Ma nun me lassà,
Nun darme stu turmiento.
Damme un pacemaker …
Famme campà!
The Gulf of Naples and its surrounding area have served as a beautiful, historic, and romantic attraction for centuries, although the site was seriously damaged by the tragic eruption of Mount Vesuvius in 79 A.D. that led to the destruction of the Roman cities of Pompeii and Herculaneum plus several other nearby settlements. The bay can be looked at as an incomplete and distorted circle-like shape with eight geographical reference points: the Ischia and Procida Islands, the city of Naples, the Vesuvius volcano, the ruins of Pompeii, the cities of Castellammare di Stabia and Sorrento, and the Island of Capri. A map of the bay and surrounding area reveals an interesting irregular and warped trapezoid shape (Figure 1).

“Torna a Surriento” (in English, “Come Back to Sorrento”) became a very popular song [1], along with others of similar sentiment, which were performed often by the best international singers. The song was composed in 1902 by the brothers Ernesto and Giambattista de Curtis; however, even though the listener is led to believe that a hurt lover deeply misses his other half, the true meaning behind the song had a political background and a quite different objective. Disappointing!
Nonetheless, let us revisit the ritornello of this touching canzone in the original Napolitano lyrics:
Ma nun me lassà,
Do not let me down
nun darme stu turmiento!
Do not give me this torment!
Torna a Surriento …
Return to Sorrento …
famme campà!
make me revive!
Now, perhaps, the reader may better understand the modified theme suggested in the epigraph, which could be sung during a pacemaker implantation to cheer up the patient while applying a grain of good humor to the medical act.
Development of Pacemaker Technology
After this somewhat untraditional beginning, let me state the objective of this note: to present some of the milestones of this breakthrough technology across its long and difficult historical development. This is not an exhaustive list, for the literature is extensive. Also, some advances are practically impossible to pinpoint, as the product development was often somewhat lateral, and no one can be really credited as holding full ownership. However, this article is also intended to spotlight some contributors who, for one reason or other, seem to have been left out of the historical narrative. Some designers offered essential ideas, while others came up with less significant contributions; but all belong to a huge pyramid that led to the current situation of this clever little lifesaving gadget—even foreseeing newer advances for a not-too-distant future.
Several publications cover this history with the intent of being as fair as possible, although accounts run the risk of inadvertently omitting information. Several websites also provide good information. A nice overview about cardiac electrical stimulation was collected by David Charles Schechter [2], himself a contributor to the subject, and another by Leslie Alexander Geddes [3]—both going well beyond cardiac pacing that could be better considered as antecedents to actual pacing. Two other articles were produced by Seymour Furman and Amer Chaikhouni, respectively [4], [5]. More specific and informative are very short notes by Furman [6] and Geddes and Bakken [7]. In 1968, Sowton referred to implantable cardiac pacemakers [8]. Greatbatch, back in 1991 in a predecessor of this magazine, published a nice historical summary of the pacemaker [9].
Forgotten Names
There is a name in the history of pacemakers that is, unfortunately, too often forgotten: that of Louise G. Robinovitch, who, more than 100 years ago, produced an external defibrillator that included a pacemaker. She published two papers on the subject, in a journal that was apparently not suited for the topic [10], [11]. She was a controversial Jewish physician of Russian origin who suffered significant discrimination, both because of her gender and her ethnicity. Her doctoral dissertation was rejected in Paris and deemed inadequate. She was a pioneer in American medicine, a graduate of the Women’s Medical College of Pennsylvania in 1889 who continued her studies and research in France during the 1900s.
Robinovitch discovered that pulsed electrical stimuli could be used for cardiac resuscitation, and she designed equipment that was the forerunner of the automatic defibrillator. Moreover, she wrote a series of reports from 1906 through 1909, designed the first portable electrical resuscitative apparatus for ambulances, and produced a kind of external pacemaker device. The significance of these sporadic experimental and clinical reports was not well appreciated at the time because of a lack of understanding regarding ventricular fibrillation. Electric defibrillation was considered impractical, and applications of either cardiac pacing or electrical defibrillation were delayed [12], [23]. In several respects, cardiac pacing is related to and often mixed with defibrillation, as the literature clearly demonstrates [13].
In South America, two names must be rescued and brought to light: those of an electronics engineer, Jorge Reynolds Pombo (1936 to present) [14], and a cardiologist, Orestes Fiandra (1921–2011). The first pacemaker was designed and constructed by Reynolds Pombo in Bogotá, Columbia, and connected to a patient in December 1958; the device was powered by a 12-volt battery and had variable frequency and pulse width [15], [16]. Fiandra, a native of Montevideo, Uruguay, was a professor and researcher in medicine and cardiology. In 1960, he implanted a pacemaker provided by Rune Elmqvist from the Karolinska Institute of Sweden. In 1969, Fiandra founded the company Centro de Construcción de Cardioestimuladores (CCC), or the Cardiostimulators Constructing Center, which was later acquired by Wilson Greatbatch (1919–2011). CCC produced pacemakers until 2009, exporting them to several European countries, Argentina, India, China, and the Dominican Republic [17]. Fiandra’s own words offer support that his was the second implantable pacemaker in the world [18].
A Few Interesting Early Findings

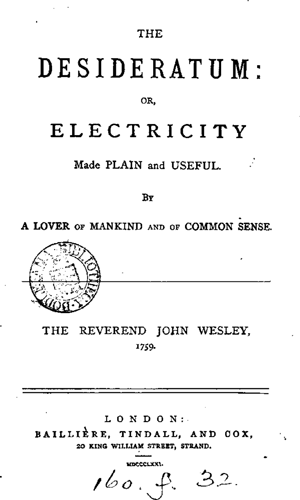
John Wesley (1703–1791) was the 15th child of a clergyman from Epworth in Lincolnshire, England (Figure 2, right). After receiving his bachelor of arts degree, Wesley followed his family’s tradition by taking holy orders, becoming a deacon in Christ Church Cathedral in 1725. He planted the seed of the Methodist Church, and, in 1732, the term Methodists was first coined to describe the group of men meeting in Oxford, as it reflected the method and order of their lives. Wesley was not a scientist or physician but directed his mind to medicine and physics, setting up free clinics that were among the first in England to use electricity for medical purposes. His name is linked to the topic of pacemakers based on a few observations made in his 1759 Desideratum (Figure 3, lower right). Wesley wrote, “I shall endeavour to make it [electricity] useful,” and thus promoted several functions—in particular, that electric pulses accelerate the motion of blood and also quicken the heart by three or four pulses in half a minute. Are we justified in calling this an anticipation of cardiac pacemakers [19], particularly considering that he conducted experiments as well? (It should be noted that Wesley produced another book, published posthumously in 1843, a collection of pseudoscientific observations and health recipes [20].)
In 1882 in Germany, Hugo von Ziemssen (1829–1902) described a case of a 42-year-old woman who had a postoperative defect in the anterior left chest wall. Ziemssen noted that application of electrodes resulted in rhythmic stimulation only if the rate of stimulation was greater than that of the spontaneous heart rate. Slower stimulation produced an erratic and sometimes slower rate.
Back to the 20th Century
In 1926, the Australian anesthesiologist Mark C. Lidwill (1878–1968) devised a portable apparatus in which one pole was applied to a skin pad soaked in a strong salt solution; the other pole, consisting of a needle insulated except at its point, was plunged into the appropriate cardiac chamber. The pacemaker rate was variable, from about 80 to 120 pulses per minute, and likewise the voltage varied from 1.5 to 120 volts. In 1928, the apparatus was used to revive a stillborn infant, whose heart continued to beat of its own accord after the end of ten minutes of stimulation.
In 1932, the American physiologist Albert S. Hyman (1893–1972) described an electromechanical instrument of his own, powered by a spring-wound, hand-cranked motor. Hyman coined the term artificial pacemaker to describe this electric device, which could pace the heart and lead it like an artificial maestro. Publication was delayed, as was application of this research, probably because the work was seen to be interfering with nature by reviving the dead and prolonging life, thus interfering with the will of God. In those days, death was defined as the arrest of cardiac activity and absence of pulse. Hyman did not publish data on pacemaker use in humans because the response, both among his fellow physicians and the press, was so negative. Likewise, Lidwill did not proceed with his experiments in humans. But consider the date—about 85 years ago! It seems hard to believe.
Seventeen years later, in Canada, Wilfred G. Bigelow (1913–2005), John A. Callaghan, and John Hopps used transcutaneous electrodes to pace the right atrium in dogs. During an experimental operation, a dog’s heart suddenly stopped. Recalls Bigelow, “I gave the left ventricle a good poke with a probe I was holding. All the four cardiac chambers responded to it, and further pokes clearly indicated that the heart was beating normally with good blood pressure.” Using dogs and rabbits, Bigelow and Callaghan proceeded with these experiments and presented films on the topic at the Annual Surgical Congress of the American College of Surgeons in 1950.
An external pacemaker, designed and built by the Canadian electrical engineer Hopps (1919–1998), took the form of a large electrical machine that used vacuum-tube technology to provide transcutaneous pacing. Hopps himself later became a pacemaker recipient. As quoted from [5], “Hopps also designed the first catheter electrode for cardiac stimulation, which was introduced via the right external jugular vein of the experimental animal. Using his external pacemaker, atrial pacing was achieved and control of the cardiac rate was accomplished.”
In 1950, Paul Maurice Zoll (1911–1999) began work on an external pacemaker that was used to stimulate the heart across the chest wall. The electrodes consisted of two metal disks placed on the right and left sides of the chest and held in place by a rubber strap making contact via electrode jelly. External pacing was painful and required sedation; prolonged stimulation produced local skin burns. The longest period of reported stimulation was 11 days. Zoll also later developed a bulky external transcutaneous pacemaker operated by rechargeable batteries.
The First Battery-Operated Portable External Pacemaker: 1957
Earl Bakken (1924–present), an electrical engineer, designed the first battery-operated pacemaker. Bakken and his brother-in-law, Palmer Hermundslie, cofounded Medtronic in a Minneapolis garage in 1949. At the time, Clarence Walton Lillehei (1918–1999) was working on the successful repair of a congenital heart defect using cross-circulation and, later, the heart–lung machine. About one patient in ten developed complete heart block postoperatively. It was thought that temporary pacing could keep patients alive until the recovery of the conducting system. The external pacing developed by Zoll was clearly inappropriate, as the high-voltage pacing delivered transcutaneously would be far too traumatic on the young children with whom Lillehei was working.
Lillehei and his coworkers developed a myocardial stainless steel wire in a Teflon sleeve. One end was implanted directly into the myocardium, and the other was connected to a stimulator. An indifferent electrode was placed under the skin to complete the circuit. Because of the direct contact with the myocardium, effective pacing required only 1.5 volts.
As stated in [5], “The first myocardial wire was implanted in 1957, in a three-year old girl in whom heart block had complicated the repair of Fallot’s tetralogy. Pacing was successful and the little girl soon regained sinus rhythm and survived.” Further problems with this pacemaker soon became obvious: the stimulator was large and heavy, and the system depended totally on an external power supply. After experimentation with a transistor circuit, the first battery-powered pacemaker was put into clinical use.
The First Totally Implantable Internal Pacemaker: 1958
In October 1958, the first implantation of a totally internal pacemaker was performed in Sweden. The system was developed by surgeon Ake Senning (1915–2000) and the physician-inventor Rune Elmqvist (1906–1996). It was implanted in a 43-year-old engineer named Arne Larsson, who had been hospitalized with complete heart block and Stokes–Adams attacks. Two electrodes were inserted into the myocardium and tunneled to a pulse generator placed in the abdominal wall. The pulse rate was fixed at a constant rate of 70 to 80 beats per minute. This procedure was reported at the Second International Conference on Medical Electronics in 1959.
Senning was the cardiac surgeon at the Karolinska Hospital in Stockholm, and Elmqvist was a medical graduate who became an engineer. These two men began to collaborate closely in 1950. They discovered the main problem with external pacemakers was the route for ascending infection along the wire, so they set about to design a fully implantable system using silicone transistor technology and a pulse generator powered by two rechargeable nickel–cadmium batteries. Recharging was accomplished transcutaneously using external induction coils for 12 hours every week. The energy need was minimized because Elmqvist used silicon transistors in the circuit. The approximate diameter of the device was 55 millimeters, and it was 16 millimeters thick.
Elmqvist died in 1997, and Senning remained very active in the field of cardiac surgery until his passing in 2000. Larsson, outlived both the engineer and the surgeon. Until his death of cancer at age 86 in 2001, he required five lead systems and 22 pulse generators of 11 different models.
Wilson Greatbatch, a native of Buffalo, New York, was an electrical engineer trying to develop an oscillator to aid in the recording of tachycardia. In late 1959, Greatbatch, together with Dr. William Chardack and Dr. Andrew Gage at the local Veterans Administration Hospital, came up with an implantable device using primary cells as the power source. Tests were run first on a dog. They reported the first success in a human with this unit in June 1960 on a 77-year-old man in complete heart block. The patient survived uneventfully for two years. The device was known as the Chardack–Greatbatch implantable pacemaker (patent number 3,057,356).
In 1961, Chardack, Gage, and Greatbatch reported on a series of 15 patients who had implanted pacemakers. In 1961, Greatbatch licensed his patent to Medtronic. The following year, Parsonnet and Ekstrom developed the technique for inserting permanent transvenous bipolar pacing electrodes. Transvenous leads replaced myocardial leads, which allowed pacemakers and their leads to be implanted without a thoracotomy and without general anesthesia.
Many other improvements ensued, such as follow-up for pacemaker patients by phone. Biventricular pacing for heart failure was introduced and started the revolution of cardiac resynchronization therapy. Chaikhouni states that an “additional lead was introduced via the coronary sinus toward the left ventricle. The right ventricle (via the standard lead) and the left ventricle (via the coronary sinus lead) were paced simultaneously to resynchronize their contraction and improve the symptoms and survival of properly selected heart failure patients” [5].
Discussion and Conclusions
As suggested in the introduction, this article is not intended as a review; rather, it is intended to bring to light some lesser known events and contributors while also recalling the more significant developments originating from several different sources, physicians and engineers alike—once again showing the magnitude and significance of interdisciplinary work. Viewing a subject from different reference points often brings about enlightening ideas.
As stated in Beck et al. [21], it is quite appropriate to repeat that June 2010 marked the 50th anniversary of the first successful human cardiac pacemaker implantation in the United States. On 6 June 1960 in Buffalo, New York, William Chardack implanted a pacemaker— designed and built by Greatbatch—in a 77-year-old man with complete atrioventricular blockage, as noted earlier. This landmark event ushered in a new era of implantable cardiac pacemakers with batteries and leads of high reliability and increasing durability.
Over the past half-century, the field of electrophysiology and implantable devices for the management of cardiac conduction disturbances has evolved dramatically. Today’s pacemakers include increasingly complex features such as telemetry monitoring, autoprogrammability, and hemodynamic sensors. The lithium iodide battery remains the mainstay of implantable pacemaker systems, exhibiting a multiple-year lifespan, slow terminal decay, and a reduced size and production cost. Novel concepts such as leadless and biologic pacing are under active investigation. Greatbatch’s historic achievement 50 years ago thus reminds us that technologic progress is timeless.
Perhaps it is not too out of place that we also remember those who long before, in less recognized ways, also contributed to this remarkable technology. The heart is a marvelous biological design, with a (by far) much longer development; it is ordinarily a long-enduring physiological pump that propels blood. Sometimes, however, it does not accomplish this task properly and needs to be stimulated, as if saying to it, “Come on boy, hurry up”—and, sure enough, pulling hidden strength out, it comes back into action! Pets such as dogs have also benefited from this technology, as veterinarians have taken up the challenge, using the same standards as in humans.
Quite interesting data have also been reported rather recently by Mrinal Kanti Das et al. regarding cardiology and pacemaker use in India [22]. The work of these authors leads to a serious and disturbing question: How many of the world‘s poorest people have access to an affordable cardiac pacemaker, even of the simplest type?
References
- G. Martinelli. Torna a Surriento. [Online].
- D. C. Schechter, Exploring the Origins of Electrical Cardiac Stimulation. Minneapolis, MN: Medtronic, Inc, 1983.
- L. A. Geddes, “A short history of the electrical stimulation of excitable tissue. including electrotherapeutic applications,” Physiol., vol. 27, no. 1, p. 47, 1984.
- S. Furman, “Early history of cardiac pacing and defibrillation,” Indian Pacing Electrophysiol. J., vol. 2, pp. 2–3, 2002.
- A. Chaikhouni, “The magnificent century of cardiothoracic surgery. Part 8: Reviving the dead heart views,” Heart Views, vol. 11, no. 2, pp. 85–91, June–Aug. 2010.
- S. Furman, “In memoriam: Clarence Walton Lillehei (1919–1999),” PACE, vol. 22, pp. 1566, Oct. 1999.
- L. A. Geddes and E. E. Bakken, “Who first performed cardiac pacing: Why, when and where?” IEEE Eng. Med. Biol. Mag., vol. 26, no. 3, pp. 77–79, 2007.
- E. Sowton, “Implantable cardiac pacemakers,” British Heart J., vol. 30, no. 5, pp. 587–590, 1968.
- W. Greatbatch and C. F. Holmes, “History of implantable devices,” IEEE Eng. Med. Biol. Mag., vol. 10, no. 3, pp. 38–41, 1991.
- L. G. Robinovitch, “Resuscitation of electrocuted animals. Choice of the electric current and method used and application to human beings. Experimental study of the respiration and blood pressure during electrocution and resuscitation,” J. Ment. Pathol., vol. 8, no. 2, pp. 74–81, 1907.
- L. G. Robinovitch, “Induction coil specifically constructed according to our indication for purposes of resuscitation of subjects in a condition of apparent death caused by chloroform, morphine, electrocution, etc.,” J. Ment. Pathol., vol. 8, no. 3, pp. 129–145, 1909.
- L. G. Robinovitch, “Electrical analgesia and electric resuscitation after heart failure under chloroform or electrocution,” JAMA, vol. 56, no. 7, 1911, pp. 478–481. [Online].
- M. E. Valentinuzzi, Fibrillation-Defibrillation: Clinical and Engineering Aspects. vol. 6. Singapore: World Scientific, 2010.
- Jorge Reynolds Pombo. Wikipedia. [Online].
- J. Reynolds Pombo, Treinta Años de la Estimulación Cardíaca en Colombia, (in Spanish). Bogotá, Colombia: Editorial Andes, 1988.
- J. Reynolds Pombo, “The early history of cardiac pacing in Colombia,” PACE, vol. 11, no. 3, pp. 355–361, Mar. 1988.
- Orestes Fiandra. Wikipedia. [Online].
- O. Fiandra, “The first pacemaker implanted in America,” PACE, vol. 11, no. 8 pp. 1234–1238, Aug. 1988.
- The desideratum: Or, electricity made plain and useful. [Online].
- J. Wesley, Primitive Physic, or, An Easy and Natural Method of Curing Most Diseases. London: Barr, 1843. [Online].
- H. Beck, W. E. Boden, S. Patibandla, D. Kireyev, V. Gupta, F. Campagna, M. E. Cain, and J. E. Marine, “50th anniversary of the first successful permanent pacemaker implantation in the United States: historical review and future directions,” Amer. J. Cardiol., vol. 106, no. 6, pp. 810–818, Sept. 2010.
- M. Kanti Das, S. Kumar, P. Kumar Deb, and S. Mishra, “History of Cardiology in India,” Indian Heart J., vol. 67, no. 2, pp. 163–169, Mar.–Apr. 2015.
- Saxo. Louise G. Robinovitch. [Online].


