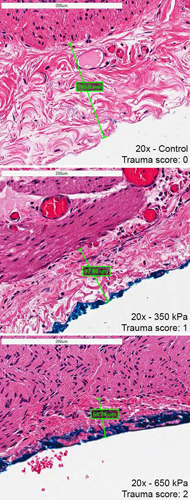
Excessive magnitudes of compressive stress exerted on gastrointestinal tissues can lead to pathological scar tissue or adhesion formation, bleeding, inflammation or even death from bowel perforation and sepsis. It is currently unknown however, at exactly what magnitude of compressive stress that these pathologies occur. A novel simple compressive device was engineered to provide an objective means of producing discrete compressive stresses on human tissues. Samples of human large intestine (colon) were removed from consenting patients as a part of their standard surgical procedure. These samples were compressed with a range of loads normally produced by standard laparoscopic graspers in representative abdominal surgeries. After compression, specimens were processed for histological analysis and assessed. The two independent pathologists who were blinded to stress magnitudes were both able to quantify increasing tissue damage that corresponded to increasing amounts of compressive force. A threshold between 350–450 kPa was discovered that corresponded to both significant serosal thickness change and a positive histological trauma score rating. Whether the tissue injury quantified is pathologic is subject for future in-vivo longitudinal investigation but certainly based on literature, can be the basis of pathological adhesion formation or an area for hemorrhage and scar formation.