Recent breakthroughs in science and technology have produced prosthetic hands, arms, and legs that increasingly resemble biological ones
Despite remarkable advances in the field of prosthetic limbs, existing products still aren’t meeting the needs of patients. A 2022 survey found that 44% of upper-limb amputees abandoned their prostheses, citing discomfort, heaviness of the device, and problems with functionality [1].
Researchers and product developers are hard at work to change that, developing a new generation of bionic limbs, which are robotic prosthetics that are controlled by signals from users. For people who have lost body parts to trauma, disease, or congenital defects, bionic limbs hold the power to restore a high degree of independence. Pioneering new surgeries, life-like materials, and touch feedback for users are some of the key innovations fueling that progress.
Making the artificial more biological
Several key technological advances have set the stage for prosthetic limbs that are more responsive, resilient, and user-friendly than their predecessors. Improvements in the primary components of robotic limbs, including microcontrollers, motors, transmission systems, batteries, artificial intelligence (AI), and machine learning have occurred in tandem over the past decade, catapulting research in the field to new heights.
Another boon for the field: 3-D printing. PSYONIC, a bionic technology company based in San Diego, has leveraged the relatively inexpensive technique to build its Ability Hand, the fastest hand on the market, but also one of the lightest and most resilient (Figure 1). Rather than using rigid materials common in the field of prosthetics—such as injection-molded plastics and custom machine steel—PSYONIC’s hand is built with soft robotics materials, including silicone and rubber, that more closely resemble human hands [2].
“The number one complaint we heard from patients and clinicians was that their expensive prosthetics would break easily,” said Aadeel Akhtar, Ph.D., PSYONIC’s founder and CEO. “In contrast, our own fingers are flexible and compliant, which is what makes them so impact-resistant and robust.” The Ability Hand1 has survived a range of durability tests, including punching through flaming wooden boards, breaking ice blocks, falling 30 feet, and tumbling around in a dryer for 10 minutes.
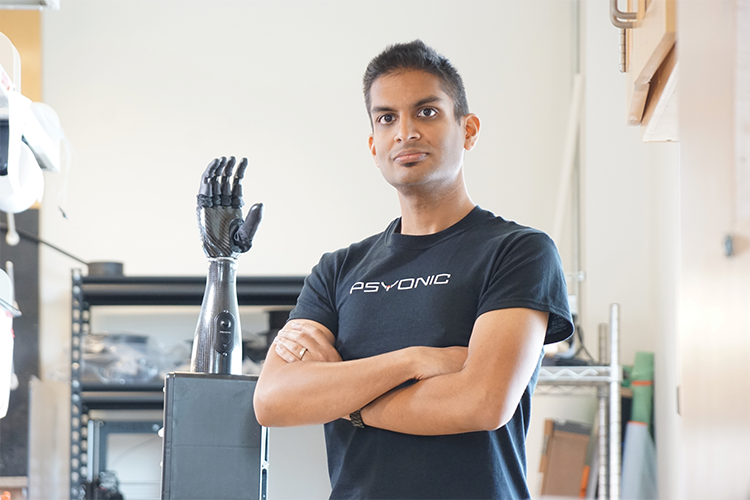
Figure 1. PSYONIC’s CEO and Founder, Aadeel Akhtar, Ph.D., with the Ability Hand1. (Photo courtesy of PSYONIC.)
It’s the first hand on the market to give users touch feedback, via six sensors on each finger (one each on the finger pad and tip; four on the shaft). When a sensor makes contact with another object, it transmits a subtle vibration to the user’s residual limb. The firmer the contact, the stronger the vibration (Figure 2).

Figure 2. Tina Brockett uses the Ability Hand1, which provides touch feedback to users via six touch sensors on each finger. (Photo courtesy of PSYONIC.)
Mechanical advances have also bolstered lower-limb prosthetics. The Utah Bionic Leg, funded by the German prosthetics firm Ottobock, is about half the weight of any existing robotic leg prosthesis [3]. That can make a big difference for users, because adding weight to a prosthesis makes walking harder, interferes with balance, and can destabilize the interface between the user’s body and the device, said Tommaso Lenzi, Ph.D., an associate professor of mechanical engineering at the University of Utah. “Weight has been one of the biggest issues in translating robotic leg prostheses from the lab to the real world,” he said.

Figure 3. Utah Bionic Leg. (Photo courtesy of Christoph Neumann and Sascha Boldt | Ottobock.)
Lenzi and his team have used insights from human biology to refine the Utah Bionic Leg, which has been under development for more than five years. They substituted stiff actuators, common in robotics, for more compliant materials such as springs and dampers, allowing the bionic leg to rely on gravity and inertia the same way a biological leg does. They have effectively created a variable transmission system, allowing users to seamlessly “shift gears” when they need more torque or speed (Figure 3).
The Utah Bionic Leg also relies on the physical properties of biological movement to provide virtually endless battery life for its users. If the battery approaches empty, the device enters a low-power mode, harnessing the energy generated by the user to continue operating. (Because walking on level ground is a net-zero energy task, the energy spent during the acceleration phase of each step is essentially equal to the energy recovered during the deceleration phase.)
Endless battery life is hugely important to the user, affording the freedom to walk without the fear of being stranded. But challenges still remain: namely, handling the unpredictability of the world outside the lab. Lenzi and his colleagues are exploring several approaches to adapting bionics to work in unstructured environments, including an AI and machine learning system that learns about a user’s environment and a neural engineering approach that gives more volitional control to the user.
“Every person walks differently. Every staircase is different. Every chair is different,” Lenzi said. “Dealing with all of the real world’s variability—while giving users a device that’s functional and safe—is a big open challenge.”
Problem of control
The other major question facing prosthetics researchers is how to give users an intuitive way to operate a robotic body part. “A central challenge with bionic limbs is the problem of control,” said Thomas Roberts, Ph.D., a professor of biology and vice chair of the Department of Ecology, Evolution, and Organismal Biology at Brown University. “One of the goals is to come up with a way to measure user intent—essentially a way for a user, without holding some sort of remote, to control various aspects of their prosthetic device.”
The most common existing method for measuring user intent—attaching electrodes to the skin atop remaining muscles near the amputation site—often provides an unreliable signal due to sweat and the movement of electrodes. Many believe that electrodes implanted in the nervous system will be the next big frontier for the field of bionics. At PSYONIC, Akhtar and his colleagues are using Google’s TensorFlow platform to create an algorithm that trains a bionic hand to act like a biological one using implanted electrodes. By recording movements from a user’s remaining hand, they can then leverage the data they collect to train nerve implants on the other side of the body.
PSYONIC is also developing a technique that will enable surgeons to directly anchor a bionic finger to a patient’s residual bone. A titanium implant connects the device to the bone, while an artificial tendon sutured onto a residual tendon allows the user to control the prosthetic finger with their own muscle. Other groups are also working to develop and refine surgical techniques that enhance user control. Hugh Herr, Ph.D., of the Massachusetts Institute of Technology (MIT), and Matthew Carty, M.D., of Brigham Young University, pioneered a technique known as agonist–antagonist myoneural interface, which sutures two opposing muscles to a device to control a prosthetic joint the same way the body operates a healthy one [4].
Roberts and his collaborators, including Herr, Carty, and MIT’s Cameron Taylor, Ph.D., are exploring another innovative way to measure user intent: magnets that detect changes in muscle length. The researchers implanted two spherical magnets along the length of a muscle and used an array of magnetometers to extract data on the distance between the two magnets. When a muscle contracts or a joint changes position, the magnets move in a predictable way. That signal can then be fed through a control algorithm to operate a linked robotic device. Initial tests in animal models show that the magnets accurately measure the changing length of muscles during running, jumping, and other movements [5] and that the implants do not cause inflammation or other problems [6].
Implants can also provide users with sensory feedback, including touch and proprioception, that makes it much easier to operate a robotic limb. At the University of Pittsburgh’s Rehab Neural Engineering Labs, Lee Fisher, Ph.D., and his colleagues stimulated the spinal cord of amputees using implanted electrodes. That stimulation helped restore sensation from a missing foot and improved balance and stability while walking with a prosthetic [7].
As engineers continue to study the most effective methods for controlling robotic limbs, other researchers are exploring how the brain and nervous system adapt to bionic devices [8]. At the University of Cambridge, Tamar Makin, Ph.D. is conducting research to answer questions such as: What conditions enable a person to experience an artificial limb as part of their own body? For example, does a prosthetic limb need to look like a real one? And how does the brain change after using a bionic limb?

Figure 4. Tommaso Lenzi, Ph.D., works with a participant to test the Utah Bionic Leg. (Photo courtesy of HGN Lab for Bionic Engineering.)
Democratizing bionic limbs
Engineers tend to focus on improving function—making a prosthetic more powerful, faster, or precise, for example—but users often care more about a device’s intuitiveness, Lenzi said. People want artificial hands, arms, and legs that are under their control and feel like part of their own body. “One thing that’s going to become increasingly important is how much we’re including end-users in our research,” Lenzi adds (Figure 4). In the past, engineers might work on a prosthetic device for years in the lab before testing it with end-users. “Now, I have amputees coming in and out of my lab pretty much every day, and they’re involved very early on with everything we do,” he said. “It’s a fantastic change that is really helping the field progress.”
At the other end of the pipeline, companies like PSYONIC are also prioritizing patient engagement. The PSYONIC Institute, a nonprofit subsidiary of the company, collects donations to subsidize the cost of the Ability Hand1 for uninsured U.S. patients and people in other countries. Akhtar is also in the midst of an equity crowdfunding campaign that has allowed patients and other members of the public to invest in PSYONIC.
“That’s also part of the future of where the field is heading: democratizing bionics and making them even more accessible, but also making the companies accessible as well,” he said.
References
- S. Salminger et al., “Current rates of prosthetic usage in upper-limb amputees—Have innovations had an impact on device acceptance?” Disability Rehabil., vol. 44, no. 14, pp. 3708–3713, Jul. 2022, doi: 10.1080/09638288.2020.1866684.
- A. Akhtar, “3D-printing hands that feel,” GetMobile, Mobile Comput. Commun., vol. 24, no. 4, pp. 10–16, Mar. 2021, doi: 10.1145/3457356.3457360.
- M. Tran et al., “A lightweight robotic leg prosthesis replicating the biomechanics of the knee, ankle, and toe joint,” Sci. Robot., vol. 7, no. 72, Nov. 2022, Art. no. eabo3996, doi: 10.1126/scirobotics.abo3996.
- M. Hutson, “This new surgical procedure could lead to lifelike prosthetic limbs,” Science, May 2017, doi: 10.1126/science.aan6912.
- C. R. Taylor et al., “Untethered muscle tracking using magnetomicrometry,” Frontiers Bioeng. Biotechnol., vol. 10, p. 1979, Oct. 2022, doi: 10.3389/fbioe.2022.1010275.
- C. R. Taylor et al., “Clinical viability of magnetic bead implants in muscle,” Frontiers Bioeng. Biotechnol., vol. 10, Oct. 2022, Art. no. 1010276, doi: 10.3389/fbioe.2022.1010276.
- A. C. Nanivadekar et al., “Spinal cord stimulation restores sensation, improves function, and reduces phantom limb pain after transtibial amputation,” medRxiv, Sep. 2022, doi: 10.1101/2022.09.15.22279956.
- E. Amoruso et al., “Intrinsic somatosensory feedback supports motor control and learning to operate artificial body parts,” J. Neural Eng., vol. 19, no. 1, Jan. 2022, Art. no. 016006, doi: 10.1088/1741-2552/ac47d9.



