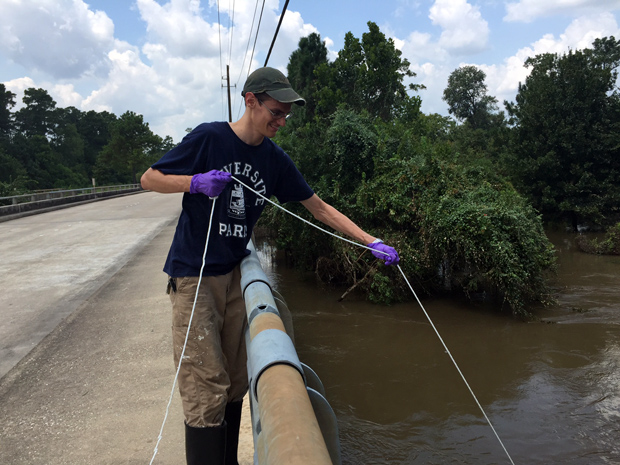
Above, Figure 1: 2. Seth Pedersen, a graduate student from Rice University, wades into a flooded street to collect water samples after Hurricane Harvey flooded Houston, TX. Photo Credit: Ya He.
In early September 2017, when the rains from Hurricane Harvey finally subsided in Houston, Texas, Seth Pedersen loaded up his pickup truck with sample collection kits, waders, rubber boots, buckets, and a small aluminum fishing boat. On that particular day, Pedersen, a second-year graduate student in environmental engineering at Rice University, was—along with a fellow graduate student—on a mission to test the water in homes flooded by Hurricane Harvey. He was looking specifically for E. coli bacteria, chemicals, heavy metals, and other pathogens (Figure 2).

Pedersen was part of a team of researchers in the greater Houston region who were sampling floodwaters in areas affected by Harvey to better understand the public health risks they posed (Figures 1 [above] and 3 [below]). The test results were not surprising: the samples revealed a host of bacteria and chemicals.
“There were definitely bacterial pathogens present—that’s why researchers often see an uptick in gastrointestinal diseases after floods in public health studies,” says Lauren Stadler, an environmental engineer at Rice University and one of the leaders of the project. “There was definitely sewage running off and being untreated, because that’s what happens in the event of a flood. Even with household chemicals that you keep under the kitchen sink—when your house gets flooded, where do you think those go?”
Earlier in 2017, Hurricane Harvey was preceded by a huge flooding event in South Asia that affected 41 million and killed more than 1,000 across Bangladesh, India, and Nepal. Hurricane Maria, which followed Harvey, swept through Puerto Rico in September 2017. In 2010, flooding in Pakistan displaced more than 20 million people; Hurricane Katrina in 2005 forced approximately 200,000 Americans living along the coast of the Gulf of Mexico to leave their homes and killed nearly 2,000.
Worldwide, floods are the most frequently occurring natural disaster and cause the most human suffering and loss, according to Jorge Castilla, an emergency officer at the World Health Organization (WHO). And it’s getting worse: rains during monsoon seasons are get- ting stronger in Asia, India, Australia, and other tropical regions. While the immediate hazards include serious injuries or even death, there are also long-term public health consequences.
In the days and weeks fol- lowing floods, the threat of contracting an infectious disease is high [1]. For instance, after the 2010 foods in Pakistan, more than 6 million people suffered from gastroenteritis, respiratory infections, malaria, and skin conditions. Diarrheal diseases were ram- pant due to a lack of safe drinking water. In 2015, floods in Chennai, India, also led to a spike in cases of diarrhea, cholera, dysentery, respiratory infections, hepatitis A and E, typhoid fever, leptospirosis, and vector-borne diseases. Recent re- search from the Karolinska Institute in Stockholm, Sweden, confirmed the impact of floods on human health after examining 113 cases of floods that occurred worldwide. Notably, they found that skin infections, gastrointestinal infections, wounds, and poisonings from carbon monoxide, gasoline, bleach, and hydrocarbons all spiked after storm events in both developing and developed countries.
The specific public health impacts of floods depend greatly on where the flooding event occurs. For instance, because Houston is home to many oil and gas companies, the floods that accompanied Harvey sent a cocktail of chemicals into the floodwater. Sewer overflows unleash a host of microbes into water that can infect open wounds and cause disease, as Pedersen and Stadler have observed in their test results. As such, health authorities in Houston were concerned about the possibility of a surge in flesh-eating bacteria, as well as cases of antibiotic-resistant staph infections, diarrheal disease from noroviruses, and respiratory infections and disease. (One woman from a Houston suburb died from coming into contact with flesh-eating bacteria in water.) Because it takes time for high floodwaters to recede, pools of standing water become a breeding ground for mosquitos, which can carry viruses such as West Nile, dengue, chikungunya, and Zika. (At the time this story went to press, there was no significant increase in respiratory illnesses in the month after Harvey—according to data collected by the Health Department in Houston, which tracks over 70 conditions in real time—compared to the same time period in 2016, when Houston was not flooded.)
Molecular Surveillance of Disease
In floodwaters sampled after Harvey, Stadler was particularly interested in the microbial communities present. Currently, she and her colleagues are using 16S ribosomal RNA sequencing to profile the microbial communities present. However, she doesn’t have data from before the flood. “That’s actually one of the biggest concerns I have,” she says. “That, from a scientific perspective, we don’t have baseline data to compare it to.”
Elsewhere, researchers are sampling components in their environment and investigating the unique microbial communities that exist. Sewage, for example, teems with a host of microbes and viruses that could be pathogenic. One team of researchers (called Underworlds) from the Massachusetts Institute of Technology in Cambridge is using technology to understand the microbial composition of sewage. Tapping into this reservoir of information, project manager Newsha Ghaeli says, can help cities and municipalities monitor urban health patterns. While the project has not yet reached that point (team members are still manually sampling sewage and performing a metagenomic analysis on these samples), their hope is that this type of platform can be automated and used in real time to help communicate public health risks and decisions.
One global consortium, MetaSub, is working toward a better understanding of a molecular and genetic view of cities. “There’s a global push to understand cities, sewage, buildings—the entire built environment—at a molecular and genetic level,” says Christopher Mason (Figure 4, right), a computational biologist at Weill Cornell Medical Center in New York City and director of MetaSub. Spanning more than 70 cities and six continents, MetaSub uses metagenomics to determine what microbes are present on distinct surfaces.
“So when you do have a flooding event, you already have a genetic baseline of a city. You’ll know what the state was like when things were healthy and normal, and it wasn’t disrupted,” Mason explains. Following Hurricane Sandy, which hit New York City in the fall of 2012, floodwaters inundated the South Ferry subway station in lower Manhattan. Afterward, Mason and his colleagues swabbed the walls of the station and found that many of the microbes they detected resembled marine and fish-related bacteria. “Things that you normally found in the ocean were still present on the surface a year later as they were repairing the station,” Mason says. “It carried what we like to call a ‘molecular echo’ of what had occurred at the station.”
But building a baseline profile of cities can be labor intensive. Right now, much of the molecular profiling is performed manually, i.e., researchers go out into their communities, collect samples, and bring them back to the lab to be analyzed. Members of Mason’s lab at Weill Cornell, however, are developing prototype automated samplers that can either be attached to someone’s arm, e.g., a swab that comes out and then retracts back, or that can be attached to bike wheels. “You’d go out, ride on your bike for a while, and then come back to the lab and take it off,” Mason explains.
Understanding the Medical Needs of the Community
Cities and municipalities prone to flooding should also develop preparedness, contingency, and emergency health response plans tailored to their specific needs, as well as consider the many risks associated with flooding, says the WHO’s emergency officer Castilla. One way for cities to do this would be to understand the medical needs of the communities they serve.
Juanita Graham, a professor of nursing at the University of Southern Mississippi, Hattiesburg, has reflected on the impacts of Hurricane Katrina to formulate solutions. She writes that, if public health officials already have an understanding of the overall health of the populations they serve, they can use this type of information to effect decision making while responding to and recovering from disasters. For instance, gathering data and showing that a population might have a high rate of diabetes suggests that, during disasters, the emergency response team should be able to immediately provide insulin for the community.

Understanding the needs of patients who lived with chronic illnesses prior to a disaster could translate to healthcare facilities carrying their medications, even in the face of disaster, so these patients can continue treatment without any disruption. “Some counties have made efforts to collect this type of health data, although it is not collected uniformly and comprehensively at the county level, nor is it always readily accessible,” says Kimberly Gill (Figure 5, right), a sociologist at the Disaster Research Center at the University of Delaware. Gill is currently working with researchers at Johns Hopkins University on a community resilience project called COPEWELL, which looks at county-level community health during and after a disaster.
Apps can also alert users whether there are public health issues lurking in their proximity. The Program for Monitoring Emerging Diseases (ProMED) is a web-based reporting system that provides early warnings of disease outbreaks so that public health precautions can be taken at all levels to prevent transmission.
In 2006, a group of researchers at Boston Children’s Hospital founded HealthMap, a tool that aids the real-time surveillance of emerging public health risks. HealthMap takes data from local health departments, travelers, eyewitness reports, and governments and organizes these data so that people who utilize their app, Outbreaks Near Me, can be alerted to any health risks in their neighborhood. App users can also set a notice to be automatically alerted when an outbreak is occurring nearby. (ProMED and HealthMap collaborate in their efforts to provide real-time information on health hazards.)
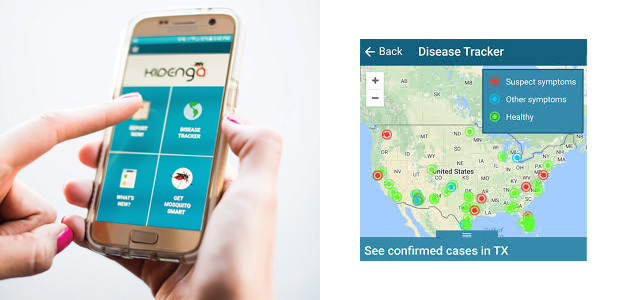
Researchers with the Zuckerman College of Public Health at the University of Arizona, Tucson, have recently developed Kidenga (Figure 6, below), a crowdsourcing app aimed at detecting outbreaks of Zika. The app allows public health investigators to track the location of mosquitos and identify people with symptoms of illness. Kidenga uses information from citizen scientists to track data on Aedes aegypti (the yellow fever mosquito), which transmits not only Zika but also viruses like dengue and chikungunya.
Rethinking Location

To respond to diseases that may arise after floods, cities should ensure that their main hospitals are located outside of flood zones. Sabrina McCormick (Figure 7, right), a sociologist at George Washington University’s Milken Institute, and her colleagues performed a case study of Tampa, Florida, a city vulnerable to hurricanes. “Their main hospital is out on a peninsula. People are going to have a really hard time using that critical infrastructure during a flood because it may be flooded itself,” she says.
These low-lying healthcare centers should be moved, if possible, argues Castilla of the WHO, to an area “above normal flood levels to ensure continuous operations after a seasonal flood.”
Over the longer term, floods may impact the mental health of those who have been displaced. “We see a lot of stress, anxiety, and other mental health effects following these extreme events,” McCormick says. After Katrina, for instance, New Orleans experienced a large number of suicides. “We need to be building our health care infrastructure to support people who have experienced these events, because they’re becoming more frequent and more severe.”
References
- D. D. Saulnier, K. B. Ribacke, and J. V. Schreeb, “No calm after the storm: A systematic review of human health following flood and storm disasters,” Prehospital Disaster Medicine, Oct. 2017. doi: 10.1017/S1049023X17006574.



