Welcome to the era of cognitive health care, a new partnership between human beings and technology with the goal of transforming health care on a global scale.
Cognitive systems that understand, reason, and learn are helping people expand their knowledge base, improve their productivity, and deepen their expertise. With cognitive computing, we can now see health data that were previously inaccessible, and we can impact the field of health care more than we ever thought possible. Humans generate an enormous amount of health-related data, from our personal fitness trackers and mobile apps to electronic medical records and genomic and clinical research. Unfortunately, much of this information is discarded or underutilized, and a majority of patients do not even have access to their own data.
Imagine a world where healthcare professionals could harness the best expertise from world-class doctors to reach the most remote regions and match more patients to life-saving clinical trials. The era of cognitive health care will bring together individual and clinical research and social data from a diverse range of healthcare sources to redefine a patient’s path to better health.
Toward Personalized Care
The future of health care is focused on giving individuals a complete picture of the many factors that affect their health. Seeking the same conveniences they access in other industries, today’s patients want personalized, transparent, integrated, and high-quality care. To provide the experience empowered consumers demand, healthcare organizations need better ways to tap into and analyze health information in real time. Real-time analysis allows doctors, researchers, insurers, case workers, and other stakeholders to make the most informed decisions, while also providing patients greater control over their own care. However, this complex coordination requires significant time and can tax the resources of even the most versatile organizations.
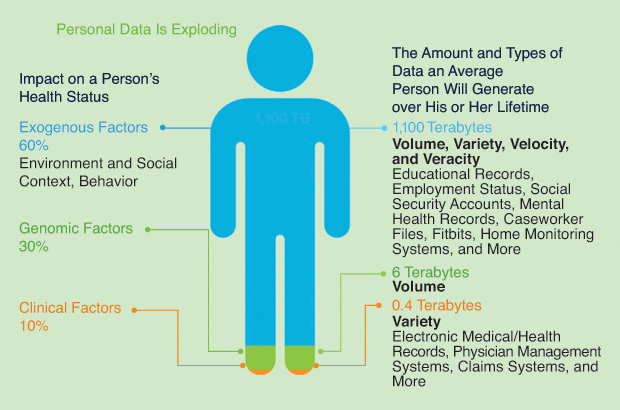
Like any other industry, health care is being disrupted and transformed by an exponential growth in data. More healthcare data are produced today than at any other time in history. As shown in Figure 1, volumes of health-related data from a variety of sources have created data management and integration challenges. By 2020, the footprint of medical data will double every 73 days: an estimated 80% of this data will be unstructured. While medical professionals have access to an abundance of data, the volume is simply too significant for them to consume, analyze, and apply in ways that are meaningful for patients. In addition, the growth and pace of medical research, clinical trials, and treatment options are staggering. It is estimated that it would take a doctor 150 hours each week to read every piece of content published in his or her field of interest.
These growing pools of healthcare-related information, including electronic health records, clinical research, pathology reports, lab results, radiology images, voice recordings, and exogenous data, are difficult to share because they are fragmented. In addition, these information sources do not readily incorporate critical information about an individual’s nonclinical conditions, which may have a strong bearing on health. As a result, patients and their healthcare providers are forced to make decisions based on a limited pool of evidence. This problem, as seen in Figure 2, is expected to get worse: between electronic medical records, digitized diagnostics, and wearable medical devices, the average person will likely leave a trail of more than one million gigabytes of health-related data in his or her lifetime— the equivalent of about 300 million books.
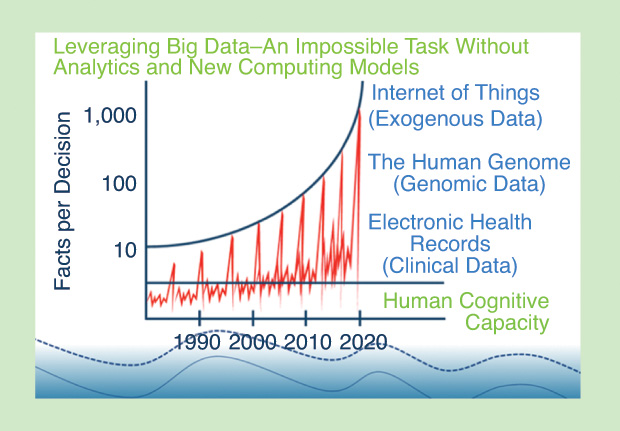
Cognitive computing constitutes a new evolution of algorithms and systems featuring natural language processing (NLP), hypothesis generation and evaluation, and dynamic learning. Cognitive computing can rapidly and intelligently parse through disparate data to help coordinate care. Cognitive systems can augment efforts to improve health information sharing for better patient outcomes. Advances in data availability, connectivity, and cognitive computing are allowing doctors, researchers, and other health professionals to personalize care with greater diagnostic certainty. This enables healthcare providers to make better, faster, and more cost-effective decisions, and it provides individuals with the insights they need to understand their health and receive truly personalized care. There is a vast amount of meaningful data that can help tell the whole story about an individual’s health and needs.
Based on machine learning, cognitive computing involves a category of analytics that are taught or learned. It is distinct from programmed or rules-based analytics and computing. Cognitive computing systems continually acquire knowledge from the data fed into them by mining these diverse data for pertinent streams of information. These systems themselves refine the way they look for patterns as well as the way they process data so they become capable of anticipating new problems and modeling possible solutions. Cognitive computing also involves self-learning systems that use data mining, pattern recognition, and NLP to mimic the way the human brain works. Cognitive computing is used in numerous artificial intelligence (AI) applications, including expert systems, natural language programming, neural networks, robotics, and virtual reality. The goal of cognitive computing is to create automated information technology systems capable of solving problems without requiring human assistance. In five years, machines will emulate human senses, each in their own special way.
Why Cognitive Computing in Health Care?
The promise of cognitive computing is driving interest and investment in the technology and its application across almost every field: for example, it has enabled autonomous vehicles, marketers are using it to better understand and target their audiences, and investors are employing it to improve their research and analysis. However, the greatest disruption resulting from the rise of cognitive computing will likely occur in the field of health care. New AI systems that augment the role of doctors and engage patients will expand access, lower costs, and, most importantly, improve outcomes—ultimately making our world healthier and happier. From advanced personal training to cancer treatment, from clinical trial matching to insulin pumps that think, cognitive computing and AI are transforming the way organizations impact health and wellness.
- Cognitive computing enables researchers to uncover new insights in relationships among genes, proteins, pathways, phenotypes, and diseases.
- Cognitive computing helps identify the most critical attributes of a patient case and can provide easy-to-consume summaries for both patients and healthcare providers.
- Cognitive capabilities have been used in clinical trial matching to optimize patient selection and recruitment.
- Cognitive computing can assist in creating individualized treatment plans and thereby enhance the patient and physician experience.
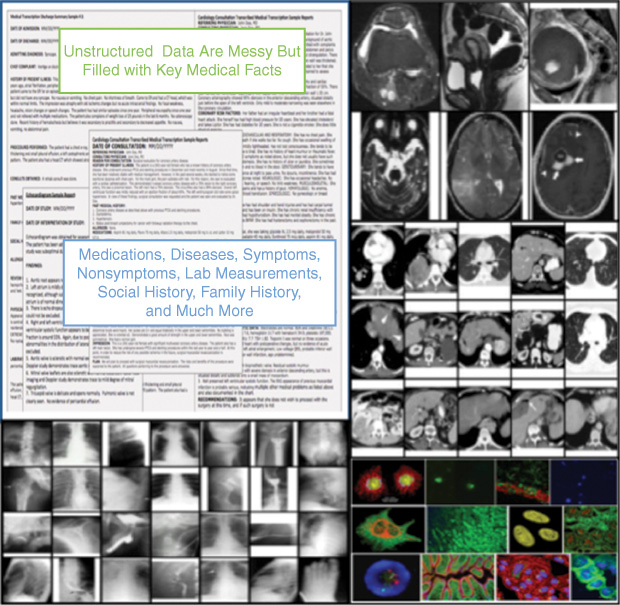
As shown in Figure 3, the field of medicine is primed for cognitive computing because it generates a substantial volume of unstructured data: text from research papers, doctors’ notes, and medical textbooks; images from X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI); and, as more people have some or all of their genome mapped, cellular- level assays to help understand disease. Obviously, not all data like these can be reduced to a number in a database (like a blood pressure reading). However, cognitive tools such as NLP and automated image analysis will unlock such unstructured data and make them useful to advance research and education, inform diagnosis and treatment decisions, and improve communication between patients and their healthcare providers.
The transformation of the healthcare industry is occurring not only at the point of care. Indexing the diverse wealth of knowledge found in medical textbooks, research papers, clinical studies, and the human genome will benefit education and research in important ways, as well. Strong health education institutions in the developed world produce competent, experienced, and skilled clinicians, but this is not true for the developing world. Providing better access to the expertise of the global community will help doctors without a path to top-notch medical schools get the training they need to serve their patients. Greater availability of expertise could change medical schools around the world. With knowledge constantly at their fingertips, students can reduce the focus on understanding minute details of biological and chemical processes and be empowered to practice the soft-skills needed to connect with patients.
Better access to the mass of global medical knowledge will also empower researchers as never before. Cognitive computing systems can evaluate thousands of research papers to uncover new insights into relationships among genes, proteins, pathways, phenotypes, and diseases. No longer having to spend countless hours reading, trying to find needles in haystacks of papers, researchers will be able to focus on the most promising leads, accelerating the pace of breakthrough discoveries.
Every corner of medicine will work with unstructured data in new ways.
- Computer systems can help attention-fatigued radiologists quickly find the anomalies of interest in images. There is less risk of missing something or of wasting time searching for an anomaly that does not exist.
- Patients will be able to send updates to their doctors through speech or text, anytime and from anywhere. These messages can be analyzed to find signs of progressing or deteriorating health, and a doctor will be notified if any patterns suggest intervention.
- Research has already shown that analyzing patients’ descriptions of symptoms in the context of their demographics can help diagnose cardiovascular disease. In the case of illnesses that affect the mind, patients’ communications can provide clues about what is wrong or show improving or declining cognitive functions over time. The more sources of information computers understand, the more they can help us make better decisions.
IBM’s Cognitive Computing Effort in Health Care
IBM approached the long-standing research problem of opendomain question answering (QA) through the television game show Jeopardy! with a massively parallel, probabilistic, evidence-based architecture known as Watson. The Watson project shapes a grand challenge in computer science, aiming to illustrate how the wide and growing accessibility of natural language content and the integration and advancement of NLP, information retrieval, machine learning, knowledge representation and reasoning, and massively parallel computation can drive open-domain, automatic, QA technology to a point where it clearly and consistently rivals the best human performance.
Based on its Jeopardy! success, IBM scientists and engineers customized and delivered Watson as the first commercially available cognitive computing capability, a capability that represents a new era in computing. The system, delivered through the cloud, analyzes high volumes of data, understands complex questions posed in natural language, and proposes evidence-based answers. Watson continuously learns, gaining value knowledge over time from each interaction with a human.
IBM Watson Health and the Watson Health Cloud
In April 2015, the company launched IBM Watson Health and the Watson Health Cloud platform. The mission of this new unit is to improve the ability of doctors, researchers, and insurers to innovate by surfacing insights from the massive amount of personal health data created and shared daily. The Watson Health Cloud allows this information to be deidentified, shared, and combined with a dynamic, constantly growing, and aggregated view of clinical, research, and social healthcare data.
IBM has partnered with various academic, research, and private institutions to apply Watson and cognitive computing in solving the most challenging and pressing problems in patient care. For instance, IBM is working with researchers, clinicians, and cancer institutions to apply Watson technology to the data challenges of cancer treatment through partnerships with New York’s Memorial Sloan-Kettering Cancer Center and the MD Anderson Cancer Center at the University of Texas, Austin. At Minnesota’s Mayo Clinic, Watson is helping doctors match patients to relevant clinical trials, and 16 leading cancer institutes are working with Watson to help doctors translate DNA insights into personalized treatment options for patients. Researchers from Baylor College of Medicine in Texas are using Watson to develop solutions for automated hypothesis generation. The American Diabetes Association and IBM Watson Health recently announced a long-term collaboration to bring together the cognitive computing power of Watson and the association’s enormous repository of clinical and research data. As part of the collaboration, Watson will be trained to understand diabetes data so that it can identify potential risk factors and create evidence-based, confidence-ran ked recommendations for a range of healthcare decisions.
IBM has also partnered with Apple, Johnson & Johnson, and Medtronic to make it easier for healthcare organizations to store and analyze patient data using Watson’s cognitive capabilities, creating new health-based offerings that leverage information collected from personal health, medical, and fitness devices to provide better insights, real-time feedback, and recommendations that can improve everything from personal health and wellness to acute and chronic care.
IBM Watson for Clinical Trial Matching
Clinical trials are at the heart of all medical advances in preventing, detecting, and treating cancer. However, no two people and no two cancers are alike. The current process for trial matching is conducted via clinical coordinators who sort through patient records and match patients to a given study protocol. But a given protocol has, on average, 46 requirements. These criteria can include a certain genetic marker, age range, tumor stage, and/or treatment history. The huge range of data to be matched makes this a complex and difficult task to conduct without advanced analytics capabilities.
This is where IBM Watson and cognitive computing are able to help: a clinician can submit a particular patient’s health information; then, Watson analyzes the patient’s data against clinical trial databases and offers feedback to the physician regarding the patient’s eligibility for specific clinical studies. The need for this approach will continue to grow as trials increasingly factor in genetic components and personalized medicine continues to come to the forefront, which will require targeting specific and perhaps small groups of patients who may have no natural affiliation, such as those in orphan disease groups.
Watson will support a higher level of personalized patient care by enabling individual health information to be securely connected with a vast array of clinical trials. Through highly precise matching of more patients with appropriate clinical trials, Watson will help advance scientific discovery and thus the health of whole communities. For example, cognitive clinical trial matching can help doctors bring more patients and researchers together in an effort to speed the development of new cancer therapies and extend hope to patients.
Virtual Cancer Patient Health Advisor
More than 1.6 million Americans are diagnosed with cancer each year, so the challenge of finding the right information for each person to manage his or her disease often presents a significant hurdle. Filtering countless health websites for relevant, accurate, and trustworthy information is daunting, and it becomes even more difficult to draw insights from multiple sources. This is where Watson’s cognitive capabilities may help.
Combining the depth and breadth of cancer information from American Cancer Society (ACS) data sources with the power of IBM Watson’s cognitive technology, the ACS and IBM are partnering to create a patient “virtual advisor.” The virtual advisor will mine the ACS’s cancer.org website, which contains some 14,000 pages of detailed information on more than 70 cancer topics, including healthy lifestyles, risk reduction, and early detection. Watson will also ingest the ACS National Cancer Information Center’s de-identified and aggregated patient data regarding self-management, support groups, health/wellness activities, and cancer education. Once developed, the advisor will anticipate the needs of people with different types of cancers, at different stages of disease, and at various points in treatment. It will be dynamic and become increasingly personalized as individuals engage with it, effectively becoming smarter each time it is used.
The ACS and IBM also envision incorporating Watson’s voice recognition and NLP technology, enabling users to ask questions and receive audible responses. For example, a person with breast cancer experiencing unusual levels of pain could ask what might be causing her pain. The virtual advisor will be designed to respond with information on symptoms and self-management options associated with her current and future phases of treatment, based on the experiences of women with similar characteristics. Because the virtual advisor learns from each engagement, a patient will receive customized options based on preferences Watson has learned, such as that a person prefers online peer support groups to telephone calls from a health coach.
Looking Forward
For most of history, health care has been delivered according to a one-size-fits-all approach, with diagnostic and treatment decisions made based on the “average” patient. Understandably, outcomes can vary greatly among populations. By incorporating more information about individual patients, their history, environments, and genetics into each medical decision, medical professionals can make the best choice for each personalized patient rather than an average one. Cognitive computing offers this path to more individualized medical decisions. And, while even large teams of doctors cannot make sense of hundreds of data points across millions of patients, machine learning is capable of improving health care with more types of data and more cases to process.
Cognitive healthcare decision assistance has the twin benefits of improving patient health and reducing the costs of missed diagnoses and suboptimal treatment plans. Ultimately, the application of cognitive computing in healthcare is about producing superior, best-practice, decision-relevant information for everyone in the health system. For healthcare practitioners, this means being able to provide more personalized care to patients with greater diagnostic certainty and best-practice treatment options based on the world’s latest medical evidence.