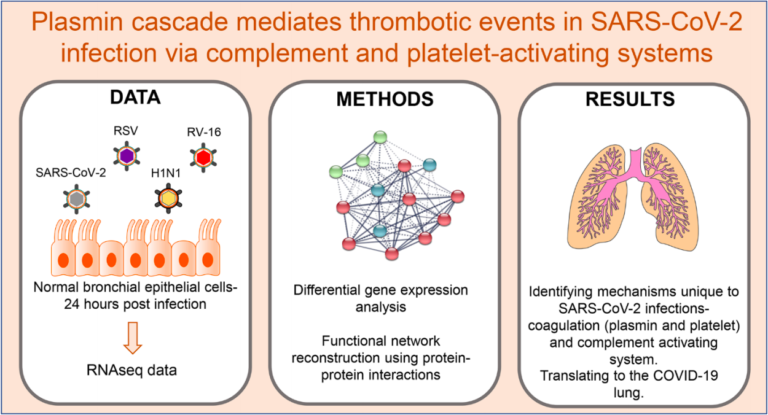
Recently emerged beta-coronavirus SARS-CoV-2, has resulted in the current pandemic designated COVID-19. COVID-19 manifests as severe illness exhibiting systemic inflammatory response syndrome, acute respiratory distress syndrome (ARDS), thrombotic events, and shock, exacerbated further by co-morbidities and age. Recent clinical evidence suggests that the development of ARDS and subsequent pulmonary failure result from a complex interplay between cell types (endothelial, epithelial and immune) within the lung promoting inflammatory infiltration and a pro-coagulative state. How the complex molecular events mediated by SARS-CoV-2 in infected lung epithelial cells lead to thrombosis and pulmonary failure, is yet to be fully understood. We address these questions here, using publicly available transcriptomic data in the context of lung epithelia affected by SARS-CoV-2 and other respiratory infections, in vitro. We then extend our results to the understanding of in vivo lung, using a publicly available COVID-19 lung transcriptomic study. Our analysis indicates that there exists a complex interplay between the fibrinolytic system particularly plasmin, and the complement and platelet-activating systems upon SARS-CoV-2 infection, with a potential for therapeutic intervention.