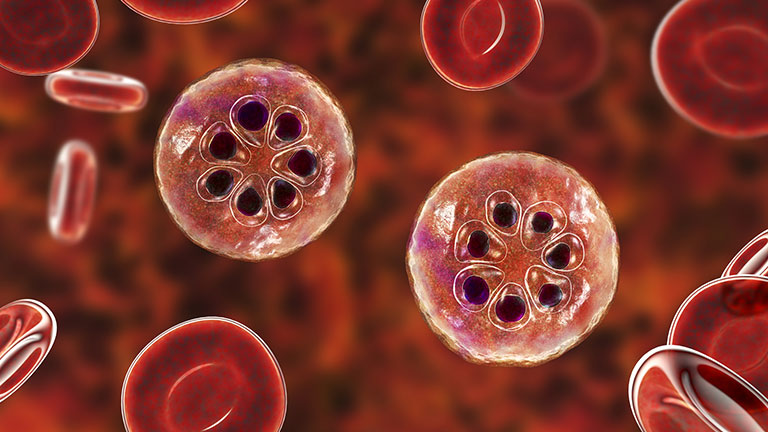
Malaria is a disease that has plagued humanity since ancient times. Mentioned in Chinese scriptures from almost 5,000 years ago, and throughout Greek and Roman literature, it is caused by Plasmodium parasites, which infect humans through the bite of the infected female Anopheles mosquito. Though it is both preventable and curable, it kills hundreds of thousands of people every year.
According to the World Health Organization (WHO), there were 229 million cases worldwide in 2019, which caused 409,000 deaths. Children under five are most at risk, accounting for two-thirds of those deaths. Though the disease is present globally, the vast majority of cases (94%) are found in Africa.
Kwadwo Koram, an epidemiologist at the University of Ghana, Accra, Ghana, has seen the impact of the disease on local communities since the start of his career, and while he has seen great efforts made to control the disease, he is aware that there is much left to do.
“A lot of progress has been made over the past three decades,” he remarks. “When I was in training in the ’80s and early ’90s, the estimates were that malaria was responsible for more than a million deaths annually, almost all of them in Africa. The current estimates are somewhere less than 500,000 deaths annually, so one can talk of progress.”
“However, for a preventable and curable disease, one death is one death too many,” he adds. “Besides, for the poor mother in my village who loses a child to malaria, that is a disastrous occurrence, so even as we celebrate the success of reducing malaria mortality we should think about such mothers and redouble our efforts to achieve elimination and eradication.”
With the discovery of the parasite’s life cycle by British Army surgeon Ronald Ross toward the end of the 19th century, efforts to control the disease targeted the transmission vector and its known habitats (Figure 1). Since then, the focus has shifted more toward the potential of vaccines, though development has been slow and progress has been hampered by low efficacy.
In October 2021, however, the WHO approved the world’s first malaria vaccine—Mosquirix (RTS,S)—for use in Africa, following the results of an ongoing pilot program in Ghana, Kenya, and Malawi. The vaccine can be given to children aged six weeks to 17 months to protect against malaria caused by the Plasmodium falciparum parasite.

“This is a big step forward,” Koram believes. “I believe we should be humble enough to realize that it will take a long while to get the magic bullet that will solve the malaria problem, so we should be glad for anything that allows us to chip away at the problem a little at a time. We should also not fool or lull ourselves into thinking that we have the solution to the problem.”
Magic bullet?
Vaccine development has been challenging because the biology of a parasite is more complex than that of a virus or a bacterium. The publication of the genome of the parasite 20 years ago was a great step forward, but the function of several genes remains to be mapped. Koram believes that, as our understanding of the parasite’s genes grows, it will be possible to develop a parasite vaccine but that, for now, Mosquirix is the most viable vaccine option. Others disagree.
For Stefan Kappe, affiliate professor at the Department of Global Health, University of Washington, who studies malaria-parasite biology and immunology at the Seattle Children’s Research Institute, Seattle, WA, USA, Mosquirix falls down because of its limited efficacy. He compares it to a Covid-19 vaccine that is only 20%–30% effective. “It confers modest protection but claims are exaggerated,” he remarks. “It will only have an impact with other malaria interventions, such as insecticides, so it is an add-on to the toolkit for preventing malaria.”
Currently, Kappe is collaborating with researchers at biotechnology company Sanaria, who are developing a vaccine that uses a disabled version of the whole parasite, rather than individual proteins. It is the next iteration of radiation-attenuated Plasmodium falciparum sporozoite (PfSPZ) vaccines.
“If our vaccine is highly efficacious, it could be used to vaccinate large populations and stem the transfer of infection from the blood of infected humans,” he believes. “The whole parasite concept started in the 1960s. It used parasites that infect mice and irradiated them, so you could induce complete protection. Trials in humans showed complete sterilizing immunity.”
“Sanaria took up that concept 15 years ago,” he adds. “Administering irradiated parasites by injection provides robust protection in volunteers never infected by malaria, and confers very high levels of protection against homologous strains and less against heterologous strains, but it is still better than RTS,S, even though that does reduce the incidence of severe malaria.”
With such impressive results from live parasites vaccines, one question remains—why have we not seen such a vaccine fully developed and approved? The answer lies in the development path of genetic engineering technologies.
“Though parasites were a great concept, they were not what you wanted to build a vaccine on, but with genetic engineering we can now delete certain genes from the 5,000 genes in the parasite that leave it alive but mean it cannot replicate in the liver,” Kappe explains.
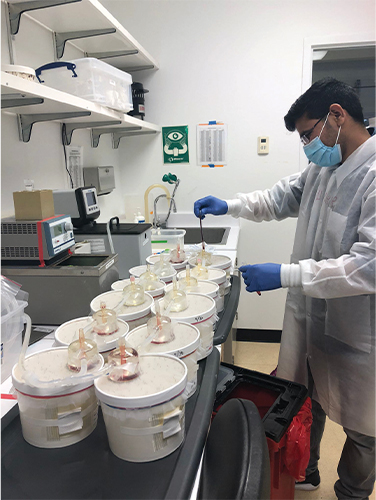
To test its vaccines, Sanaria uses parasites that have been genetically engineered using CRISPR-Cas9 technology to delete genes that render it harmless for the human vaccinee (Figure 2). The initial result was a parasite that infects the liver and dies off, rather than growing to build biomass in the liver.
“They are comparable to irradiated parasites,” he explains. “The level of protection is good, but it can be better, so we wondered if we let the parasite build up in the liver, replicate, and add biomass would it provide more protection? We don’t want blood infection, but the new strain we developed helps create the antigens without breaking through into the blood. In rodent models, we have shown that this latest generation strain, which will go into clinical trials in the spring, is superior to irradiated parasites.”
Long road to immunity
Dr. Patrick Duffy, who works on malaria vaccines at the U.S. National Institute of Allergy and Infectious Diseases (NIAID), Bethesda, MD, USA, has a bird’s eye view of the measures taken to combat malaria, from drug treatments and vector control to the development of vaccines. He has also seen Sanaria’s work up close, as NIAID is a collaborator in its development program.
After the studies done to date, Duffy senses that a new era is about to start, as the potential of whole parasite vaccines is realized.
“Mosquirix is the first vaccine against a parasitic disease in humans, but it is only partially effective,” he observes. “It is another tool in the toolkit. Then there is R21, which works in a similar way. Whole organism vaccines were not thought to be practical for malaria, but now we have a company that is making purified sporozoites for human injection.”
“Before, the barrier was the creation of the microbe, and there had been little success growing the different developmental stages of the parasite, but now we have a method to produce aseptic mosquitoes from which the salivary glands can be harvested. Though it generated a lot of skepticism at first, it is a leap of imagination.”
Kappe is hoping that the vaccine will offer more than 90% protection against infection. If that goal is reached, the vaccine could be used as a standalone protective measure and, potentially, create herd immunity. In that scenario, other control measures that are costly and difficult to implement would not be used.
“Studies tell us that it is possible to generate very high levels of sterile immunity to strains other than the one you vaccinate with,” says Duffy. “We didn’t expect the levels of efficacy we saw. We were amazed by them. It was an unexpected but happy outcome.”
“The next step is to see if we can administer drugs to kill the parasites at the same time as the sporozoites,” he adds. “A study in Mali has shown the efficacy of that approach, so we need to look at what regimen gives us the highest efficacy in the field.”
Inevitably, there are potential pitfalls that could limit the effectiveness of the new vaccine. As drugs are required to kill the parasite after infection, there is the possibility that drug resistance could emerge. As Koram points out, the principle rests on having a safe drug and also a sensitive parasite, and we should be alert for reduced vaccine efficacy that may develop as a result of parasite resistance.
Consequently, the task of eliminating malaria will not be easy. It will require patience and consistent investment in all aspects of infection control and prevention. Parasites evolve and infection vectors change over time, so the efficacy of vaccines and drug treatments must be under constant review.
That said, the work being done by Sanaria represents a paradigm shift in the approach to malaria vaccines. The hope is that it could deliver a significant acceleration of movement along the road to malaria elimination, which now seems less like a pipe dream and more like an achievable goal.