Suppose you were out on a small boat, 100 mi from shore, with a few friends. Suddenly, one of them begins coughing hard and complaining of aches and pains and chills. It could just be the start of a bad cold, but he also seems to be running a fever, which might signal the onset of the flu. But it could also be something more serious, like bacterial pneumonia, that might require hospital care. How would you know?
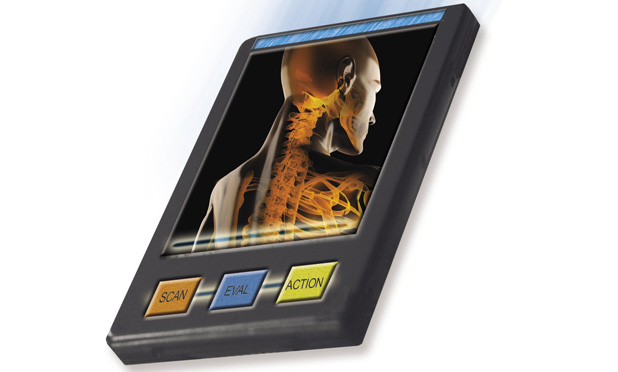
These days, you’d probably err on the side of caution and head for shore. But in the world of science fiction, you’d whip out an all-purpose diagnostic device like the well-known tricorder from Star Trek, you’d wave it over the patient, and, in a few seconds, you’d get a definitive diagnosis and maybe even some kind of treatment. If only life were really like that.
Amazingly, many aspects of that kind of all-purpose diagnostic tool have already begun to appear, piecemeal, mostly in the lab but in a few cases on the market. And suddenly it’s not quite so far-fetched to imagine integrating all of the tests that do exist, and pushing forward the ones that so far do not, into a portable package that anybody—not just a Starfleet doctor—could use to evaluate a medical emergency, make a clear diagnosis, and recommend a course of action. What once seemed like fantasy or the stuff of magic may not actually be so far away.
That’s what a group of physicians and engineers considered during a meeting in 2011 where they were brainstorming about ambitious, far-reaching, but attainable goals that might benefit from an extra kick. That is, goals that could get the boost needed to bring them to fruition by having a clear, tangible, and dramatic incentive—a substantial prize, for instance.
That vision of a multipurpose hand-held diagnostician was the springboard for the creation of what is now known as the Qualcomm Tricorder X-Prize. It was launched by the X-Prize Foundation, the same group that spurred the first all-privately funded launch of humans to the edge of space, by offering up the original X-Prize—a US$10 million purse won in October 2004 by aviation pioneer Burt Rutan and Microsoft cofounder Paul Allen with a craft called SpaceShip One. The new contest’s goals may not have quite that degree of visual drama and excitement, but they are, in a way, just as daunting as those of the original Ansari X-Prize—and potentially could have a much greater direct impact on people’s lives.
That original prize called for sending a two-person craft up to at least 100-km altitude—and then doing it again in the same craft within a fortnight, an accomplishment that even NASA hadn’t achieved. The incentive and the publicity surrounding the competition drove dozens of teams to invest a cumulative total of well over ten times the prize money trying to accomplish the goal. And it led to a whole new kind of business—commercial space flights on Virgin Galactic’s SpaceShip Two that are expected to begin this year.
And that’s just the kind of thing the X-Prize’s founder Peter Diamandis and his allies are hoping will happen to medical diagnostics as a result of this new challenge. It’s something that seems so difficult to do that it borders on impossible but whose elements are already beginning to appear at the cutting edge of technology—and whose successful implementation could forever change the face of health care.

If the effort succeeds, it could help spur the kind of convergence that sometimes happens with major advances in consumer technology—think of the iPhone, for example. Most of the individual elements needed already exist, or are well under development. But integrating them together into one small package that functions seamlessly can produce results far more dramatic than just the sum of the parts.
A Push to Integrate Data into One Comprehensive System
The prize was officially launched in January of 2012, but it wasn’t until last fall that the final roster of teams submitted their registrations. Thirty-four teams have signed up, representing everything from established biomedical companies to colleges to small start-up enterprises to a group of high school students—geographically spread from Taiwan to Slovenia to Utah. (See “Final Frontier Medical Devices,” “Nanobiosym,” and “Team
Gen Z.”) The teams will face their first big hurdle this summer: a set of evaluations that will whittle their number down to no more than ten finalists. Those ten will then square off next year in a final set of tests for the determination of the top three prizes—US$7 million, US$2 million, and US$1 million, respectively, for the top-scoring devices.
[accordion title=”Final Frontier Medical Devices”]
Two Brothers Combine Their Expertise to Tackle the Prize
Basil Harris, M.D., spends his working hours in a bustling emergency room at a hospital just outside Philadelphia. Amid the frequent chaos, pain, and frustrations of patients dealing with situations ranging from trivial to catastrophic, Harris says, as a physician who also has a doctorate in engineering, he came to realize that there had to be a better way. And when he heard about the Qualcomm Tricorder X-Prize, he recognized that was just what he’d been looking for.

“The prize project is basically what I’m doing every day,” he says. “In the ER, making diagnoses is my thing.” To compete for the prize, he says, amounts to trying to “deconstruct that into its components and program it.”
That’s where his brother, George Harris, a computer network engineer, comes in. Between the two of them, Basil Harris says, “we can do this thing!”
Essentially, Basil just wants to automate himself. “Ninety-five percent of the people who come in just want a diagnosis,” he says. But most of those patients wouldn’t have needed the care of medical professionals if they could have gotten an accurate diagnosis at home. “So many people don’t have access to the health care they need,” he says, “even in the United States, where we have the best technology, the most advanced health care system.” An automated, low-cost diagnostic system “would be a great tool to equalize health care,” he says.
Many of the diagnostic components needed for the comprehensive device envisioned by the contest do already exist, so the key is engineering and integrating them into a compact and user-friendly form. “Putting them all together in a package that meets the weight limit, that’s the challenge,” he says.
Basil acknowledges that, as a new company, Final Frontier Medical Devices, based in Paoli, Pennsylvania, formed under the impetus of the prize, may be a long-shot for the prize money, but that’s fine with him. “Whatever contribution I manage to make is something that I probably wouldn’t have had an opportunity to do otherwise,” he muses. “I think it’s great to get the little guys involved.”
[/accordion]
[accordion title=”Nanobiosym”]
Small Company with Big Plans
A strong contender for the prize with a headstart in this area is a small Cambridge-based biotech company called Nanobiosym, which has been in business for about a decade. The company was the first-place winner in last year’s Nokia X-Prize Challenge, which involved a subset of the tasks required for the new tricorder prize, and garnered them a US$525,000 cash infusion.
The company is developing a portable product called Gene-RADAR, to diagnose “any disease that can be detected through a DNA marker,” including HIV and malaria, says its founder and chief executive officer, Dr. Anita Goel. They are currently designing field trials for HIV testing in Rwanda.
The system, developed by Goel, can use just a drop of blood or saliva to make diagnoses with an accuracy comparable to those of standard lab testing, she says. It uses a nanoarray of sensors to give results in an hour—far faster than conventional lab tests—and using a mobile device.
Goel, who has both an M.D. and a Ph.D. degree in physics (from Harvard and the Massachusetts Institute of Technology, respectively), has been working in nanotechnology for 20 years, she says, to bring together the nexus of nanofabrication, mobile technology, and polymerase chain reaction analysis, hoping to change the face of medical diagnostics.
As she and her company develop the diagnostic system, “the first generation is the size of a notebook,” she says, to display the data collected by its sensors. Ultimately, the vision is to bring it down to tablet size, and eventually even to iPhone size. She sees it becoming something that “allows you to do mobile diagnostics in a point-of-care device, in homes or in clinics.”
The Qualcomm Tricorder prize, she says, is a great way for the X-Prize Foundation to attempt to mobilize the ecosystem, providing a boost to people with tangible visions for ways of transforming the way health care assessments get made. She and her company—along with a few others—were already moving in that general direction, but the prize could be “a profound accelerator,” Goel says, “allowing the future to happen faster.”
[/accordion]
[accordion title=”Team Gen Z”]
Believing in Never-Tried Solutions
Jack Andraka, who is now 16, sometimes says in interviews that his youthful optimism may have been what made the difference in his successful quest to find a new diagnostic test for pancreatic cancer that could catch the disease earlier, when it is still treatable. More experienced researchers, more familiar with the obstacles, apparently didn’t think there was enough chance of success to make the attempt.
But Andraka, who was 14 at the time, says he was motivated by the death of a family friend from the disease. The Maryland teen plunged ahead, doing his research online (starting with Wikipedia and Google), and has said that the inspiration for the idea, based on the use of carbon nanotubes and antibodies for mesothelin, a biomarker linked to the disease, came to him as he was sitting in his high school chemistry class.
One professor at Johns Hopkins University, Anirban Maitra, responded to the barrage of letters Andraka sent out and offered to help with his project, which resulted in a simple, paper-based test that can detect the disease using a small sample of blood or urine. Andraka went on to win more than US$100,000 at the Intel International Science and Engineering Fair, has been featured widely in the media, has given a TEDx Talk, and was profiled in a segment on 60 Minutes on CBS, where he said “my parents really taught me to dream big.” (His father is an engineer, his mother a physician, and his older brother was a previous national science fair winner).
Now, having already filed for a patent on the first invention and having discussions with companies about commercializing it, he is looking to broaden his diagnostic portfolio. He has organized a team called Gen Z, composed entirely of high school students and based in Bellevue, Washington, to compete in the Qualcomm Tricorder competition.
Maitra, who has served as a mentor, was quoted in The Baltimore Sun saying, “This kid is the Edison of our times. There are going to be a lot of lightbulbs coming from him.”
[/accordion]
“That’s nothing to sneeze at,” says Erik Viirre, a neurologist at the University of California San Diego medical center and the medical director of the competition. “$US10 million is a big deal, even if you’re a Fortune 500 company.” Viirre says the impact could extend far beyond the realm of the contest itself. “What this competition really does is demonstrate the breadth of technologies,” he said, technologies that are now available or are on the brink of development, which can replace or supplement existing diagnostic systems that are expensive, take a long time to carry out, and/or require specialized equipment only available in limited locations. And while the individual components of such a system may exist or be close to realization, their integration into a comprehensive system is something that might take far longer to develop without this extra push.
“The prize is a great incentive to show that these kinds of aggregated systems are feasible and will come forward,” says Viirre.
“Individual companies have tended to make single-purpose devices,” such as those for monitoring blood glucose levels or blood pressure, says Don Jones, a vice president of sponsor Qualcomm, who spearheaded the company’s underwriting of the prize. But there is potentially great power in bringing those sources of data together and using sophisticated software to analyze their collective significance. “This is going to really push along the software, the integration of the information,” he says. Such a device could “not only gather the data but advise you on what to do next.” That integration and interpretation of data, not just raw accumulation, is what’s supposed to set the new “tricorder” apart. In this way, “it becomes part of the therapy, instead of just a diagnostic number,” Jones says.

So what, exactly, does the contest require of these futuristic, nearly magical-seeming devices?
There are three broad categories on which the entries will be judged: first, diagnosing a suite of 15 specific diseases; second, providing ongoing long-term monitoring of basic vital signs such as pulse, respiration, and blood oxygen levels; and third, providing information to the user—the actual patient, not a doctor, nurse, or other professional—in a form that’s easy to use and understand.
In the head-to-head judging sessions, each device will be tested on a series of patients who have one of the listed conditions, and some who have none of them, to check for rates of successful diagnoses, as well as false positives and false negatives. Their vital-signs monitoring functions will also be tested, comparing their accuracy to that of current “gold standard” testing technologies. And finally, the usability and understandability of the user interface will be evaluated and scored by a group of nonmedical users.
Most of those capabilities exist—devices of various kinds can already diagnose most of the conditions that form the competition’s target list, though few have ever been combined into a multitest device, and many remain expensive or unwieldy. And the monitoring systems exist, but have never been integrated in the ways this contest envisions to provide long-term data collection and analysis. According to Viirre, the challenge is to integrate and to miniaturize all these functions together.
On the Starting Line
Of the 34 teams that met the requirements to register, some are starting from scratch, while others have a strong headstart having already produced, or at least substantially developed, devices that meet some subset of the required tasks. For example, both Scanadu, a company in Moffet Field, California, and Biosign, a company in Ontario, Canada, market small sensing devices that connect to a laptop computer to monitor vital signs continuously. Scanadu’s device, called Scout, monitors temperature, pulse, and blood oxymetry, while Biosign’s Pulse wave device monitors pulse and blood pressure and displays readings in real time. Tactio Health Group of Montreal, Canada, sells a whole line of fitness and health monitoring and tracking devices and apps. And Zensor, of Belfast, United Kingdom, sells wireless monitoring systems for ECG, heart rate, and respiration, among others.
On the diagnostic side, DNAmicroarray of Carlsbad, California, sells devices that can detect a wide variety of genetic markers for various diseases.
And some teams have unique approaches that may provide an edge in certain specific diagnostics. Team Gen Z of Bellevue, Washington, has its own diagnostic test for certain cancers, while Visualant of Seattle, Washington, has a proprietary system on the market called ChromaID, a handheld spectral analysis tool that it says can identify chemical compounds with great precision—for example, blood glucose levels for a diabetic patient.
Not all of the listed conditions would need to be correctly diagnosed by a given team for the team to take home the prize money, though. The winners will be those who garner the highest overall point total, based on scores from each of the many required functions. Perhaps surprisingly, delivering the data counts just as much as collecting all of those complex bits of biomedical data. “Almost half the score is the user interface,” Viirre says. “That’s the key ingredient that’s going to make the difference.”
Part of that requirement is that the device be largely self-explanatory. In the final competition, a panel of users will each have to be able to figure out how to make use of each device with only 60 min of total training time and no instruction manual to refer to—a significant challenge for a complex device. “If you have all this great technology, but the user can’t figure out how to turn it on, that’s not going to help,” says Viirre.
There are almost no requirements for what the device will look like or how big it will be, or even whether it’s one object or a whole kit of separate pieces. The only overall rule is that all of its components together can’t weigh more than 5 lb—though the organizers doubt that anyone will come close to that heft, since having a lightweight unit is likely to be a big factor in the usability scoring.
In the rules for diagnostics, it’s a bit like the Olympic gymnastic competitions, with their mix of required and optional moves: There is a set of required tests and then a whole menu of additional tests the teams can choose from, to rack up their total of 16 diagnostic functions. Thirteen of the listed conditions comprise the “core” set that each team’s system must be able to diagnose correctly. The remaining three conditions can be selected from an additional list of a dozen “elective” tests.
The diagnostic tests required span a wide range, from chronic conditions like anemia, type 2 diabetes, sleep apnea, chronic obstructive pulmonary disease, hypertension, allergies, high cholesterol and osteoporosis, to infections such as ear or urinary tract infections, strep throat, or pneumonia. They also include specific disease conditions including HIV, leukocytosis, hepatitis A, mononucleosis, and pertussis and acute conditions including stroke and atrial fibrillation.
The winning device doesn’t have to be able to diagnose all of these conditions flawlessly. After all, the contest’s organizers stress, even diagnoses made in a doctor’s office are only right about half the time, studies have shown. As with a decathlon, “You can’t necessarily be the top in the world in all the criteria,” Viirre says. “But you have to be good enough in each of them to win enough points to get the prize. It doesn’t have to be perfect, though we would love that.”
But there are some absolutes. Every device does have to be able to successfully record, over time, five basic vital signs: pulse, respiration, blood pressure, oxygen saturation, and body temperature. In addition, “the bar that everybody has to clear is safety,” Viirre says. The systems must be as noninvasive as possible and can’t expose their users to electric shocks, chemicals, or high temperatures.
Many of the teams that have signed up already have some expertise, or even products already on the market, that perform one or more of the designated functions. Some specialize in DNA testing or vital signs monitoring, or on patient information systems. Some of them may decide to join forces. “Our suspicion is there will be some interesting merger activity going on,” Viirre says. “People will say ‘I have this capability and you have that, so let’s get together’.”
A Device Could Radically Alter Health Care Systems Around the World
Integrating the different kinds of diagnostic tools into one device or assemblage could help to drive costs down radically, in much the way that the mass proliferation of computers and cell phones has slashed their costs. Today, electrocardiogram equipment costs upwards of US$10,000, Jones points out, but members of one team have already developed a system that can provide the equivalent of a 12-probe ECG in the form of a smartphone app and a set of low-cost connectors that just plugs directly into the headphone jack. “Lessons learned from consumer electronics, from phones and tablets, can now be applied to these specialized devices,” he says.
The real power of the innovation spurred by this competition is likely to be in the aggregation and interpretation of data by the system’s built-in artificial intelligence. For example, the continual logging of data, rather than occasional tests in doctors’ offices, can build up an individual database that’s never before been possible outside of a hospital setting—or even in it. “That actually is revolutionary,” Jones says. “We don’t yet know all the implications of that for the whole health care system.”
The potential market for a device capable of reliably diagnosing all these conditions could be enormous, as could its potential impact. While the initial target would be first-world early adopters who already use smart phones, the impact of such tools could ultimately be greatest in the places that have been least affected so far by the advances of modern medicine, such as low-income rural communities both domestically and in the developing world.
Viirre sees the possibility of a kind of leapfrogging of whole stages of technology by communities in the developing world. “I think the analogy is the dissemination of mobile phone technology,” he says. In many areas, people are “skipping over the whole stage of having land lines. In a directly analogous fashion, people in the developing world may end up getting their health care through a mobile device, and never go to a conventional hospital.”
But you don’t have to be in a remote village in central Africa to be able to appreciate the kind of difference such devices could make to one’s life. Anyone caring for children, or for elderly parents, can imagine the relief of not having to rush to a clinic or emergency room at 3 a.m. for a simple test to find out the difference between a routine ailment and a life-threatening condition that requires immediate professional care.
“There’s a broad range of people who will be able to make use of these systems,” Viirre says. And thanks to the push provided by the incentive of the X-Prize, that day when they will be able to enjoy the convenience and peace of mind of having a diagnostic lab right in their own medicine cabinet may come a lot sooner than it otherwise would have.