Pinpointing where healthy brain aging leaves off and dementia begins is difficult. Is a slip in memory an expected outcome for a too-busy person or a warning of something else? If an empty-nester loses the motivation to cook, is it a sign that the person is enjoying retirement after a lifetime spent cooking or an early sign of a cognitive decline?
Dementia takes hold gradually, which can mask the severity and urgency of the problem. Often, what brings a person with dementia to a doctor’s attention is a crisis, such as a fire from an unattended kitchen burner. Such events are usually preceded by several years’ worth of worrisome symptoms, but doctors lack the tools to efficiently track cognitive declines.

Now, experts are now turning to computerized tools to detect dementia in earlier stages. Early detection might bring more successful clinical trials for treatments, which, by and large, have failed for full-blown dementia; at the very least, early detection helps people prepare for what is to come.
“Even in the absence of a pill that can cure dementia, it’s very valuable to have that kind of information early on,” says Nina Silverberg, director of the Alzheimer’s Disease Centers Program at the National Institute on Aging in Bethesda, Maryland (Figure 1, right). “We really think there are a lot of opportunities to help people and their families, even if it’s just to understand what to expect and what to prepare for as the disease progresses.”
Several computerized strategies for detecting early stages of dementia are in the works. Some researchers have adapted standard cognitive tests for use on computers or tablets, which allows more reliable, flexible, and efficient assessments that may give a more accurate view of a person’s abilities. Other digital tools can pick up changes not apparent on a standard paper-and-pencil test, include sensors placed in the home to track changes in a person’s activities (see also the article “A Balancing Act”). Still other technologies enlist the help of family members, who are usually the first to notice cognitive declines, and help caregivers navigate the complex medical realities of caring for someone with dementia.

So far, these strategies haven’t yet delivered anything more sensitive than standard paper-and-pencil tests. But the potential for computerized tests to be adopted widely would allow for regular monitoring of a person’s cognitive health. Much like a blood test for cholesterol, a short cognitive test might become part of an annual checkup.
“I think many of us feel that the true remedy to the situation is to monitor an individual’s cognition longitudinally, over time,” says John Harrison (Figure 2, right) of Metis Cognition, a cognitive testing consultancy based in Warminster, United Kingdom. “If you have somebody who is reliably declining across a period of time and you can’t find any other explanation for that, then [these] seem to be the true cases we want to look at for further evaluation.”
Tracking Cognition
Dementia refers to a decline in mental abilities, including memory, language, attention, and reasoning. In the United States, 8.8% of adults 65 or older had dementia in 2012—a welcome decline compared to earlier estimates [1]. But because dementia makes it hard for people to take care of themselves, the lower figure still poses a substantial burden on healthcare systems and families.
The risk for dementia goes up with age, and there are several causes, such as stroke and other brain-damaging conditions like Parkinson’s disease. Alzheimer’s disease is the most prominent form of dementia, however, making up 60–80% of all dementia cases. Alzheimer’s disease is caused by progressive brain degeneration tied to neuron-disrupting protein clumps, but it is tricky to detect because of its gradual onset. Typically, a person complaining of memory problems to a general practitioner might receive a test that looks for cognitive impairment. For example, the Mini-Mental State Examination, a commonly used test, only registers a cognitive deficit when a person scores well below a normal average, even if a subtle decline relative to what the person was once capable of has been apparent for some time.
“I think it’s fair to say there’s widespread dissatisfaction with how things are done currently,” Harrison says. “Unfortunately, once these kinds of tests get established, they’re hard to supplant, even though most users would acknowledge that it is certainly inadequate.”
Once a person has been flagged for possible dementia, a thorough evaluation by a specialist usually follows. This might involve a brain scan, a neurologic examination, and further cognitive testing. A paper-and-pencil cognitive test would be administered and scored by a specially trained neuropsychologist. But computerized versions may improve upon this, because they can reliably score a test without a specialist.
“Cost is also a significant factor, because the most expensive element to cognitive assessment is the time of the assessor,” Harrison adds. “If people can do this remotely, or do it for themselves, then that takes a lot of the cost out of the equation.”

While placing trust in computers for cognitive assessment of computer-shy older people may seem ill advised, touchscreen technology has helped get around that. “Elderly people more easily understand how to use a tablet compared to a computer because it’s more intuitive,” says Sietske Sikkes of the Vrije University Medical Center (VUmc) in Amsterdam, The Netherlands (Figure 3, right). Sikkes is a neuropsychologist and assistant professor who works at the VUmc Alzheimer Center.
Tablet versions of cognitive tests, such as Cogstate, are now being used in research studies or specialist memory centers. Like standard tests, these measure memory as well as other domains of cognition, including attention, emotion recognition, and so-called executive functions that require multistep planning and thought organization. The tests seem to compare well to standard tests delivered by a neuropsychologist [2], and one has been adopted by a large longitudinal study of 1,000 people being monitored for subtle cognitive declines in Australia (https://aibl.csiro.au).
Computerized tests might provide a more accurate picture of a person’s cognition, for example, by avoiding practice effects. On standard paper-and-pencil tests, patients are exposed to a list of words, then asked to name as many as they can by memory. The items on the list remain the same in subsequent tests so that, with repeated testing, a patient may remember them easily. But with a computerized version, the list can be changed each time a person takes the test.
Computerized tests might also provide a better measure of cognition if they decrease a subject’s anxiety related to test taking. Tests taken at home or in a clinic with a tablet, rather than in front of a clinician with a clipboard, might get a cleaner measure of cognition. Turning tests into games may also help: one developed collaboratively by Akili Interactive Labs and the pharmaceutical company Pfizer delivers cognitive testing in the form of a fast-paced video game on a tablet. Preliminary results suggest that performance tracks with brain amyloid level [3].
Computer adaptions of tests can also haul in more data than the standard versions. For example, the clock-drawing test, used for over 50 years, asks a patient to draw an analog clock from memory. When drawn with a digitizing pen, however, the test records the pen’s movement in space and time with high accuracy, thus providing data on the effort and strategies a person uses. A study last year found that, although people with memory impairments spent less time penning the parts of the clock than did healthy controls, they paused much more between strokes, resulting in an overall increase in time to draw a clock [4]. Tiny changes in the direction of a stroke, called hooklets, may also become informative, because they are thought to reflect planning ahead for the next stroke; these may be lost in cases of cognitive decline.
Despite the promise of computerized assessments, experts agree they probably will never be sufficient to make a definitive diagnosis on their own. A clinician will always be needed to interpret the results in the context of other signs and clinical information.
“I think most clinicians would be very leery of using a completely automated assessment to make an actual diagnosis,” Silverberg says. “All methods of cognitive testing require interpretation, because a lot of performance depends on a person’s individual history and other relevant information, such as medication or current circumstances.”
Frontline Families
Enlisting family members of those with dementia can also provide sensitive measures of cognitive decline. For example, getting information from them about a person’s daily activities can indicate early mental changes, because things like banking, cooking, or shopping involve multiple steps that are cognitively complex.
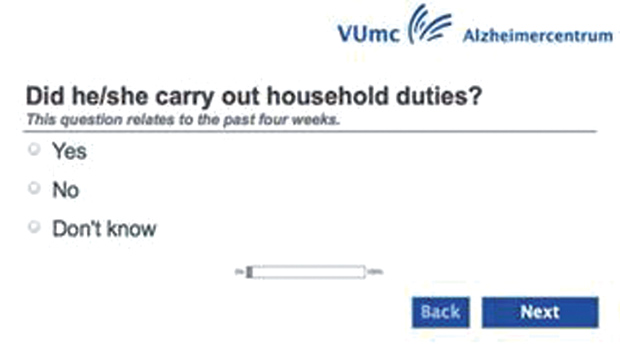
“A caregiver often notices what’s going wrong at home but also has a reference to how this person was functioning before,” says Sikkes, who developed a questionnaire for caregivers about the daily activities of someone they suspect may have a memory problem. She quickly recognized the need to computerize the questionnaire and tailor it to a person’s particular habits. For example, if a person didn’t usually do the finances in a household, then it would not be informative to learn that he or she wasn’t doing banking transactions in old age. Now, Sikkes’s test on a tablet adjusts its questions according to the answers someone gives. A shortened version of the questionnaire, taking only ten minutes to complete, has been shown to measure a range of cognitive declines (Figure 4) [5].

Changes in computer use itself can also reveal cognitive declines. A recent study found that among older people who agreed to fill out a weekly questionnaire about their activities over a year, those with mild cognitive decline began to submit their answers later in the day and needed more help to complete the questionnaire than those who remained cognitively intact [6]. Similarly, computer use declined with time by those with mild cognitive impairment, which might reflect users finding it more difficult to navigate a complex interface [7]. The same research group, based in Portland, Oregon, is also experimenting with other sensor technologies to unobtrusively measure a person’s movement patterns in the home. These can provide data about walking speed or sleep/wake cycles, which change with cognitive decline.
Another approach is to develop technologies designed to help family members sort through behavior changes that might be cause for worry versus those that are probably not, as well as when to take action. Norman Foster (Figure 5, right), a geriatric neurologist at the University of Utah in Salt Lake City and director of the Center for Alzheimer’s Care there, is developing an app for mobile devices caregivers can consult when they notice something amiss. Based on symptoms and other basic information about the loved one entered by the caregiver, the app can recommend medical follow-up or not. The app also helps caregivers judge the quality of the medical care received and navigate the next steps to take (Figure 6). “We envision Memory Care Partner [to be] like having an expert at your shoulder helping you through, step by step, the kinds of things you need to think about,” Foster says.
Educating families with this app may shorten the usually years-long process of getting help for people with dementia. Moreover, breaking down the information into digestible, relevant pieces using the app may offer an advantage over other available dementia guides.
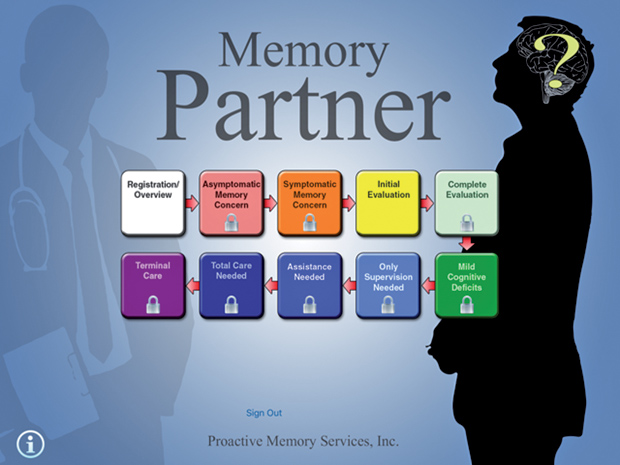
“There’s a lot of information to be given, and there’s some very good books that might be helpful if you can find them, but they’re 300 pages,” Foster says. “An app lets you go to what you need now, as well as gives you ideas of what you need that you may not know about.” For example, families often do not get help for someone until the person’s memory deficits provoke a crisis. If families had been aware of options such as senior day programs or other support systems within the community, then these problems might be averted, and people with dementia may be able to stay in their homes longer.
“By actually educating and supporting families so we could prevent problems, we are bringing preventive care to dementia care,” Foster adds.
References
- K. M. Langa, E. B. Larson, E. M. Crimmins, J. D. Faul, D. A. Levine, M. U. Kabeto, and D. R. Weir, “A comparison of the prevalence of dementia in the United States in 2000 and 2012,” JAMA Intern. Med., vol. 177, pp. 51–58. Jan. 2017.
- D. M. Rentz, “Validating use of technology for cognitive test assessment,” EBioMedicine, vol. 11, pp. 23–24. Sept. 2016.
- Business Wire. (2016, Dec. 9). Akili and Pfizer present positive data from digital biomarker study to detect subtle cognitive changes in healthy subjects at risk of developing Alzheimer’s disease. [Online].
- W. Souillard-Mandar, R. Davis, C. Rudin, R. Au, D. J. Libon, R. Swenson, C. C. Price, M. Lamar, and D. L. Penney, “Learning classification models of cognitive conditions from subtle behaviors in the digital Clock Drawing Test,” Mach. Learn., vol. 102, no. 3, pp. 393–441. Mar. 2016.
- R. J. Jutten, C. F. W. Peeters, S. M. J. Leijdesdorff, P. J. Visser, A. B. Maier, C. B. Terwee, P. Scheltens, and S. A. M. Sikkes. (2016, Oct. 21). Detecting functional decline from normal ageing to dementia: development and validation of a short version of the Amsterdam IADL questionnaire. [Online].
- A. Seelye, N. Mattek, D. B. Howieson, D. Austin, K. Wild, H. H. Dodge, and J. A. Kaye, “Embedded online questionnaire measures are sensitive to identifying mild cognitive impairment,” Alzheimer Dis. Assoc. Disord., vol. 30, no. 2, pp. 152–159. Apr.– June 2016.
- J. Kaye, N. Mattek, H. H. Dodge, I. Campbell, T. Hayes, D. Austin, W. Hatt, K. Wild, H. Jimison, and M. Pavel, “Unobtrusive measurement of daily computer use to detect mild cognitive impairment,” Alzheimers Dementia, vol. 10, no. 1, pp. 10–17. Jan. 2014.


