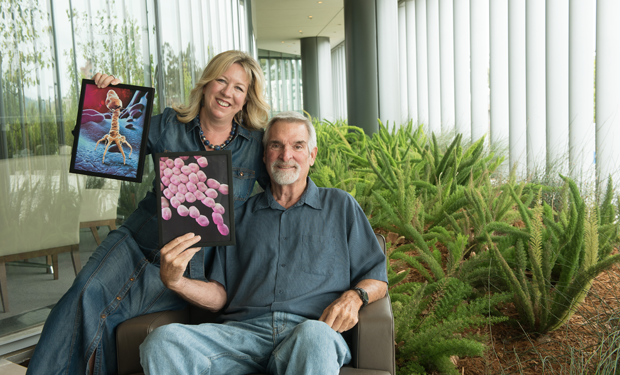
Above: After a grueling battle with a nasty bacterial infection that nearly killed Thomas Patterson (seated), bacteriophage therapy came to the rescue and saved his life. Patterson holds an image of his nemesis, a multidrug-resistant strain of A. baumannii, while his wife Steffanie Strathdee holds up an image of a bacteriophage. Strathdee is an infectious disease epidemiologist at the UCSD School of Medicine and is now the co-director of the university’s newly established Center for Innovative Phage Applications and Therapeutics (IPATH). (Photo courtesy of UCSD.)
Until a dangerous bacterial infection left her husband near death 3 years ago, scientist Steffanie Strathdee had never heard of bacteriophage therapy. After it ultimately saved his life, however, she not only has become a staunch advocate of the therapy, but also now serves as co-director of the newly established Center for Innovative Phage Applications and Therapeutics (IPATH) at the University of California San Diego (UCSD) (above).
Strathdee’s story began when she and her husband Tom Patterson were vacationing in Egypt in November 2015. On the last night of their trip, he became violently ill with severe abdominal pain and vomiting. He was rushed to a Luxor clinic, where he was diagnosed with gallstone pancreatitis, and then sent to Frankfurt, Germany, where doctors discovered that he was infected with a lethal, multidrug-resistant strain of Acinetobacter baumannii. With the infection raging, he was medevaced home to California and hospitalized in Thornton Hospital at UCSD Health. Strathdee and Patterson knew UCSD Health well because both were faculty members in the UCSD School of Medicine—she was an infectious disease epidemiologist and he was a professor of psychiatry.
The UCSD medical team pumped Patterson with full of antibiotics, but to no avail. He slipped into a coma and Strathdee realized that her husband was going to die. Rather than accept the prognosis, she turned to her skills as a researcher and began scouring the scientific literature for alternative strategies to battle superbug infections.
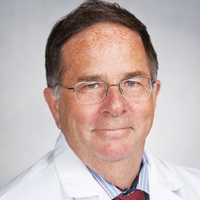
In that pursuit, she came across what she describes as “an obscure paper” extolling the potential virtues of treatment with bacterial viruses called bacteriophages (phages) [1]. She realized that she was grasping at straws by that point, but thought bacteriophage therapy just might have merit. She pitched the idea to the primary physician on the case—Robert “Chip” Schooley, MD, chief of the Division of Infectious Diseases (right)—and he said he was willing to try it, but with two caveats. One was that Strathdee could find phages that matched her husband’s bacterial isolate, and the other that he could get the go-ahead from the U. S. Food and Drug Administration (FDA).
The Hunt for Phages
Strathdee contacted as many U.S. phage researchers studying A. baumannii as she could find and asked for their help. Almost immediately, she heard back from Ry Young, a professor of biochemistry, biophysics, and biology at Texas A&M University. Young asked her to send him the isolate so his team could check it against his own collection of phages, and several hundred environmental samples from sewage and barnyard waste. They found three that matched. He also put out the call for more phages from colleagues worldwide so he could check theirs too. In addition, the San Diego-based biotech company AmpliPhi also donated a bacteriophage that matched Tom’s bacterial isolate.
In the meantime, Schooley contacted FDA officials, who ultimately granted approval to use phage therapy to treat Patterson on a compassionate-use basis. In addition, an official suggested that he and Strathdee get in touch with researchers involved in a large bacteriophage program run by the U.S. Navy. The trail led to two of the biggest names in bacteriophage therapy today—Carl Merril and Biswajit Biswas—and both would play key roles in pulling Patterson back from the brink of death.
A medical doctor with a love for research, Merril had been interested in phages ever since he took the famed Cold Spring Phage Course in 1966 [2]. He eventually became the chief of biochemical genetics in a laboratory at the National Institutes of Health, and until his retirement 43 years later in 2005, he continued to study bacteriophages. He became especially interested in their potential in human medicine. “I knew something that some people don’t know or just don’t pay attention to: if you take a liter of water from anywhere on Earth, whether that’s the Ganges River, the Potomac River, or off the coast of Maine, there’s a billion bacteria in it, and since there are 10²¹ liters of water on the planet, that’s a lot of bacteria,” he says. “And for each of those bacteria, there are approximately 10 bacterial viruses. That makes 10³¹ phages in every liter of water. I thought that if we could develop a rapid way of determining which ones work against a bacterial infection and which ones don’t, we could treat almost any bacterial infection,” he recalled.
To make bacteriophage/phage therapy a reality, he envisioned a quick-response system featuring a large library of phages. In such a system, a clinician could send in a bacterial isolate from a patient, quick-response technology could run the isolate through the precharacterized phage library to find those phages that worked against it, and the effective phages could then be packaged into a personalized treatment that could be shipped out to fight the infection. The technology to create such a system was not yet available by the time Merril retired, but one of his postdoctoral fellows was thinking along similar lines. That was Biswas, who had by then moved on to a different phage research group.
In 2010, Biswas became the senior scientist and phage group team leader in the U.S. Navy Biodefense Directorate at the Naval Medical Research Center (NMRC) at Fort Detrick, MD, USA. The directorate is charged with protecting against attacks, including from bioterrorism. Biswas began inviting his onetime boss to lunch in Maryland to talk about the phage library idea. Merril recounts, “I was retired, so I just did it because it was fun. Every time we met though, more and more people would show up. I didn’t realize they were actually putting the whole thing into practice.”
Creating a phage library
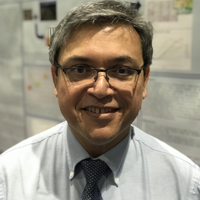
The U.S. Navy directorate was especially interested in A. baumannii, a hard-to-treat bug that often infects wounds of active military serving in the Persian Gulf region. For that reason, it is sometimes called Iraqibacter. “One objective was to develop an alternative therapy to treat this naturally antibiotic-resistant bacterium,” Biswas (right) explains. “We got some Congressional money to fund in-house research, and began looking at therapy using a combination phage, which involved a process I developed here at NMRC that puts together a very specific group of phages which are very effective against a specific bacterium.”
To develop targeted combination phage therapy, Biswas and his research group began harvesting bacterial viruses from sewage, hospital waste, and other human-related sources. “We collected a large number of diverse phages from the environment, and that became our phage library,” he said. To make sure the library contained no unsafe viruses, they had to check each one for deleterious genes, including those that transfer antibiotic resistance from one bacterium to another, confer antibiotic resistance, or are toxic. “A lot of people in different places still don’t believe we can implement this (safety check) at this point, but it is possible,” he asserted. “We can ensure that anything we inject in humans will be devoid of all of these problems.”
Matching the bacteriophages to the bacteria was another challenge. Here, Biswas’s group developed a robotic system that very rapidly distributes phages into multiwelled plates that contain a growth medium and tetrazolium dye. “Then we infect those hundreds of wells with a specific bacterium that has been isolated from the patient’s body, and incubate them at 37 degrees Centigrade in a system developed by the company Biolog (of Hayward, CA, USA),” Biswas describes. If the phages aren’t effective, the bacteria grow, respire, and reduce the tetrazolium dye, converting them from colorless molecules to bright-red molecules. The Biolog system features a camera that takes a picture of each well and picks up any red, therefore reporting the success of the different phages. From start to finish, the screening process takes 18 hours, which is the time it takes for the bacterium to grow on the plates. The system can check 5,000 wells at a time.
To test the system’s effectiveness, the researchers made targeted cocktails and tried them out on bacterial infections in animal models. They worked. The researchers also demonstrated that the approach could yield new phage combinations if the bacteria became resistant to the initial cocktail, Biswas notes. “It was during this time in 2015–2016 that we learned that a patient at UCSD had a multiple-drug-resistant Acinetobacter infection, and the doctors there were looking for alternate therapies.” The patient was Patterson, who by then had been hospitalized for more than 3 months.
Taking it to Humans
Biswas’s group put their process in action and quickly found ten phages that were active against Patterson’s infection. They selected four of the most virulent and shipped them to UCSD in March 2016. Merril was involved in the treatment by that point. “He convinced us that we really needed to administer the phages intravenously because my husband was fully colonized,” Strathdee recounts. “He said that other phage trials in the past have failed largely because of under-dosing, and if you administer this topically or through an abdominal catheter, you might miss hidden reservoirs (of bacteria), so you’re actually giving the bacteria a leg up to become resistant, and all this phage therapy will be for naught.”
Then they all waited, but fortunately not for long. Having already started to receive the Texas phage cocktail a few days before, Patterson came out of the coma just 3 days after getting the Navy phage strains that were selected using the Biolog system for his specific infecting A. baumannii organism [3], [4]. “He was so close to death, in a coma for two months and entering multi-system organ failure. Almost everybody thought he was a goner, and then he woke up. It was just a dramatic turnaround,” Strathdee says. Some resistance did develop, but the Navy team identified one more phage directly from sewage water that was active against both the initial bacteria and the mutated bacteria. When combined with one of the original phages and an antibiotic, the adjusted cocktail ultimately eliminated Patterson’s infection for good. Within less than 2 weeks, Patterson was off all life support.
“As it turns out, he was the first person to receive intravenous phage therapy in the United States to treat a systemic bacterial infection that was multi-drug resistant,” Strathdee reports.
With her husband on the mend, Strathdee realized that bacteriophage therapy was something that could and should be explored further. “From the moment that this case was presented by Dr. Biswas at the Pasteur Institute at the 100th anniversary of the discovery of bacteriophage in 2017 [5], we started getting calls from all over the world and so did Dr. Schooley. We all thought, it’s one thing to continue offering these compassionate-use therapy cases, but what we really need to do is move to clinical trials.”
Going Viral
Since UCSD already had the infrastructure in place to do multisite clinical trials, Strathdee and Schooley spearheaded the June 2018 establishment of the IPATH bacteriophage center at the university. The first of its kind in North America, IPATH combines expertise from 20 researchers and clinicians at UCSD, plus scientists at national research institutions and private industry to push the research forward and begin clinical trials. Those trials, which they hope will begin in 2019, will focus first on infections facing cystic fibrosis patients, Strathdee says (above).
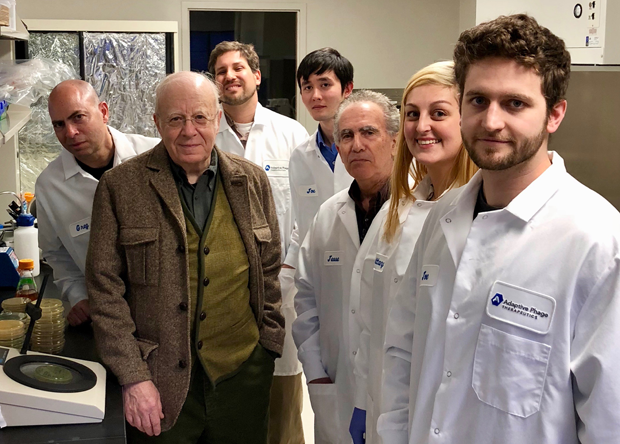
Among the center’s private collaborators is Adaptive Phage Therapeutics (APT), which Merril and his son founded in 2016 at the urging of Biswas and others in the NMRC. “Basically, the Navy needed a commercial partner who understood what they were trying to do, which is individualized therapy. After they advertised and had nobody really compete, they asked me to stop being retired and to start up a business to collaborate with them,” Merril says. Based in Gaithersburg, MD, USA, APT is drawing on the NMRC’s phage library and screening technology to develop new bacteriophage therapies and run clinical trials.

Instead of seeking FDA approval for bacteriophage therapies one infection at a time, which would be too time-consuming and expensive, Merril hopes the FDA will grant a license for the entire concept. This includes the phage library, in which all phages are totally genomically characterized and screened against toxin and antibiotic resistance gene databases to assure that they have no deleterious genes. In addition, these phages will have to be purified and pass rigorous testing for bacterial cell contaminates and infectious microbes to provide for the production of personalized phage therapies, he states. “Once that happens, I think the pharmaceutical industry will see the light and begin to invest. In fact, we’re already negotiating with some of the big pharmaceutical companies,” he says. “There’s a lot of enthusiasm there now, and there wasn’t just a couple of years ago.”
On the medical-care side, UCSD doctors have already treated a handful of other patients with multi-drug resistant bacterial infections, including those who have cystic fibrosis or who have had organ transplants or implanted hardware devices. In addition, APT is currently working with about three dozen patients who have resistant infections. Through IPATH, Strathdee is also trying to spread the word. “We want to disseminate the information we learned so other patients who have these antibiotic-resistant infections won’t have to die without hope.” She and Patterson are publishing a book on their story in spring 2019. The title is The Perfect Predator: A Scientist’s Race to Save Her Husband from a Deadly Superbug.

As for her own husband, Strathdee says with a smile, “He’s awesome. He’s been back at work for more than a year, and it hasn’t held us back from having a normal, productive life.” She adds, “I just feel really lucky. We found the right people at the right time, and we had the right technology. I’m looking forward to seeing what bacteriophage therapy holds for the future.”
References
- C. R. Merril, D. Scholl, and S. L. Adhya, “The prospect for bacteriophage therapy in Western medicine,” Nature Rev., vol. 2, pp. 489–497, June 2003.
- M. Susman, “The Cold Spring Harbor phage course (1945–1970): A 50th anniversary remembrance,” Genetics, vol. 139, no. 3, pp. 1101–1106, April 1995. Accessed: October 29, 2018. [Online].
- R. T. Schooley et al., “Development and use of personalized bacteriophage-based therapeutic cocktails to treat a patient with a disseminated resistant Acinetobacter baumannii infection,” Antimicrob. Agents Chemother., vol. 61, no. 10, pp. e00954–17, 22 Sept. 2017.
- S. Strathdee and T. Patterson, The Perfect Predator: A Scientist’s Race to Save Her Husband from a Deadly Superbug: A Memoir, New York, NY, USA: Hachette Books, 2019.
- “Centennial Celebration of Bacteriophage Research,” Institut Pasteur. [Online].