Telemedicine provides access during the pandemic
In a Jetsons episode from 60 years ago, Elroy, the youngest Jetson, tries to get out of taking a space calculus test at school by telling his mom he’s sick. “I think I have Venus Virus,” he says. His mom doubts him, but summons a doctor anyway. She presses a large red button in their living room and a screen rolls down from the ceiling. On it, a doctor instantly appears to evaluate Elroy. “Venus Virus? Oh, that can be catching,” the doctor says, donning a mask.
In March of this year, this scene was being reenacted (minus the cartoon levity) in homes around the world, as patients and doctors connected on-screen to discuss health issues while avoiding the highly infectious novel coronavirus, COVID-19. Hardly a futuristic concept anymore, telemedicine, or telehealth, has been available for decades, though it’s been largely a niche practice—until the pandemic (see “U.S. data on telemedicine use due to COVID-19”). Overnight, virtual doctor’s visits spiked, prompting speculation about whether this forced entrée into telehealth would transform into the new normal—even after the virus recedes.
The number of virtual visits will likely dip as cities open up. Nevertheless, telemedicine experts believe this moment may result in more mainstream adoption and spur development of ancillary devices that could make virtual visits less “chat” and more data-exchange. If the digital divide can be addressed and if federal waivers that expanded insurance coverage in the United States remain in some form, telemedicine could broaden access to health care-at-home for those who’d benefit from it the most: the elderly, the mobility-impaired, those with chronic conditions, and the immunocompromised.
Sudden return of the house call
Ten to fifteen years ago, telemedicine was not designed to be accessed at home. “You had a big cart in an emergency room, a big telepresence system,” recalls Dr. Peter Antall, chief medical officer of Amwell, a telemedicine company that offers urgent care video conferencing to patients in 44 states (Figures 1a and b). In their 2016 report, “The State of Telehealth,” Drs. Ray Dorsey and Eric Topol anticipated a shift in telehealth away from clinics and hospitals and into homes. The spread of broadband, an increase in portable diagnostic technologies, coupled with the number of homebound elderly and those with chronic conditions reaching into the millions, they wrote, would accelerate this shift. “Evidence abounds,” they predicted, “for the proximity of a ‘tipping point’ in telehealth, in which adoption moves beyond early adopters, who are focused on the technology, to the majority, who are focused on pragmatic applications.” Dorsey and Topol did not mention a global pandemic, but perhaps COVID-19 will have turned out to be the not-so-gentle tap that tipped the scale.
Removing the barriers for widespread use
Moving medicine to tele-modalities, rapidly and at scale, meant more than an exchange of phone numbers between doctor and patient. Telehealth delivery and reimbursement are multilayered. There are legal barriers, financial disincentives, licensure constraints, infrastructural challenges, training, and processes—not to mention technology platforms—all of which required some significant federal changes to make telehealth accessible to more people. As platforms scrambled to find the needed server power to support the new volume of users, the U.S. federal government approved policy changes to make it easier for the country to use telemedicine. These included expanding telemedicine coverage by Medicare (making it available to 60M elderly people) and allowing non-Health Insurance Portability and Accountability Act (HIPAA) compliant technology to be used (e.g., Zoom or FaceTime). Additionally, the Federal Communications Commission (FCC) gave temporary access to the 5.9 GHz spectrum for rural wireless broadband and proposed a “COVID-19 Telehealth Program” to financially assist health care providers with telehealth services.
U.S. data on telemedicine use due to COVID-19
A study conducted by Harvard University and Phreesia, a health care technology company, found that the number of visits to ambulatory practices had declined nearly 60% by early April 2020 (based on data from 50,000 U.S. providers) while telehealth visits increased rapidly, up by 14% from their baseline pre-COVID. By late June 2020, use of telehealth was falling.
At the University of Rochester Medical Center, Dorsey says telehealth visits rose to 60% of total visits between March and May. In the six-week period from March 7 to April 11, Cleveland Clinic’s outpatient visits swelled from 2% remote (virtual or phone) to 75% remote. Amwell reports a 1000% increase in visits on average year over year (YOY) driven in part by COVID-19. In some geographies, they said, it’s a 3000%–4000% increase.
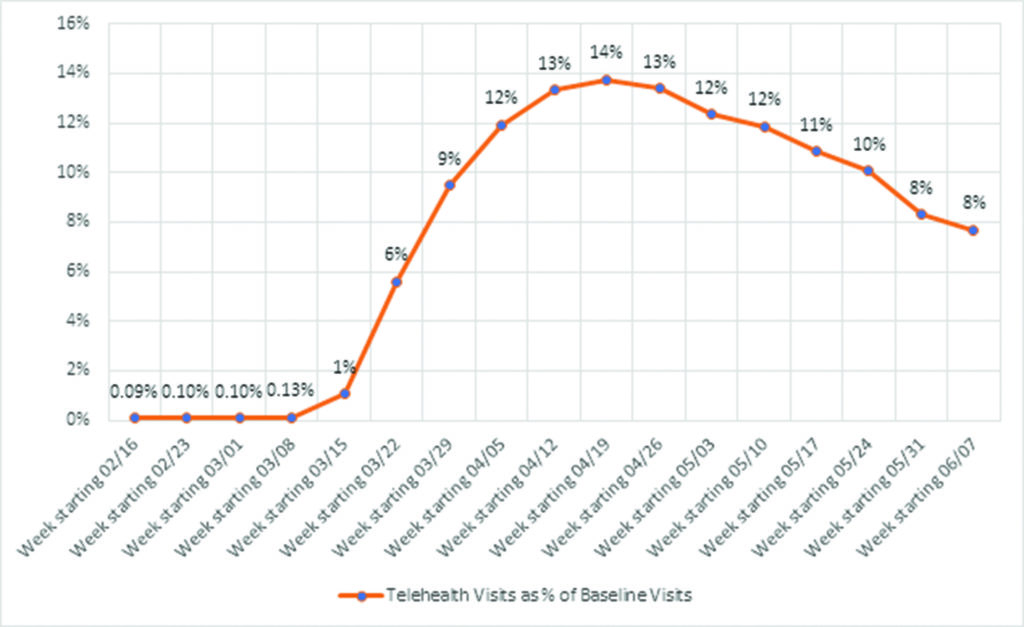
Data are presented as a percentage, with the numerator being the number of telemedicine visits in a given week and the denominator being the number of visits in the baseline week (March 1–7). Telemedicine includes both telephone and video visits. Before the pandemic, roughly 0.1% of all visits were telemedicine. In April, that number jumped to 14%—more than a 1000% increase. [Graph reproduced from A. Mehrotra et al., “The impact of the COVID-19 pandemic on outpatient visits: Practices are adapting to the new normal,” Commonwealth Fund, June 2020 (https://doi.org/10.26099/2v5t-9y63).]

The expansion of Medicare coverage was perhaps the most significant of these changes (Figure 2). “I care for people with Parkinson’s disease and have been doing so via telemedicine for 13 years,” Dorsey said in an interview. Dorsey is director of the Center for Health + Technology at the University of Rochester Medical Center. “I don’t think Medicare has ever paid us for providing care to thousands of patients that we’ve seen in their homes. That all changed in a blink of an eye.”
Reaping the benefits
Telemedicine offers advantages beyond the obvious benefit of allowing patients to avoid infection with COVID-19. It’s more convenient, especially for those who are distant from their specialists or for whom travel is difficult (Figure 3). For Parkinson’s patients, one survey found that a typical 30-minute doctor’s visit took them 4 hours and 15 minutes from door to door. Telemedicine saved them an average of 3 hours of travel time and 100 miles of travel [1].
At times, the inconvenience of getting to a clinic is not offset by the value of being there in person. “How many times do patients come in and sit in an office in a chair—not on the exam table, not in the white paper gown—and just talk about their medications and adjustments and look at their lab results? … Why do we need to bring somebody into an office for that?” Antwell asks.
Medical care can be more comfortable at home— and not just because you’re on your own couch instead of an exam table. Dorsey believes there’s an equalizing quality to a virtual visit: “You’re at eye level with the clinician. You’re on your terms and the clinician’s on their terms, and the power asymmetry is reduced. You can be surrounded by your pets and your loved ones and whatever else you want to be surrounded with in your home.”
Telemedicine is arguably also more confidential. “If you go to a neurology Parkinson’s clinic,” Dorsey points out, “you’re basically saying, ‘I have Parkinson’s disease.’ … If you go to an HIV clinic, you’re telling the world that you have HIV.” With telemedicine, personal medical information isn’t broadcast by your physical movements— and most users interviewed for this piece say they are comfortable taking the usual data security risks entailed in using digital platforms for their virtual visits.
Conventionally, telemedicine has been used for routine problems such as strep throat or skin rashes, as well as for mental and behavioral health. Telemedicine can also be instrumental when time is a crucial factor in treatment. For example, mobile stroke units use live video connection to bring a stroke neurologist “into” an ambulance for more rapid diagnosis and treatment all before the patient reaches the hospital. Telemedicine can also be integrated into a “hospital at home” model for older adults in which remote monitoring by physicians connects to at-home devices, freeing elderly patients from risk of other infections with hospital admission. These scenarios notwithstanding, telemedicine has been considered less suited for conditions that are life-threatening or complex, such as cancer. “When you have a complex patient with multiple comorbidities, that’s when it starts to break down,” says Dr. Eric Topol, director of the Scripps Research Translational Institute and author of Deep Medicine.


When touch is impossible
Telemedicine’s greatest advantage in a time of COVID-19 is arguably its greatest weakness in ordinary times: the absence of physical touch. “The biggest problem with [a virtual] visit is you lose human touch—laying of hands, doing a physical exam,” observes Topol.
In addition to the impediment of not being able to physically examine patients, doctors also find it challenging to establish trust and empathy, and to pick up on nonverbal cues when consulting virtually. When they do achieve these things over a video call, they have to work harder to do so. A small, qualitative study conducted with psychiatrists who’d transferred their practice to virtual visits found that one of the negative impacts for them was a “reduced ability to observe nonverbal cues to support diagnosis and treatment” [2].
Dr. Amy Wells, a naturopathic doctor (ND) primary care physician in Seattle, says she feels “spent” after a full day of virtual visits, as compared to a 9-to-5 day of in-person care. “I’m a people person … there’s so much we pick up on in person … smells, body movements. You have to work really hard to pick up on things through the screen.”
London-based general practitioner (GP) Dr. Kamila Naz agrees: “Phone calls are often more exhausting than a face-to-face because we’re relying on the patient giving us information about their current symptoms, which can be a long-winded process. Whereas when I see someone face-to-face, I can make a lot of decisions very quickly about that patient, based on observing them physically and picking up the nonverbal cues.”
Despite media references to “virtual visits,” telemedicine— during the pandemic at least, is often no more than a phone call with a doctor. “It’s hard to get your 75-year-old patients to get on a Zoom call, so a bunch of these [telehealth visits] turn into phone calls,” Mehrotra says. And although a phone call can be more distraction-free than video for some users, it still can’t convey everything.
“What we can’t see is the patient’s reaction,” says cardiologist Dr. Simeon Rubenstein. “Particularly with a new patient,” he adds, “it’s harder to have an interpersonal relationship.”
More data with your conversation
Now that more people are tapping telemedicine, this may be the moment to revamp it. How might we, asks Topol, push it to its “2.0” stage, where telemedicine becomes “more objective and meaningful than a video chat” through integration of ancillary technologies. A small percentage of people have at-home devices that can measure heart rate, oxygen levels, blood pressure, and glucose levels. Imagine, says Topol, creating more tools that allow a patient to transmit more data to their doctor from home by enabling labs and exams at home with a doctor’s remote supervision. “[We need to build] on the patient consumer side,” proposes Topol, “[by giving them] sensors, self-imaging, self-lab tests they can do on their own, whether it’s through their saliva, a finger prick stick” or other means.
For example, suspected urinary tract infection or ear infections could be confirmed or ruled out with home self-testing. The possibilities for selfexam could be multiplied through smartphone imaging. “I’ve been able to do a smartphone exam of every organ in my body except my brain,” says Topol, “using my phone with an ultrasound probe.” Extended to patients at home if or when the probes become more affordable, a doctor could talk patients through the process in conjunction with artificial intelligence (AI) guidance.
That said, even the most innovative and consumer- friendly devices for augmenting the telemedicine experience can only impact patients who have video streaming. Dorsey explains, “[In the USA,] there’s differential access to the Internet and related technologies based on who people are, where they live, their level of education, and race. 20% of homes lack broadband access and 20% of individuals lack smartphones.” Telehealth’s champions will have to reckon with this digital divide if it is to become a more permanent, widely used mode of care. If they succeed, telemedicine’s inherent advantages of privacy, comfort, convenience, and accessibility mean it could do more than get really good at simulating face-to-face doctor visits—it could, in many cases, surpass the in-person visit altogether.
References
[1] E. R. Dorsey et al., “Randomized controlled clinical trial of ‘virtual house calls’ for Parkinson disease,” JAMA Neurol., vol. 70, no. 5, pp. 565 570, 2013, doi: 10.1001/jamaneurol.2013.123.
[2] L. Uscher-Pines, J. Sousa, P. Raja, A. Mehrotra, M. L. Barnett, and H. A. Huskamp, “Suddenly becoming a ‘virtual doctor’: Experiences of psychiatrists transitioning to telemedicine during the COVID-19 pandemic,” Psychiatric Services, May 19, 2020. [Online]. Available: https://www.rand.org/pubs/external_publications/EP68177.html
Sarah Campbell (sarah.campbell.k@gmail. com) is a writer living in Seattle, WA, USA.



