A few years ago, the average person had no idea what the microbiome was, but now it is bantered about on quasi-medical talk shows, social media, and blogs almost as though it were the savior of human health: change your microbiome, change your world!
Researchers and health professionals, of course, have a different view. Yes, the microbiome is a diverse and highly individualized collection of bacteria and other microorganisms that live on or in humans, but beyond that general statement, they see a great deal of work to be done to understand exactly how the microbiome influences health and an even longer path before they can use that knowledge to any great extent for reducing the risk of or possibly treating certain illnesses. Science needs a fuller understanding of the microbes that are present, their interactions with other microbes, and their individual and collective functions before the microbiome’s clinical potential can be realized.
Who’s There?

Much of the initial research on the microbiome has been in identifying its inhabitants: which organisms live on the skin, in the mouth, inside the digestive system, within the vagina, and in the nose? That has led to an ever-increasing number of scientific papers, as researchers determine the species, sequence their genomes, and establish the function of their genes. Even so, while we have learned a considerable amount about the microbiome, much remains unknown.
“There is still a lot of component-level information missing, including much microbial dark matter—species that we just don’t know and did not yet sequence,” says Elhanan Borenstein (Figure 1, right), associate professor in the Department of Genome Sciences at the University of Washington. “Even for the species that have been identified and sequenced, in many cases, we only know the function of a fraction of their genes. There is definitely still a huge need for continued work on identifying the elements of the system.”
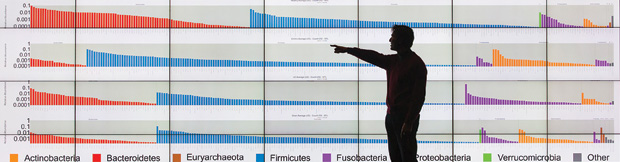
One effort to discover the many players in the microbiome and how they differ from person to person is the American Gut Project [1]. Self-described as “one of the largest crowdsourced, citizen-science projects in the country,” the venture encourages individuals to send in microbiome samples—e.g., a fecal sample or tongue (Figure 2), forehead, or palm swab—along with such lifestyle information as diet and exercise routine. For a monetary contribution, the individual receives information about the microbes present in the sample and how the microbiome matches up with other people’s samples.

“What makes this project unique is its scale,” says Rob Knight (Figure 3), cofounder of the American Gut Project as well as a professor of pediatrics and of computer science and engineering at the University of California, San Diego, and director of the Center for Microbiome Innovation there. He notes that the project has raised more than US$1.5 million and has released the data for 10,000 samples. On the research side, the microbial composition and lifestyle information for each sample goes through an open-access data analysis model that Knight’s group helped pioneer and becomes available in a privacy-protected database that researchers can access at no charge (Figure 4). “Anyone at a government agency, such as the U.S. Environmental Protection Agency or Centers for Disease Control and Prevention, or a researcher, educator, or student can use it as a resource,” he says.
For his own part, Knight is interested in the impact of lifestyle on the microbiome. “There’s a whole body of research literature that shows that the microbiome has statistically significant associations with all kinds of things, such as how much you weigh, how much you eat, how much you exercise, how much you sleep, and what drugs you take, but we don’t have a good sense of which factors have large or small effects, and we don’t have a sense about how factors may interact with one another.” To further investigate, his lab is using a variety of techniques, notably principal coordinates analysis and the UniFrac distance matrix (devised by his group in 2005), that together help to compare biological communities and visualize similarities and dissimilarities in data.
“We’ve made huge progress, but we’re still very near the beginning,” Knight continues. A current emphasis is to broaden the participant pool in the American Gut Project to include more people from low-income groups, certain underrepresented ethnicities, and immigrant populations. Immigrant populations would be especially interesting to explore because country of origin can influence the microbiome’s composition and that, in turn, may affect disease susceptibility, he explains. Knight would also like to increase coverage of individuals with certain health conditions, such as children with autism and adults with Parkinson’s or Alzheimer’s disease. That would not only enlarge the scope of the data the American Gut Project is collecting but could inform research studies. Says Knight, “That’s very exciting.”
What’s Going On?
Many researchers are now standing on the growing mountain of data related to the microbiome’s components and trying to devise methods for mining and analyzing these data. However, some researchers aim to move beyond examining the microbiome’s components and toward studying the microbiome as a whole. Borenstein’s group is one of those taking a systems-biology approach to microbiome research and analyzing the microbiome as an ecosystem. “We are all captivated when we hear about an explorer who is traveling to a remote location of the planet and finding interesting and exciting ecosystems,” he says. “Now, we are realizing that we have equally (if not more) amazing ecosystems inside and on our bodies. There is something intriguing about the concept of humans as walking, talking habitats for a complex and diverse ecosystem that is actually affecting our health in many different ways.”
Although scientists are still focused primarily on studying and cataloging the many components of the microbiome, including which species are there, which genes are expressed, and which proteins and metabolites are present, Borenstein contends that a glaring omission remains: a comprehensive systems-level view of how all those different elements work together. “When you’re studying a system, especially one as complex as the human microbiome, the most challenging and exciting thing to understand is how all those elements that you’ve identified jointly work to create an emergent behavior observed at the system level.”

Such a broad view is pivotal, especially if researchers hope to exploit the microbiome for possible clinical applications, says David Relman, Thomas C. and Joan M. Merigan Professor in the Department of Medicine and the Department of Microbiology and Immunology at Stanford University (Figure 5, right). “We need a more integrative understanding of how all of these organisms work together as a single unit, but I’m still seeing resistance to the idea, because a fair number of researchers want to reduce these communities to the sum of a bunch of parts: growing each of the individual members in the laboratory, characterizing them as individuals, and then maybe reconstructing simple communities using these cultivated members. It tends to be a reductionist approach, and that kind of approach will only get us so far.” Relman asserts that a more progressive and productive path forward is one that concentrates on understanding interactions and communities as a whole.
Borenstein is tackling that challenge by trying to develop computational models of the microbiome (Figure 6), which he believes are essential if researchers hope to exploit the microbiome’s potential for clinical applications. He remarks, “If we ever want to get to a point where we can truly design personalized and tailored microbiome-based interventions, we need to have a model of the microbiome that will allow us to generate hypotheses as to what kind of interventions might work and to rationally design specific compositions of species that might be able to carry out some desired metabolic task or synthesize a required vitamin.”

Specifically, Borenstein and his group aspire to model the metabolism of the microbiome. “This is a process that we know how to model well for a single species, but we need to move forward and model a system with two species—or ten species or 1,000 species—as well as the interactions among these species to capture the complexities of the microbiome. Hopefully, by doing that, we will ultimately obtain a predictive, comprehensive, system-level model of the microbiome, which will allow us then to make accurate predictions about how the microbiome will behave in different settings.”
Complementary to this model development, Borenstein’s group is also working on computational methods to integrate different omics, such as those that measure metabolites and gene-expression levels. “The idea is not just to identify statistical associations—for instance, finding that when the concentration of a certain metabolite is high, the abundance of some species is low,” Borenstein says. “Instead, it’s really about trying to integrate such data using a mechanistic model that will allow us to understand why this metabolite’s concentration is high when this species’ abundance is low, or more generally how ecological shifts in the composition of species in the microbiome are translating into shifts in its metabolic capacity and function.”
Borenstein and his group have already gained some insights. One study, published earlier this year [2], explored the use of a series of simple models and a straightforward framework to predict the concentration of metabolites, based on the composition of species in the microbiome and on available genomic data. He says, “We weren’t optimistic that it would work, but it turns out that even if we apply this simple framework, we are able to explain observed variation in a large number of metabolites across samples. That suggests that, in some cases, there’s a strong enough signal to mechanistically understand why a specific community produces a specific metabolite and another community produces another.” Other recent work introduced a new framework for characterizing strain-level genetic variations in the microbiome and revealed extensive and widespread differences in strains—in addition to differences in microbial species—among individuals [3].
While Borenstein is happy to talk about his group’s successes, he is the first to concede that modeling a system as complex as the microbiome is complicated and rather daunting. “We know it’s not something we’ll fully accomplish in the next few years, but we need to start building the infrastructure to do that [4]. Otherwise we’ll never get this done,” he says. “That’s why we’re trying to come up with the building blocks, technologies, and algorithms to see what a model like this would look like. We also know it would likely not be one simple modeling solution.” He anticipates a need to integrate many different types of techniques, data, and frameworks to discern the different processes in the microbiome and adds, “What we’re trying to do is to build those steps toward a large-scale model.”
Relman’s approach to the microbiome is one of temporal dynamics: measuring microbial community attributes, including functions, and learning how these attributes are preserved over time, especially in the face of disturbance. The work involves longitudinal studies of healthy subjects composed of three phases: 1) monitoring microbial communities at multiple sites around the body and over a sufficient period of time in the absence of overt disturbance to get a good picture of what the undisturbed state looks like, 2) exposing the subject’s microbial communities to one of several kinds of disturbances and assessing that impact on the microbiome, and 3) assessing the ability of the microbiome to recover previous functions and seeking to understand the basis for resilience [5], [6].
Such longitudinal studies have included antibiotics as a selective chemical disturbance; a colonic cleanout (the procedure done before a colonoscopy) as a flash-flood type of disturbance, because it mechanically washes away microbes; and a droughtlike disturbance, in which subjects take a medication that makes the mouth dry [7]. The first two disturbances are examined via fecal analyses and the latter through samples taken from tooth surfaces. Relman explains, “The idea is that for any one disturbance, there might be specific kinds of rules that determine whether a community will be stable or destabilized, but that there also may be more general rules that apply to many different kinds of disturbance.”
Relman’s group is gathering data now and has formed some impressions and hypotheses about what happens to the microbiome over time, but defining sets of rules is still a way off. “I think there are going to be several kinds of challenges,” he explains. “One is, of course, to exploit these multiple forms of data to the greatest degree possible, because we’re measuring taxa, and also genes, genomes, transcripts, proteins, and metabolites. We want to be able to look at many attributes of these communities in a thoughtful and holistic way with respect to time. Meanwhile, time-series analysis is a field of analytical theory and practice worthy of attention unto itself.”
Another challenge is in the assessment of microbial community-wide functions. Relman suggests that the genomic and postgenomic microbiota features most commonly measured are only surrogates for function and “do not adequately reflect the synergistic activities of microbial community members, as well as their net effects on their host.” A third challenge lies in the design of an effective longitudinal study, according to Relman. “There are some major issues surrounding selection of human subjects, collection of relevant clinical, demographic, and environmental data about them, and how to control for or even recognize some of the possible compounding factors that might skew the data in one direction or another without you even knowing it.”
For now, Relman is planning a careful examination of certain population subsets to help inform his study design.
How Do We Benefit?
Although understanding of the microbiome has grown enormously over the past decade and continues to do so, the field is nascent when it comes to exploiting the microbiome’s potential for clinical applications. Even so, work is advancing on many fronts, including that focusing on illnesses, notably inflammatory bowel diseases (see the article “Omics Tech, Gut-on-a- Chip, and Bacterial Engineering” on page 9).
For Borenstein’s part, he doesn’t see a comprehensive computer-modeling framework making its way into the clinical setting over the next few years. “Having an off-the-shelf system that takes information about a disease, host genetics, and the composition of the microbiome and computationally suggests beneficial microbiome changes will not be available for a while yet. That said, it doesn’t have to be all or nothing. There could be partial solutions that may be able to accurately model specific processes in specific diseases, and that could become available in the shorter term.”
Regardless of how it makes its entrance, Borenstein predicts that the microbiome will have a clear influence in the clinic of the future. “I do believe that the next couple of decades will see dramatic changes in the way that we think about health and medicine, changes that take into account the microbiome and that promote therapies that we never considered before, as well as an understanding of human physiology, nutrition, and disease that is perhaps very different from our current understanding.”
Relman is also confident that the microbiome will be recognized as an intimately interwoven factor in human health but asserts that it likely will not be the sole explanatory factor for why one person is healthy and another is sick, because other fundamentally important forces are also in play. He adds with a laugh, “It’s a note of caution that we should definitely get excited about the microbiome’s potential, but not too excited.”
References
- American Gut Project. [Online].
- C. Noecker, A. Eng, S. Srinivasan, C. M. Theriot, V. I. B. Young, J. K. Jansson, D. N. Fredricks, and E. A. Borenstein, “Metabolic model-based integration of microbiome taxonomic and metabolomic profiles elucidates mechanistic links between ecological and metabolic variation,” mSyst., vol. 1, no. 1, pp. e00013–e00015, Jan.–Feb. 2015.
- S. Greenblum, R. Carr, and E. Borenstein, “Extensive strain-level copy-number variation across human microbiome species,” Cell, vol. 160, no. 4, pp. 583–594, Feb. 2015.
- A. Eng and E. Borenstein, “An algorithm for designing minimal microbial communities with desired metabolic capacities,” Bioinformatics, vol. 32, no. 13, pp. 2008–2016.
- E. K. Costello, K. Stagaman, L. Dethlefsen, B. J. Bohannan, and D. A. Relman, “The application of ecological theory toward an understanding of the human microbiome,” Sci., vol. 336, no. 6086, pp. 1255–1262, June 2012.
- David Relman Laboratory. Dynamics of the human microbiota. [Online].
- hyposalivation.org. (2016). Saliva and human oral health [Online].



