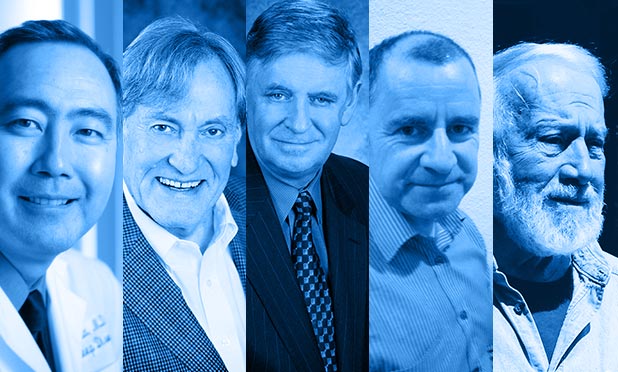
Five of the top researchers in the field of sleep research, diagnostics and treatment were invited by IEEE Pulse to discuss recent developments in the field, including where the technology stands now and where we can expect further progress in coming years. The panel consists of Allan Pack, a professor at the University of Pennsylvania School of Medicine and recognized expert on sleep disorders and genetics; Clete Kushida, a sleep researcher and clinician and former president of the American Academy of Sleep Medicine; Philip Westbrook, chief medical officer for Ventus Medical and clinical professor of medicine at UCLA; Conor Heneghan, an associate professor at the University of California at Davis and chief engineer at ResMed Sensor Technologies in Dublin, Ireland; and John Remmers, chief medical officer for Zephyr Sleep Technologies Inc. and founder of the Foothills Sleep Laboratory in Calgary, Canada.
[accordion title=”Participant Biographies”]

Conor Heneghan
Conor Heneghan is an associate professor in the School of Electric, Electronics and Communications Engineering at the University of California at Davis. He received his PhD from Columbia University in 1995. Before joining UCD in 1997, he worked as a post-doctoral research scientist at Boston University’s Department of Electrical and Computer Engineering, and as Director of Tele-Informatics at The New York Eye and Ear Infirmary. He co-founded BiancaMed in 2003, a UCD campus company which was acquired by ResMed in 2011. He continues to act as chief engineer in ResMed Sensor Technologies in Dublin. His research and professional interests are in biomedical signal processing in the areas of sleep and respiration monitoring.

Clete Kushida
Dr. Clete A. Kushida is a leading sleep medicine clinician and sleep scientist. He was the 2009-2010 President of the American Academy of Sleep Medicine (AASM), and is an associate professor in the Department of Psychiatry and Behavioral Sciences at the Stanford University Medical Center, acting medical director of the Stanford Sleep Disorders Clinic, and director of the Stanford University Center for Human Sleep Research. He received a doctorate in neurosciences/biopsychology from the University of Chicago in 1986, and a medical degree from the University of Chicago School of Medicine in 1990.

Allan Pack
Dr. Allan I. Pack is a professor of medicine at the University of Pennsylvania Perelman School of Medicine. He pursues research on genetics/genomics of sleep and its disorders. His laboratory is conducting studies in Drosophila and mice and translating these findings to humans. A particular focus of Dr. Pack’s work is to evaluate the genetic determinants of sleep homeostasis. Studies are ongoing to evaluate molecular mechanisms of sleepiness and sleep promotion using both hypothesis-driven and discovery science. Dr. Pack’s clinical expertise is in sleep disorders with a particular focus on diagnosis and management of obstructive sleep apnea. He is internationally recognized for his expertise in this area and has been listed in the Best Doctors in the United States and in the Philadelphia region (Philadelphia Magazine).

John Remmers
John Remmers, M.D., is an expert in the field of snoring and sleep apnea. He was the first to demonstrate that sleep apnea is due to an anatomical narrowing of the pharynx. He went on to develop various technologies and medical devices to treat this condition, most notably the Tranquility CPAP® (continuous positive airway pressure) device. He is the Chief Medical Officer for Zephyr Sleep Technologies Inc. and is clinically active at the Southern Alberta Sleep Centre and the Foothills Sleep Laboratory in Calgary, Canada, which he founded in 1984.

Philip Westbrook
Philip R. Westbrook, M.D., serves as the Chief Medical Officer of Ventus Medical, Inc. and has been the Chief Medical Officer of Advanced Brain Monitoring Inc. since 2001. Dr. Westbrook is Clinical Professor of Medicine at UCLA and has been actively involved in the professional organizations associated with sleep disorders. He served as President of the American Sleep Disorder Association (ASDA and of Pacific Sleep Medicine. He has been a sleep medicine leader for over 35 years, and he established the sleep disorders centers of the Mayo Clinic and Cedras Sinai Medical Center He received his MD from Stanford University School of Medicine.
[/accordion]
IEEE Pulse: Could you describe the recent progress in the field of diagnostics for sleep disorders, and what are currently the best methods and technologies?
Kushida: Well, in terms of sleep apnea, there’s a shift toward home-based testing. So now, patients with fairly straightforward sleep apnea—meaning that they don’t have significant co-morbidities, they’re probably young and healthy—those types of patients more frequently are being diagnosed with home-based sleep testing. Lab studies are now mostly for patients who have co-morbidities such as heart problems or respiratory problems, or even brain-related problems like stroke. Those cases of complex sleep disorders, including central sleep apnea, which is caused by brain or heart related issues, will have lab studies.
Heneghan: The gold standard for many years was the lab-based system but since about 2000 people have been trying to simplify that, to both lower the cost and expand the access to care. It’s now progressed to the point that we would get maybe 30 percent of the tests right now in the United States conducted in the home environment, and effectively what they’ve done is taken a limited set of the signals from the lab-based tests. I think the net effect in terms of clinical care has been to increase the number of tests done and make it a bit easier for people to get sleep testing.
There can be, psychologically, quite a high barrier to going into the hospital for the night, whereas the in-home test, for people who are reluctant to go into the hospital, gives them access to a diagnostic test they otherwise might have avoided or put off for a long time. So the overall effect has probably been quite positive for the clinical outcomes.
Westbrook: For many years the diagnostic procedure of choice involved recording sleep (with an electroencephalogram, or EEG). With sleep apnea and its subtypes, that required the patient being brought into the laboratory and hooked up to an EEG and recorded all night, and the field of sleep medicine became a sort of one-procedure specialty. But that technology evolved to the point that you could pack what used to be a refrigerator-size recorder into something about the size of an iPhone, and with that we were able to apply recorders and sensors to the patient and send them home with it, or mail the recorder to the home and have them apply it themselves, and record everything we needed to know, in the patient’s home, unattended.
That move was strongly resisted by a lot of people in sleep medicine who were invested in the old technology. But it has become more and more accepted, particularly when it was shown that it cut the costs dramatically.
Pack: The equipment is getting better and better and allows us to get more data in the home. I think we’re moving much more into home-based, not just in terms of diagnosis, but also from the point of view of follow up.
We can use wireless and mobile data, and the patients themselves can sign up and they can get their own compliance data from the Continuous Positive Airway Pressure (CPAP) on their iPhones. We see when they’re using it, to the minute. And there’s data to show that if you feed back data to the client on compliance, you see a significant enhancement in adherence.
In certain areas, it’s particularly important. For example, sleep apnea is very common in commercial drivers. So there’s a push towards getting drivers diagnosed and treated. And we can treat those things, so it’s not punitive, it’s about getting them diagnosed and treated.
Remmers: CPAP has some great virtues: It always works, that is to say it’s 100 percent efficacious, and it never hurts – it’s benign. But it has a drawback, and that’s that it has a poor compliance rate – maybe half of patients who are prescribed it end up using it long-term. There is an alternative, which is a mouthpiece, like an athlete might wear. It goes over the upper and lower teeth, and it’s connected in a way that pulls the jaw forward – we would say protrudes the jaw. It is preferred by patients over CPAP, and it appears to have better compliance; people will use it to a greater extent.
So why is it so underutilized? It’s used in only about 5 percent of all cases. And the reason is that unlike CPAP, which always works, the mouthpiece – we call it an oral appliance – works in let’s say half of all patients. So long-term, the two approaches are about equally effective, and the reason is that long term, the inconsistent effectiveness of the oral appliance therapy is offset by the poor compliance with the CPAP therapy. The challenge for investigators today is finding a means for selecting patients who will be good candidates, who will be therapeutic responders to oral appliance therapy.
I’ve been working on it for ten years. I’m chief medical officer for a company called Zephyr Sleep Technologies, which makes a product called Matrx. We have the only test that can predict whether in fact someone is going to have a therapeutic success with an oral appliance.
The other problem is that in general the dentist is unclear about how much to protrude the jaw in any particular patient. It’s like giving a drug and not knowing the dosage. But the same test that can identify favorable candidates for oral appliance therapy, if a person is a favorable candidate, will also tell the dentist a target efficacious position. So we solve both problems. That’s what Matrx does.
IEEE Pulse: How much of a difference is there between the results you can get in a home-based test, compared to a test in a hospital or sleep lab? Are there both pros and cons for the two methods?
Kushida: Well, there are two basic categories of these home sleep tests, known as Level 3 and Level 2. Level 3 devices are mainly to help diagnose sleep apnea, whereas Level 2 devices are almost like an in-lab study that can be performed at home, meaning that the device can detect brainwave activity and muscle activity, so it’s almost like bringing the in-lab study into the home.
Level 3 studies are not bad for picking up apnea. They are less expensive for the patient, but they are not as sensitive or specific at picking up people with sleep disorders.
Now, the Level 2 devices, those really do measure sleep. Because they measure EEG, which is brain activity; EMG, electromyogram, which is for picking up muscle activity; and EOG, electro-oculogram, which measures eye movements, and without that you can’t really tell when a person’s asleep, you have to rely on what they fill out on the forms, when they turn out the lights, when they turn them on.
Remmers: Home sleep tests are now quite widely used, but not uniformly. They are accurate, in general. They don’t give you all the information that an in-lab polysomnogram can, but in terms of diagnosing sleep apnea, it seems to be in most cases quite adequate, and it’s certainly more convenient, less expensive, and I would say even more relevant, in that you see the patient under fairly normal conditions in the home. So that’s a general trend, and I think that it’s an inevitable trend, that we’ll move that way.
I developed, with my colleagues in Calgary, the first really accurate in home test, and there was huge pushback. Then other tests got done showing not only that it’s accurate, but it gives just as good outcomes as in-lab diagnosis. And so it started gaining momentum. The watershed, we call it an earthquake, happened two years ago in Massachusetts, when some payers said we’re not going to pay for in-hospital testing of sleep apnea.
Now, I’m guessing in Massachusetts probably 80 percent of the tests are done in-home. There are regional variations, it depends on what the local insurance carrier does, so it would vary across the country, but the trend is quite substantial. I would say in five years, diagnosis of garden-variety sleep apnea by lab testing is not going to be done much.
Westbrook: I am biased, because I have invented one of the portable recorders for sleep apnea and the system that uses that.
Probably 90 percent of patients studied now in the laboratory – having to come, having to get hooked up with all this stuff and having a technician watch them sleep all night – can be accurately diagnosed by wearing something at home. Every study that has been done that has been a randomized, validated clinical trial, has shown no difference in outcomes. And that’s now seven to ten major studies in a variety of locations worldwide.
So it’s really quite an exciting time in sleep medicine, diagnosis, and treatment, in that the diagnostic systems due to technology can now be offered to anyone, almost anyplace on the planet, and of course analyzed by experts almost anywhere on the planet through the internet. I’m sitting in a cabin in northern Minnesota and I can analyze overnight recordings from anywhere.
Pack: Most of the systems that are out there don’t actually measure sleep. They’re really there to diagnose sleep apnea – you’re picking up the oxygen drops, you’re picking up the airflow changes, and so on, and you can basically detect the apnea from those things, you can see declines in breathing from an oxygen plot.
The home studies can be very good at establishing what is basically a fairly obvious diagnosis. But if you end up with a negative test, after a high pre-test probability, then you’d probably end up getting a lab test as a follow up. That’s the challenge to the home studies, is they don’t have a very accurate estimation of sleep itself. But for most people, you don’t need that.
Heneghan: One other thing that has been a positive in the home sleep testing, is that a lot of these devices now do two or three night measurements, and sleep apnea can be quite variable from night to night. It’s not really practical to have a person spend three nights in a hospital, so that’s been quite a positive benefit of the home sleep testing.
The other thing people like about it is you’re seeing people in their home environment, so it’s probably a truer reflection of their daily life. When you bring them into the lab, sometimes they might go to bed earlier than they normally do, it’s changing your routine, it’s an unusual environment, you’ve got so many wires so you don’t sleep as well as normal.
IEEE Pulse: What are some of the most promising new directions that you expect to see in sleep diagnostics over the next few years, and what are some areas that are in need of further development?
Kushida: Once we have the diagnosis, the machines are smarter now. We’re starting to see CPAP devices that record not only compliance – how often the patient uses the machine – but that also give us feedback as to how well these devices are treating the apnea. And now these machines are also connected wirelessly, so the feedback on these machines as to how well these devices are treating the patient’s sleep-disordered breathing can be instantaneous.
There’s also sleep endoscopy, to actually characterize the upper airway during sleep, which can help surgeons determine which areas are most amenable to surgery for sleep apnea. There’s 3-D imaging, and there’s also high-density EEG, which is used to more accurately look into the brainwave activity during sleep.
Pack: We need to develop fairly efficient screeners for sleep apnea, whether it’s questionnaire based, or taking pictures of people, looking for risk factors – how heavy you are, your gender, cranio-facial structure from digital pictures, and we can see how you could build that into an app or something and do screening. If you’re out there and you’re the owner of a commercial vehicle company with thousands of drivers, what you want to do is very cost-effective screening. You want to find the people who do need home studies and move in that direction. So I think efficient screeners is an area where you could really see new technology helping.
Remmers: Other new approaches include evaluating the throat air passage by visualizing it, using MRI, or a CT scan, or with an endoscope, putting a fiber-optic scope down the nose. But if you’re going to do any of this, you have to do it while the patient is asleep.
People have shown time and again that you don’t learn anything by imaging the air passage while the patient is awake, because you compensate and always hold it open. Well, there is an approach that’s now coming out, called drug-induced sleep endoscopy, DISE. So you give a drug, knock the person out and simulate sleep. That way you can do an MRI, and look down there and see what you see, and might be able to select patients for appliances or for surgery or for hypoglossal [tongue] electrical stimulation. So we can begin to use imaging, but only when we have the patient knocked out. It’s going to be possible to induce sleep, so that is a distinct possibility, there are a couple of groups working on that, and I think that might be a way to go.
Heneghan: I think one thing we’ll start to see is trying to integrate the diagnostics with electronic health records more. The first home tests were very much standalone devices. But now, there are devices where the diagnostic information is sent to a cloud-based system. So that means the data can then be sucked into your electronic health record, so it’s easier for your primary care physician to have access to it, or for you to have access to it. The data can be more easily shared, so it’s not just in a little silo by itself. That’s going to happen in general with diagnostic testing. I think the other thing we’ll see is that people continue to try to make these devices smaller, and to get rid of wires. People are starting to use Bluetooth so that the effect is you become less and less encumbered by the home sleep testing.
The other area is pediatric sleep apnea. Kids don’t like having things pinned on them, they’re inclined to pull them off. Pediatric studies are difficult to do, so I can see that as being an area of advancement in the next few years as well. Sleep apnea is actually quite common in kids, it’s probably about two percent of children who have some degree of sleep apnea. So it’s common enough that I think it’s a significant problem.
Westbrook: One of the things I see is a better analysis of brainwaves. There will be better recording systems for recording brainwaves that don’t require gluing things to the head. The analysis of those signals will improve. In the future, I think people will be able to wear something that’s relatively comfortable and unobtrusive and we will be able to record them all day and all night for several days and know when they are going about their real business, how alert they are.
I’m 80 years old. I wish that I was a lot younger so that I could see what would come along in the next 25 years. I think it’s going to be an exciting time for technology.